Abstract
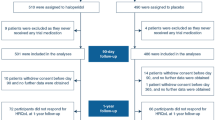
Quality of life (QOL) reflects the individual’s perception of the position within living contexts. This study was done to describe pre- and post-stroke QOLs of stroke survivors. A prospective longitudinal study was done among stroke survivors admitted to 13 hospitals in the western province of Sri Lanka. The calculated sample size was 260. The pre-stroke and post-discharge one-month QOL was gathered using short form-36 (SF-36) QOL tool. SF-36 includes questions on eight domains: general health, physical functioning, pain, role limitation due to physical problems, social functioning, vitality, role limitations due to emotional problems, and mental health. Univariate analysis was followed by determining the independent risk factors through multivariate analysis. The response rate was 81%. The disability was measured by the modified Rankin scale which ranges from 0 (no symptoms) to 6 (fatal outcome). The median (IQR) disability score was 4 (3 to 5). The post-discharge QOL scores were significantly lower than pre-stroke values (p < 0.05). With a higher pre-stroke QOL, younger age was significantly associated in six domains and higher income and better health infrastructure in two domains (p < 0.05). Six factors were determined to be independent risk factors for lower post-discharge QOL scores of SF-36: younger age (for general health and role limitation-physical domains), female gender (for physical functioning and pain domains), lower health infrastructure (for general health, vitality, and mental health domains), lower education (for pain domain), higher disability (for general health, physical functioning, vitality, social functioning, and mental health domains), and hypercholesterolemia (for role limitation-emotional domain). Stroke survivors have not regained their pre-stroke QOL at 1 month following the hospital discharge irrespective of income level and pre-stroke QOL. Higher pre- and post-stroke QOLs are associated with better statuses of social determinants of health.

Similar content being viewed by others
References
Hankey GJ (2013) The global and regional burden of stroke. Lancet Glob Health 1(5). https://doi.org/10.1016/S2214-109X(13)70095-0
Khoshnam SE, Winlow W, Farzaneh M, Farbood Y, Moghaddam HF (2017) Pathogenic mechanisms following ischemic stroke. Neurol Sci 38(7):1167–1186. https://doi.org/10.1007/s10072-017-2938-1
Colaianni V, Mazzei R, Cavallaro S (2016) Copy number variations and stroke. Neurol Sci 37(12):1895–1904. https://doi.org/10.1007/s10072-016-2658-y
Zhong W, Geng N, Wang P, Li Z, Cao L (2016) Prevalence, causes and risk factors of hospital readmissions after acute stroke and transient ischemic attack: a systematic review and meta-analysis. Neurol Sci 37(8):1195–1202. https://doi.org/10.1007/s10072-016-2570-5
WHO (2004). Global burden of stroke. atlas Hear Dis stroke. 15:50-51. doi:https://doi.org/10.1016/B978-1-4160-5478-8.10019-3.
Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World Neurosurg. 2011;76(6 SUPPL.). doi:https://doi.org/10.1016/j.wneu.2011.07.023.
Corbyn Z (2014) Stroke—statistics: a growing global burden. Nature 510(7506):S2–S3. https://doi.org/10.1038/510S2a
Fuentes B, Tejedor ED (2014) Stroke: the worldwide burden of stroke—a blurred photograph. Nat Rev Neurol 10(3):127–128. https://doi.org/10.1038/nrneurol.2014.17
WHO (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med 28(3):551–558 doi:10.5.12
Mahesh PKB, Gunathunga MW, Jayasinghe S, Arnold SM, Haniffa R, De Silva AP (2017) Pre-event quality of life and its influence on the post-event quality of life among patients with ST elevation and non-ST elevation myocardial infarctions of a premier province of Sri Lanka. Health Qual Life Outcomes 15(1):154. https://doi.org/10.1186/s12955-017-0730-9
Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. In: Cerebrovascular Diseases. Vol 27 ; 2009:204–214. doi:https://doi.org/10.1159/000200461
Opara JA, Jaracz K (2010) Quality of life of post-stroke patients and their caregivers. J Med Life 3(3):216–220 http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3018998&tool=pmcentrez&rendertype=abstract
Garratt A, Schmidt L, Mackintosh A, Fitzpatrick R (2002) Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ 324(7351):1417. https://doi.org/10.1136/bmj.324.7351.1417
Svetel MV, Jovic JS, Pekmezovic TD, Kostic VS (2015) Quality of life in patients with primary restless leg syndrome: community-based study. Neurol Sci 36(8):1345–1351. https://doi.org/10.1007/s10072-015-2103-7
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 health survey manual and interpretation guide. Bost New Engl Med Cent. 1993:1 v. (various pagings). http://books.google.com/books/about/SF_36_health_survey.html?id=WJsgAAAAMAAJ
Gunawardena NS, Seneviratne SRA, Atauda T (2003) An approach to validation of a multi-dimensional tool. J Coll Commun Phys Sri Lanka 8:18–26
Hofhuis JGM, Spronk PE, van Stel HF, Schrijvers AJP, Bakker J (2007) Quality of life before intensive care unit admission is a predictor of survival. Crit Care 11(4):R78. https://doi.org/10.1186/cc5970
Wehler M, Martus P, Geise A et al (2001) Changes in quality of life after medical intensive care. Intensive Care Med 27(1):154–159 http://www.ncbi.nlm.nih.gov/pubmed/11280627
Kranciukaite D, Rastenyte D (2006) Measurement of quality of life in stroke patients. Medicina (Kaunas) 42(9):709–716 http://www.ncbi.nlm.nih.gov/pubmed/21717044
Carod-Artal FJ (2012) Determining quality of life in stroke survivors. Expert Rev Pharmacoecon Outcomes Res 12(2):199–211. https://doi.org/10.1586/erp.11.104
Haley WE, Roth DL, Kissela B, Perkins M, Howard G (2011) Quality of life after stroke: a prospective longitudinal study. Qual Life Res 20(6):799–806. https://doi.org/10.1007/s11136-010-9810-6
Bugge C, Hagen S, Alexander H (2001) Measuring stroke patients’ health status in the early post-stroke phase using the SF36. Int J Nurs Stud 38(3):319–327. https://doi.org/10.1016/S0020-7489(00)00066-3
Jönsson A-C, Lindgren I, Hallström B, Norrving B, Lindgren A (2005) Determinants of quality of life in stroke survivors and their informal caregivers. Stroke 36(4):803–808. https://doi.org/10.1161/01.STR.0000160873.32791.20
Patel MD, McKevitt C, Lawrence E, Rudd AG, Wolfe CDA (2007) Clinical determinants of long-term quality of life after stroke. Age Ageing 36(3):316–322 7p. http://search.ebscohost.com/login.aspx?direct=true&db=cmedm&AN=17374601&site=ehost-live&scope=site%5Cnhttp://search.ebscohost.com/login.aspx?direct=true&db=c8h&AN=105997982&site=ehost-live&scope=site
Moon Y-S, Kim S-J, Kim H-C, Won M-H, Kim D-H (2004) Correlates of quality of life after stroke. J Neurol Sci 224(1–2):37–41. https://doi.org/10.1016/j.jns.2004.05.018
Vrdoljak D, Rumboldt M (2008) Quality of life after stroke in Croatian patients. Coll Antropol 32(2):355–359
Nichols-Larsen DS, Clark PC, Zeringue A, Greenspan A, Blanton S (2005) Factors influencing stroke survivors’ quality of life during subacute recovery. Stroke 36(7):1480–1484. https://doi.org/10.1161/01.STR.0000170706.13595.4f
Kwon S, Hartzema AG, Duncan PW, Lai SM (2004) Disability measures in stroke: relationship among the Barthel index, the functional independence measure, and the modified Rankin scale. Stroke 35(4):918–923. https://doi.org/10.1161/01.STR.0000119385.56094.32
Quinn TJ, Dawson J, Walters MR, Lees KR (2008) Variability in modified rankin scoring across a large cohort of international observers. Stroke 39(11):2975–2979. https://doi.org/10.1161/STROKEAHA.108.515262
Rocco A, Ringleb PA, Grittner U, Nolte CH, Schneider A, Nagel S (2015) Follow-up C-reactive protein level is more strongly associated with outcome in stroke patients than admission levels. Neurol Sci 36(12):2235–2241. https://doi.org/10.1007/s10072-015-2342-7
Banks JL, Marotta CA (2007) Outcomes validity and reliability of the modified rankin scale: implications for stroke clinical trials—a literature review and synthesis. Stroke 38(3):1091–1096. https://doi.org/10.1161/01.STR.0000258355.23810.c6
Kasner SE (2006) Clinical interpretation and use of stroke scales. Lancet Neurol 5(7):603–612. https://doi.org/10.1016/S1474-4422(06)70495-1
Kim JS, Choi-Kwon S, Kwon SU, Lee HJ, Park KA, Seo YS (2005) Factors affecting the quality of life after ischemic stroke: young versus old patients. J Clin Neurol 1:59–68. https://doi.org/10.3988/jcn.2005.1.1.59
Wijeratne T, Gunaratne P, Gamage R et al (2011) Stroke care development in Sri Lanka: the urgent need for neurorehabilitation services. Neurol Asia 16(2):149–151
Chang T, Gajasinghe S, Arambepola C (2011) Epidemiology of stroke in the district of Colombo, Sri Lanka: A community-based study Cerebrovasc Dis 32:6. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=70610079
Chang T, Gajasinghe S, Arambepola C (2015) Prevalence of stroke and its risk factors in urban Sri Lanka: population-based study. Stroke 46(10):2965–2968. https://doi.org/10.1161/STROKEAHA.115.010203
Ranawaka U, Alexander F, Nawaratne D, Liyanage H, Kulatunga A, Tissera N, et al. (2012) Factors affecting early outcome in Sri Lankan patients with stroke. Neurology. 78(1 Meeting Abstract):no pagination-no pagination. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed10&NEWS=N&AN=70727749
Wasay M, Khatri I, Kaul S (2014) Stroke in South Asian countries. Nat Rev Neurol 10(3):135–143. https://doi.org/10.1038/nrneurol.2014.13
Sprigg N, Gray LJ, Bath PMW et al (2012) Quality of life after ischemic stroke varies in western countries: data from the Tinzaparin in acute ischaemic stroke trial (TAIST). J Stroke Cerebrovasc Dis 21(7):587–593. https://doi.org/10.1016/j.jstrokecerebrovasdis.2011.01.007
Sacco RL, Kasner SE, Broderick JP et al (2013) An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American heart association/American stroke association. Stroke 44(7):2064–2089. https://doi.org/10.1161/STR.0b013e318296aeca
Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T (1980) Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 58(1):113–130 doi:D - NLM: PMC2395897 EDAT- 1980/01/01 MHDA- 1980/01/01 00:01 CRDT- 1980/01/01 00:00 PST - ppublish
Unalan D, Soyuer F, Ozturk A, Mistik S (2008) Comparison of SF-36 and WHOQOL-100 in patients with stroke. Neurol India 56(4):426–432. https://doi.org/10.4103/0028-3886.44573
Charan J, Biswas T (2013) How to calculate sample size for different study designs in medical research? Indian J Psychol Med 35(2):121–126. https://doi.org/10.4103/0253-7176.116232
Mahesh PKB, Gunathunga MW, Jayasinghe S et al (2017) Financial burden of survivors of medically-managed myocardial infarction and its association with selected social determinants and quality of life in a lower middle income country. BMC Cardiovasc Disord 17(1):251. https://doi.org/10.1186/s12872-017-0687-y
Mahesh P.K.B, Gunathunga M.W. JS. (2015) Influence of social determinants on the disease-outcome, financial burden and quality of life after a critical illness due to chronic non communicable diseases, among patients treated at government hospitals in the western province of Sri Lanka
Jayasekara RS, Schultz T (2007) Health status, trends, and issues in Sri Lanka. Nurs Health Sci 9(3):228–233. https://doi.org/10.1111/j.1442-2018.2007.00328.x
WHO. Closing the gap in a generation.health equity through action on the social determinants of health. 2008. doi:https://doi.org/10.1080/17441692.2010.514617
Author information
Authors and Affiliations
Contributions
All authors were involved in the planning of the research study. PKB was the principal investigator and was involved in getting ethics permissions, data collection, data analysis, and writing of the manuscript. MW, S, and SM were involved in data analysis, data interpretation, and writing of the manuscript. SN was involved in data collection, data entering, interpretation of data, and writing the manuscript. All authors went through the final manuscript.
Corresponding author
Ethics declarations
Ethics approval was obtained from the Ethics Review Committee of Sri Lanka Medical Association prior to the data collection (reference number ERC/119 approval was given on 27 August 2014). Informed written consent was obtained from the participants. Therefore, the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Specific national laws have been observed.
Conflict of interest
The authors declare that they no conflict of interest.
Consent for publication
The manuscript does not contain any personal details at the individual level.
Availability of data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. The dataset has been included as a supplementary file.
Electronic supplementary material
ESM 1
(SAV 245 kb)
Rights and permissions
About this article
Cite this article
Mahesh, P.K.B., Gunathunga, M.W., Jayasinghe, S. et al. Factors influencing pre-stroke and post-stroke quality of life among stroke survivors in a lower middle-income country. Neurol Sci 39, 287–295 (2018). https://doi.org/10.1007/s10072-017-3172-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-017-3172-6