Abstract
Objective
To determine the prevalence, clinical features, risk factors, and prognosis of interstitial lung disease (ILD) in patients with primary Sjogren's syndrome (pSS).
Methods
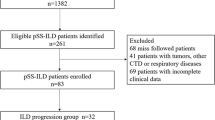
Data from 274 pSS patients from August 2013 to August 2022 were reviewed. The clinical features of pSS with ILD were revealed. Logistic regression was used to determine risk factors for ILD in pSS patients. Survival analysis and Cox regression were used to analyse the prognosis and prognostic factors of pSS patients.
Results
In pSS patients, the prevalence of ILD was 22.3% (61/274). The pSS patients with ILD were characterized by a late onset and long disease course, with a nonspecific interstitial pneumonia (NSIP) pattern as the predominant high-resolution computed tomography (HRCT) finding. Logistic regression results indicated that an age over 50 years old (OR 4.786, 95% CI 1.602–14.299; P = 0.005), purpuric rash (OR 4.695, 95% CI 1.537–14.339; P = 0.007), AMA-M2 antibody positivity (OR 2.582, 95% CI 1.166–5.722; P = 0.019), and diabetes (OR 2.514, 95% CI 1.025–6.167; P = 0.044) were risk factors for ILD in pSS patients. Cox regression results showed that advanced age (HR 1.240, 95% CI 1.088–1.413; P = 0.001) and cancer history (HR 8.411, 95% CI 1.771–39.934; P = 0.007) were risk factors for pSS patient survival.
Conclusion
This study showed that pSS patients with ILD tended to have a late onset and long course of pSS. An age over 50 years, purpuric rash, AMA-M2 antibody positivity, and diabetes were risk factors for ILD in pSS patients. Advanced age and cancer history were prognostic factors in pSS patients.
Key Points • This study showed that pSS patients with ILD tended to have a late-onset and lengthy course of pSS, with the NSIP pattern as the predominant lung image. • The risk factors for ILD in pSS patients determined in this study were an age over 50 years, purpuric rash, AMA-M2 antibody positivity, and diabetes. • The prognostic risk factors for pSS patients were advanced age and cancer history. |

Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- ILD:
-
Interstitial lung disease
- pSS:
-
Primary Sjogren's syndrome
- pSS-ILD:
-
Primary Sjögren’s syndrome-associated interstitial lung disease
- pSS-nonILD:
-
Primary Sjögren’s syndrome without interstitial lung disease
- CTD:
-
Connective tissue disease
- HRCT:
-
High-resolution computed tomography
- NSIP:
-
Nonspecific interstitial pneumonia
- UIP:
-
Usual interstitial pneumonia
- OP:
-
Organizing pneumonia
- LIP:
-
Lymphocytic interstitial
- ESR:
-
Erythrocyte sedimentation rate
- CRP:
-
C-reactive protein
- IgG:
-
Immunoglobulin G
- WBC:
-
White blood cell count
- PLT:
-
Platelet count
- ESSDAI:
-
EULAR primary Sjögren syndrome Disease Activity Index
- PFT:
-
Pulmonary function test
- FVC%:
-
Forced vital capacity percent predicted
- Dlco%:
-
Diffusion capacity CO percent predicted
- ANA:
-
Anti-nuclear antibody
- Anti-SSA :
-
Anti-Sjogren's syndrome A
- Anti-SSB:
-
Anti-Sjogren's syndrome B
- AMA-M2:
-
Anti-mitochondrial M2
- Anti-RNP:
-
Anti-ribonucleoprotein
- GERD:
-
Gastroesophageal reflux disease
- COPD:
-
Chronic obstructive pulmonary disease
- AIH:
-
Autoimmune hepatitis
- PBC:
-
Primary biliary cirrhosis
References
Ramos-Casals M, Brito-Zeron P, Siso-Almirall A et al (2012) Primary Sjogren syndrome. BMJ 344:e3821. https://doi.org/10.1136/bmj.e3821
Flament T, Bigot A, Chaigne B et al (2016) Pulmonary manifestations of Sjogren’s syndrome. Eur Respir Rev 25:110–123. https://doi.org/10.1183/16000617.0011-2016
Kuwana M, Gil-Vila A, Selva-O’Callaghan A (2021) Role of autoantibodies in the diagnosis and prognosis of interstitial lung disease in autoimmune rheumatic disorders. Ther Adv Musculoskelet Dis 13:1759720X211032457 https://doi.org/10.1177/1759720X211032457
Sambataro G, Ferro F, Orlandi M et al (2020) Clinical, morphological features and prognostic factors associated with interstitial lung disease in primary Sjgren’s syndrome: A systematic review from the Italian Society of Rheumatology. Autoimmun Rev 19:102447. https://doi.org/10.1016/j.autrev.2019.102447
Travis WD, Costabel U, Hansell DM et al (2013) An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 188:733–748. https://doi.org/10.1164/rccm.201308-1483ST
Vacchi C, Sebastiani M, Cassone G et al. (2020) Therapeutic Options for the Treatment of Interstitial Lung Disease Related to Connective Tissue Diseases. A Narrative Review. J Clin Med 9 https://doi.org/10.3390/jcm9020407
Jeganathan N, Sathananthan M (2020) Connective Tissue Disease-Related Interstitial Lung Disease: Prevalence, Patterns, Predictors, Prognosis, and Treatment. Lung 198:735–759. https://doi.org/10.1007/s00408-020-00383-w
Lee KA, Choi W, Kim J et al (2021) Elderly-onset primary Sjogren’s syndrome focused on clinical and salivary gland ultrasonographic features. Joint Bone Spine 88:105132. https://doi.org/10.1016/j.jbspin.2021.105132
Gao H, Sun Y, Zhang XY et al (2021) Characteristics and mortality in primary Sjogren syndrome-related interstitial lung disease. Medicine (Baltimore) 100:e26777. https://doi.org/10.1097/MD.0000000000026777
Kim YJ, Choe J, Kim HJ et al (2021) Long-term clinical course and outcome in patients with primary Sjogren syndrome-associated interstitial lung disease. Sci Rep 11(12827):20210618. https://doi.org/10.1038/s41598-021-92024-2
Ramos-Casals M, Anaya JM, Garcia-Carrasco M et al (2004) Cutaneous vasculitis in primary Sjogren syndrome: classification and clinical significance of 52 patients. Medicine (Baltimore) 83:96–106. https://doi.org/10.1097/01.md.0000119465.24818.98
Xuan L, Zhang YD, Li L et al (2017) Clinical Profile and Significance of Mucocutaneous Lesions of Primary Sjogren’s Syndrome: A Large Cross-sectional Study with 874 Patients. Chin Med J (Engl) 130:2423–2428. https://doi.org/10.4103/0366-6999.216403
Lin W, Xin Z, Ning X et al (2021) Clinical features and risk factors of Raynaud’s phenomenon in primary Sjogren’s syndrome. Clin Rheumatol 40:4081–4087. https://doi.org/10.1007/s10067-021-05749-w
Luppi F, Sebastiani M, Silva M et al (2020) Interstitial lung disease in Sjogren’s syndrome: a clinical review. Clin Exp Rheumatol 38(Suppl 126):291–300
Buvry C, Cassagnes L, Tekath M et al (2020) Anti-Ro52 antibodies are a risk factor for interstitial lung disease in primary Sjogren syndrome. Respir Med 163:105895. https://doi.org/10.1016/j.rmed.2020.105895
Cotton T, Fritzler MJ, Choi MY et al. (2022) Serologic phenotypes distinguish systemic lupus erythematosus patients developing interstitial lung disease and/or myositis. Lupus 9612033221122158 https://doi.org/10.1177/09612033221122158
Zhu LL, Yang LH, Xie QB et al. (2018) [Clinicopathological Analysis of Autoimmune Hepatitis with Sjogren's Syndrome]. Sichuan Da Xue Xue Bao Yi Xue Ban 49:183–187
Kopf S, Groener JB, Kender Z et al (2018) Breathlessness and Restrictive Lung Disease: An Important Diabetes-Related Feature in Patients with Type 2 Diabetes. Respiration 96:29–40. https://doi.org/10.1159/000488909
Chiu YH, Spierings J, de Jong PA et al (2021) Predictors for progressive fibrosis in patients with connective tissue disease associated interstitial lung diseases. Respir Med 187:106579. https://doi.org/10.1016/j.rmed.2021.106579
Rajasurya V, Gunasekaran K, Surani S (2020) Interstitial lung disease and diabetes. World J Diabetes 11:351–357. https://doi.org/10.4239/wjd.v11.i8.351
Dong X, Zhou J, Guo X et al (2018) A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjogren’s syndrome-related interstitial lung disease in a Chinese population. Clin Rheumatol 37:2981–2988. https://doi.org/10.1007/s10067-018-4289-6
Raghu G, Remy-Jardin M, Richeldi L et al (2022) Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am J Respir Crit Care Med 205:e18–e47. https://doi.org/10.1164/rccm.202202-0399ST
Ramos-Casals M, Solans R, Rosas J et al (2008) Primary Sjogren syndrome in Spain: clinical and immunologic expression in 1010 patients. Medicine (Baltimore) 87:210–219. https://doi.org/10.1097/MD.0b013e318181e6af
Nasser M, Larrieu S, Si-Mohamed S et al. (2021) Progressive fibrosing interstitial lung disease: a clinical cohort (the PROGRESS study). Eur Respir J 57 https://doi.org/10.1183/13993003.02718-2020
Kamiya Y, Fujisawa T, Kono M et al (2019) Prognostic factors for primary Sjogren’s syndrome-associated interstitial lung diseases. Respir Med 159(105811):20191105. https://doi.org/10.1016/j.rmed.2019.105811
He SH, He YJ, Guo KJ et al (2022) Risk factors for progression of interstitial lung disease in Sjogren’s syndrome: a single-centered, retrospective study. Clin Rheumatol 41(1153–1161):20211110. https://doi.org/10.1007/s10067-021-05984-1
Kim HJ, Kim KH, Hann HJ et al (2017) Incidence, mortality, and causes of death in physician-diagnosed primary Sjogren’s syndrome in Korea: A nationwide, population-based study. Semin Arthritis Rheum 47:222–227. https://doi.org/10.1016/j.semarthrit.2017.03.004
Singh AG, Singh S, Matteson EL (2016) Rate, risk factors and causes of mortality in patients with Sjogren’s syndrome: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford) 55:450–460. https://doi.org/10.1093/rheumatology/kev354
Maciel G, Crowson CS, Matteson EL et al (2017) Incidence and Mortality of Physician-Diagnosed Primary Sjogren Syndrome: Time Trends Over a 40-Year Period in a Population-Based US Cohort. Mayo Clin Proc 92:734–743. https://doi.org/10.1016/j.mayocp.2017.01.020
Nannini C, Jebakumar AJ, Crowson CS et al (2013) Primary Sjogren’s syndrome 1976–2005 and associated interstitial lung disease: a population-based study of incidence and mortality. BMJ Open 3:e003569. https://doi.org/10.1136/bmjopen-2013-003569
Xu Y, Zhou J, Dong X et al (2020) Risk factors for progression and prognosis of primary Sjogren’s syndrome-associated interstitial lung disease in a Chinese population. Int J Rheum Dis 23:1734–1740. https://doi.org/10.1111/1756-185X.14023
Qian J, He C, Li Y et al. (2021) Ten-year survival analysis of patients with primary Sjogren's syndrome in China: a national prospective cohort study. Ther Adv Musculoskelet Dis 13:1759720X211020179 https://doi.org/10.1177/1759720X211020179
Funding
This research was supported by the Natural Science Foundation of Zhejiang Province, China (Y21H270014), the TCM Science and Technology Program of Zhejiang Province, China (2020ZZ006), and the Scientific Research Project of Zhejiang Provincial Education Department, China (Y202146162).
Author information
Authors and Affiliations
Contributions
Y.H, Y.Q., and Z.X. designed this study. M.G. was involved in the case collection, data analysis, and patient follow-up. Y.H. and Y.Q. finished the article writing. F.Z., Y.Z., and Z.X. revised the manuscript. W.C., X.W., and J.S. supervised this study and reviewed the article, contributing equally to this work as co-correspondence authors. All authors approved the submission of the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
None declared.
Data sharing statement
No additional data were available.
Patient and public involvement
Patients and the public were involved in the design and conception of the study, and there are plans to disseminate the results to patients.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, Y., Qiu, Y., Xie, Z. et al. Risk factors and prognosis of interstitial lung disease for primary Sjögren syndrome patients: A retrospective case‒control study. Clin Rheumatol 42, 3033–3041 (2023). https://doi.org/10.1007/s10067-023-06596-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06596-7