Abstract
Objective
Sighing is a common symptom in children and adolescents. In this study, we explored the clinical characteristics and hemodynamic responses to head-up tilt test (HUTT) in children and adolescents with unexplained sighing.
Methods
One hundred ninety-two children and adolescents complaining of unexplained sighing were enrolled as study group after excluding chest wall, lung, heart diseases, and psychogenic disorders. Sixty-nine healthy individuals were enrolled as control group. All the subjects underwent HUTT.
Results
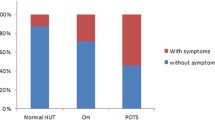
Nitroglycerin-stimulated HUTT positive rate was higher in the study group than the control group (24.0% vs 10.1%, P = 0.014). In total, 32.3% of patients with sighing had positive responses to HUTT, which was higher than that of healthy individuals (32.3% vs 15.9%, P = 0.009). Among 62 cases with positive responses to HUTT in the study group, 48 cases were vasoinhibitory type vasovagal syncope (VVS), 5 cases were mixed type VVS, 3 cases were cardioinhibitory type VVS, 5 cases were postural tachycardia syndrome, and one case was orthostatic hypertension. Sighing patients with positive responses to HUTT had female dominance (54.8% vs39.2%, P = 0.045), older mean age (9.6 ± 2.8 vs 8.1 ± 2.7 years old, P = 0.001), higher basic systolic blood pressure (104.8 ± 10.4 vs 101.1 ± 9.9 mmHg, P = 0.019), and higher diastolic blood pressure (66.0 ± 7.5 vs 62.9 ± 9.2 mmHg, P = 0.021) compared with those of negative responses.
Conclusions
Nearly one-third of children and adolescents with unexplained sighing had positive responses to HUTT, demonstrating that sighing was related to dysfunction of the autonomic nervous system. Elder female patients with higher systolic and diastolic blood pressure were more likely to have positive responses to HUTT.

Similar content being viewed by others
References
Vlemincx E, Van Diest I, Van den Bergh O (2015) Emotion, sighing, and respiratory variability. Psychophysiology 52(5):657–666
Li P, Yackle K (2017) Sighing. Curr Biol 27(3):R88–R89
Boulding R, Stacey R, Niven R, Fowler SJ (2016) Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev 25(141):287–294
Vlemincx E, Van Diest I, Van den Bergh O (2016) A sigh of relief or a sigh to relieve: the psychological and physiological relief effect of deep breaths. Physiol Behav 165:127–135
de Groot EP, Duiverman EJ, Brand PL (2013) Dysfunctional breathing in children with asthma: a rare but relevant comorbidity. Eur Respir J 41(5):1068–1073
Ramirez JM (2014) The integrative role of the sigh in psychology, physiology, pathology, and neurobiology. Prog Brain Res 209:91–129
Brisinda D, Brocca L, Sorbo AR, Lombardi G, Fioravanti F, Fenici R (2018) Psychophysiological evaluation of patients with transient consciousness loss of uncertain origin. Kardiol Pol 76(3):566–573
Olivola E, Brusa L, Rocchi C, Schillaci O, Liguori C, Cerroni R, Pierantozzi M, Chiaravalloti A, Stefani A, Stocchi F (2018) Does fatigue in Parkinson's disease correlate with autonomic nervous system dysfunction? Neurol Sci 39(12):2169–2174
Zou R, Wang S, Zhu L, Wu L, Lin P, Li F, Xie Z, Li X, Wang C (2017) Calgary score and modified Calgary score in the differential diagnosis between neurally mediated syncope and epilepsy in children. Neurol Sci 38(1):143–149
Wang C, Li Y, Liao Y, Tian H, Huang M, Dong X, Shi L, Sun J, Jin H, Du J (2018) 2018 Chinese pediatric cardiology society (CPCS) guideline for diagnosis and treatment of syncope in children and adolescents. Sci Bull 63(23):1558–1564
Connett GJ, Thomas M (2018) Dysfunctional breathing in children and adults with asthma. Front Pediatr 6:406
Orengul AC, Ertas E, Ustabas Kahraman F, Yazan H, Cakir E, Nursoy MA (2020) Psychiatric comorbidity in children with psychogenic and functional breathing disorders. Pediatr Pulmonol 55(2):462–467
Udani V, Bavdekar M, Karia S (2004) Head up tilt test in the diagnosis of neurocardiogenic syncope in childhood and adolescence. Neurol India 52(2):185–187
Gourishankar A, Belton MD, Hashmi SS, Butler IJ, Lankford JE, Numan MT (2020) Demographic and clinical features of pediatric patients with orthostatic intolerance and an abnormal head-up tilt table test; a retrospective descriptive study. Pediatr Neonatol 61(1):68–74
Mulkey SB, du Plessis AJ (2019) Autonomic nervous system development and its impact on neuropsychiatric outcome. Pediatr Res 85(2):120–126
Wong KS, Chiu CY, Huang YH, Huang LJ (2009) Plethysmographic lung volumes in children with sighing dyspnea. Pediatr Int 51(3):405–408
Prabhu MA, Pillai V, Shenthar J (2017) Comparison of efficacy, pattern of response, occurrence of arrhythmias, and the tolerability of nitroglycerine and iIsoprenaline as provocative drugs during head-up tilt test. Heart Lung Circ 26(6):586–592
Deveau AP, Sheldon R, Maxey C, Ritchie D, Doucette S, Parkash R (2020) Sex differences in vasovagal syncope: a post hoc analysis of the prevention of syncope trials (POST) I and II. Can J Cardiol 36(1):79–83
Coupal KE, Heeney ND, Hockin BCD, Ronsley R, Armstrong K, Sanatani S, Claydon VE (2019) Pubertal hormonal changes and the autonomic nervous system: potential role in pediatric orthostatic intolerance. Front Neurosci 13:1197
Onishi Y, Minoura Y, Chiba Y, Onuki T, Ito H, Adachi T, Asano T, Kobayashi Y (2015) Daily dysfunction of autonomic regulation based on ambulatory blood pressure monitoring in patients with neurally mediated reflex syncope. Pacing Clin Electrophysiol 38(8):997–1004
Funding
This work is supported by grants from the Natural Science Foundation of Hunan Province in China (2018JJ3730) and Health and Family Planning Commission of Hunan Province (20201217).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research was approved by the Medical Ethical Committee at The Second Xiangya Hospital, Central South University.
Informed consent statements
All included patients or their guardians signed informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zou, R., Wang, S., Li, F. et al. Clinical characteristics and hemodynamic responses to head-up tilt test in children and adolescents with unexplained sighing. Neurol Sci 42, 3343–3347 (2021). https://doi.org/10.1007/s10072-020-04956-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04956-8