Abstract
Background
One of the hypothalamus-pituitary axis hormones which may play a crucial role in pathophysiology of migraine is prolactin which is secreted from anterior pituitary gland and synthesized by various immune system cells as well. Whether prolactin blood levels can affect the migraine pathogenesis is an open question. Therefore, investigating prolactin circulatory levels in migraineurs may pave the way to underpin the mechanisms of migraine pathophysiology at biochemical levels. In the current investigation, the prolactin blood levels in the migraine subjects were investigated using systematic review and meta-analysis.
Methods
Using online and specialized biomedical databases including Google Scholar, Medline, Pubmed, Pubmed Central, Embase, and Scopus, without the beginning date restriction until Feb 2019, the systematic review retrieved 11 publications in this systematic review after fulfilling for the inclusion and exclusion criteria. For heterogeneity, extent calculation statistical testing was applied. In the present study, the levels of circulatory prolactin in migraineurs assessed using standardized mean difference (SMD) as the effect size.
Results
Q quantity and I2% statistic index showed a high heterogeneity in the 13 selected publications (188.370 and 92.568, respectively) and random-effects model was chosen for further analyses. The meta-analysis on a total number of 460 migraineurs and 429 healthy controls found that the weighted pooled SMD for the effects of prolactin blood concentrations on migraine pathogenesis was as follows: SMD = 1.435 (95% confidence interval, 0.854–2.015).
Conclusion
The current investigation presents evidence that prolactin blood levels are higher in migraineurs than healthy subjects.



Similar content being viewed by others
References
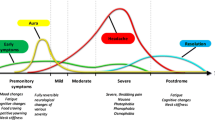
Cuvellier J-C (2019) Pediatric vs. adult prodrome and postdrome: a window on migraine pathophysiology? Front Neurol 10:199
Ambrosini A (2018) Neurophysiology of migraine. Neurol Sci 39(1):59–60
Hoffmann J, Baca SM, Akerman S (2019) Neurovascular mechanisms of migraine and cluster headache. Journal of cerebral blood flow and metabolism : official journal of the International Society of Cerebral Blood Flow and Metabolism 39(4):573–594
Giani L, Corno S, Laganà MM, Baglio F, Lovati C (2019) Cerebral venous outflow in migraine. Neurol Sci 40(1):181–182
Guidetti V, Cerutti R, Faedda N, Natalucci G (2019) Migraine in childhood: an organic, biobehavioral, or psychosomatic disorder? Neurol Sci 40(1):93–98
Grazzi L, D’Amico D (2019) Chronic migraine and medication overuse: which strategy for a complex scenario. Neurol Sci 40(1):175–176
Pavlovic JM, Akcali D, Bolay H, Bernstein C, Maleki N (2017) Sex-related influences in migraine. J Neurosci Res 95(1–2):587–593
Allais G, Chiarle G, Sinigaglia S, Airola G, Schiapparelli P, Bergandi F, Benedetto C (2019) Acupuncture treatment of migraine, nausea, and vomiting in pregnancy. Neurol Sci 40(1):213–215
Freeman ME, Kanyicska B, Lerant A, Nagy G (2000) Prolactin: structure, function, and regulation of secretion. Physiol Rev 80(4):1523–1631
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Faraone SV (2008) Interpreting estimates of treatment effects: implications for managed care. P T 33(12):700–711
Cassidy EM, Tomkins E, Dinan T, Hardiman O, O'Keane V (2003) Central 5-HT receptor hypersensitivity in migraine without aura. Cephalalgia 23(1):29–34
Cassidy EM, Tomkins E, Sharifi N, Dinan T, Hardiman O, O'Keane V (2003) Differing central amine receptor sensitivity in different migraine subtypes? A neuroendocrine study using buspirone. Pain 101(3):283–290
Fava A, Pirritano D, Consoli D, Plastino M, Casalinuovo F, Cristofaro S, Colica C, Ermio C, De Bartolo M, Opipari C, Lanzo R, Consoli A, Bosco D (2014) Chronic migraine in women is associated with insulin resistance: a cross-sectional study. Eur J Neurol 21(2):267–272
Peres MF, Sanchez del Rio M, Seabra ML, Tufik S, Abucham J, Cipolla-Neto J, Silberstein SD, Zukerman E (2001) Hypothalamic involvement in chronic migraine. J Neurol Neurosurg Psychiatry 71(6):747–751
Parashar R, Bhalla P, Rai N K, Pakhare A, Babbar R (2014) Migraine: is it related to hormonal disturbances or stress? International journal of women's health 6:921–5
Guldiken S, Guldiken B, Demir M, Kabayel L, Ozkan H, Turgut N, Hunkar R, Kat S (2011) Soluble CD40 ligand and prolactin levels in migraine patients during interictal period. J Headache Pain 12(3):355–360
Solmaz V, Ceviz A, Aksoy D, Cevik B, Kurt S, Gencten Y, Erdemir F (2016) Sexual dysfunction in women with migraine and tension-type headaches. Int J Impot Res 28(6):201–204
Dogan VB, Dagdeviren H, Dirican A, Dirican AC, Tutar NK, Yayla VA, Cengiz H (2017) Hormonal effect on the relationship between migraine and female sexual dysfunction. Neurol Sci 38(9):1651–1655
Awaki E, Takeshima T, Takahashi K (1989) A neuroendocrinological study in female migraineurs: prolactin and thyroid stimulating hormone responses. Cephalalgia 9(3):187–193
D'Andrea G, Cananzi AR, Grigoletto F, Meneghini F, Cortesi S, Soffiati G, Joseph R, Nordera G, Ferro-Milone F (1988) The effect of dopamine receptor agonists on prolactin secretion in childhood migraine. Headache 28(5):354–359
Gavaghan DJ, Moore RA, McQuay HJ (2000) An evaluation of homogeneity tests in meta-analyses in pain using simulations of individual patient data. Pain 85(3):415–424
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Sabharwal P, Glaser R, Lafuse W, Varma S, Liu Q, Arkins S, Kooijman R, Kutz L, Kelley KW, Malarkey WB (1992) Prolactin synthesized and secreted by human peripheral blood mononuclear cells: an autocrine growth factor for lymphoproliferation. Proc Natl Acad Sci U S A 89(16):7713–7716
Kiefer KA, Malarkey WB (1978) Size heterogeneity of human prolactin in CSF and serum: experimental conditions that alter gel filtration patterns. J Clin Endocrinol Metab 46(1):119–124
Teive HAG, Munhoz RP, Camargo CHF, Walusinski O (2018) Yawning in neurology: a review. Arq Neuropsiquiatr 76(7):473–480
Güven B, Güven H, Çomoğlu SS (2018) Migraine and yawning. Headache 58(2):210–216
Granata R, Sabine E, Tilg H, Wenning G (2017) Gastrointestinal dysfunction, Bedside approach to autonomic disorders. Springer, pp 101–116
Bussone G, Usai S, Moschiano F (2012) How to investigate and treat: headache and hyperprolactinemia. Curr Pain Headache Rep 16(4):365–370
Gudelsky GA, Nansel DD, Porter JC (1981) Role of estrogen in the dopaminergic control of prolactin secretion. Endocrinology 108(2):440–444
Villegas-Gabutti C, Pennacchio GE, Jahn GA, Soaje M (2016) Role of estradiol in the regulation of prolactin secretion during late pregnancy. Neurochem Res 41(12):3344–3355
Wang C, Chan V (1982) Divergent effects of prolactin on estrogen and progesterone production by granulosa cells of rat Graafian follicles. Endocrinology 110(4):1085–1093
Chang AS, Grant R, Tomita H, Kim H-S, Smithies O, Kakoki M (2016) Prolactin alters blood pressure by modulating the activity of endothelial nitric oxide synthase. Proc Natl Acad Sci U S A 113(44):12538–12543
Zhang L, Curhan GC, Forman J (2010) Plasma prolactin level and risk of incident hypertension in postmenopausal women. J Hypertens 28(7):1400–1405
Peterlin BL, Gupta S, Ward TN, Macgregor A (2011) Sex matters: evaluating sex and gender in migraine and headache research. Headache 51(6):839–842
Vega CB, Quigley L, Patel M, Price T, Arkopian A, Dussor G (2017) (137) Meningeal application of prolactin and CGRP produces female specific migraine-related behavior in rodents. J Pain 18(4):S11
Fedak KM, Bernal A, Capshaw ZA, Gross S (2015) Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology. Emerging themes in epidemiology 12:14
Rainero I, Valfre W, Savi L, Gentile S, Pinessi L, Gianotti L, Arvat E, Ghigo E, Del Rizzo P, Calvelli P, Limone P (2001) Neuroendocrine effects of subcutaneous sumatriptan in patients with migraine. Journal of endocrinological investigation 24(5):310–4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics
The present study was approved by the Ethics Committee of Ilam University of Medical Sciences.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Article highlights
• Association between blood prolactin and migraine pathogenesis was investigated using meta-analysis.
• The included studies (systematic review) were heterogeneous and random-effects model was applied.
• The pooled SMD for prolactin blood levels was 1.435 (95% confidence interval, 0.854 - 2.015). P value for the z-test was 0.000.
• Based on the findings, hyperprolactinemia is associated with migraine pathogenesis.
Rights and permissions
About this article
Cite this article
Noori-Zadeh, A., Karamkhani, M., Seidkhani-Nahal, A. et al. Evidence for hyperprolactinemia in migraineurs: a systematic review and meta-analysis. Neurol Sci 41, 91–99 (2020). https://doi.org/10.1007/s10072-019-04035-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-04035-7