Abstract
Background
The aim of this study was to analyze the relationship of the estimated glomerular filtration rate (eGFR) to hydroxychloroquine (HCQ) blood concentrations in systemic lupus erythematosus (SLE) patients.
Method
Patients with SLE who had been taking HCQ for more than 12 months were recruited. All subjects gave written informed consent. Various clinical characteristics and laboratory values were examined. The blood concentration of HCQ was measured by high-performance liquid chromatography, and the relationship of eGFR to HCQ blood concentration was mainly investigated.
Result
In total, 115 patients with SLE receiving long-term HCQ therapy were included in the study. The median concentration of HCQ was 1096 ng/ml (range 116–8240 ng/ml). The eGFR was strongly associated with blood concentration of HCQ (P = 0.011, P < 0.05), when adjusted for age, sex, body mass index (BMI), weight-adjusted dose, prednisone use and immunosuppressive drug use. No statistically significant association were found between age, duration, BMI, weight-adjusted HCQ dose, corticosteroid use, immunosuppressant use and blood concentrations of HCQ.
Conclusion
We provided novel evidence that impaired renal function influenced the blood concentration of HCQ. Patients with low eGFR need to adjust the HCQ dosage according to the monitoring results of HCQ blood concentrations.
Key points • A higher HCQ blood concentration was associated with low eGFR. • This finding reinforces the importance of routine HCQ measurement to maintain normal blood concentrations. • HCQ blood monitoring will be useful for dose modification in patients with renal dysfunction. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydroxychloroquine (HCQ) is a traditional antimalarial drug that is effective in the treatment of systemic lupus erythematosus (SLE). In addition to immune regulation through the inhibition of immune activation and the reduction of cytokine production, it is associated with a wide range of benefits, such as its anti-infection, anti-thrombotic, lipid-lowering, photoprotection, hypoglycemic, anti-osteoporosis, and anti-inflammation qualities, and improvement of dry eye [1, 2].
Previous studies [3,4,5,6,7] have identified that a very low blood concentration of HCQ is a simple marker and predictor of systemic lupus erythematosus exacerbation and treatment failure. A recent study showed that higher HCQ blood concentrations predicted retinopathy of HCQ [8]. Thus, interest in the measurement of HCQ blood concentrations has increased.
Due to its unique pharmacokinetic and pharmacogenomic characteristics, there is significant interindividual variability in HCQ blood concentrations, even if individuals take the same dose [9,10,11]. Several studies have analyzed the factors that influence the changes in the blood concentration of HCQ [12,13,14,15]. However, these studies have revealed contradictory findings, particularly on renal function. Most of the studies found a significant association of impaired renal function with high blood HCQ concentration [12, 14]. Another study did not find a relationship between renal function and HCQ concentration. However it should be noted that due to the small sample size of the study, only 3.7% of patients had renal dysfunction classified as CKD stage 3 or greater [13]. Another study including patients with renal dysfunction showed a trend toward lower blood HCQ concentrations [15]. However it should be noted that the patients took lower than usual doses (200 mg/day). Although the correlation between renal function and blood HCQ concentration remains controversial, we believe the negative findings could be attributed to the low power or low doses. Does the dosage of HCQ need to be adjusted in patients with renal dysfunction? How can the concentration of HCQ in the blood be modified in the presence of renal dysfunction with a decrease in eGFR? Therefore, the purpose of the study was to identify the relationship of eGFR to HCQ blood concentrations in SLE patients.
Method
Study design
This was a cross-sectional study aimed at exploring various factors associated with the blood concentration of HCQ, especially focusing on the effect of eGFR. The human ethics committees at the Peking University People’s Hospital approved the study (2020PHB209-01). All research adhered to the tenets of the Declaration of Helsinki. All subjects gave written informed consent.
Population
Patients who received HCQ (400 mg/day) for at least 12 months were included in this study. Whole blood was collected, and laboratory values were collected from the electronic medical record system (HIS platform). We also analyzed blood concentrations of HCQ in patients with chronic renal insufficiency. We used the chronic kidney disease-epidemiology collaboration (CKD-EPI) equation to estimate the eGFR [16]. Renal function was classified on the basis of the stage of chronic kidney disease (CKD), with eGFR ≧90, 60–89, 30–59, 15–29, and < 15 ml/minute/1.73 m.2 corresponding to stage 1, 2, 3, 4, and 5 disease, respectively [17].
Sample processing
Whole-blood HCQ can be quantified by high-performance liquid chromatography (HPLC). 300 μl of blood sample and 10 μl of 25 μl•mL−1 metronidazole solution which was used as the internal standard were extracted with 900 μl of ethyl acetate, redissolved with 200 μl of mobile phase after drying with nitrogen, and 20 μl of supernatant was taken for determination. Chromatographic separation was performed on a Symmetry® C18 column (4.6 mm x 250 mm, 5 μm) at 35℃ using a mobile phase of 20 mmol•L−1 KH2PO4-acetonitrile (85:15, ν/ν, pH adjusted to 3 by H3PO4) at a flow rate of 0.8 mL•min-1 and the detection wavelength was 254 nm. A calibration curve (100–5,000 ng/ml) was generated to validate the method. The relative standard deviations of intraday and interday precisions for HCQ were within 4%. The selectivity, sensitivity, precision, and accuracy of the method were established by an internal standard prior to measurement. The method was simple, sensitive, and accurate, and could be used for the measurement of HCQ blood concentrations in human blood.
Statistical analysis
We used descriptive statistics and plots to test the data. Because the HCQ blood concentration was not normally distributed, it was natural log–transformed. Categorical variables are presented as frequencies and percentages, and continuous variables are presented as the means and standard deviations. Normally distributed values are expressed as the mean ± SD. Nonnormally distributed values were categorized into quartiles. The clinical characteristics of patients in the low and high concentration group were compared with the chi-square test for categorical variables and the Mann–Whitney test for continuous variables. The association of eGFR and HCQ blood concentration was assessed with the use of multivariable logistic regression models. According to possible confounders, we adjusted multivariable logistic regression models for age, sex, body mass index (BMI), weight-adjusted dose, and use of prednisone and immunosuppressive drugs. In another separate analysis, for multiple group comparisons distributed by CKD, one-way analysis of variance (ANOVA) or a nonparametric Mann–Whitney test was performed. The effect of eGFR on HCQ concentration was analyzed by a simple linear regression model. Statistical analyses were performed using SPSS Statistics 24.0 software (SPSS Inc., Armonk, NY, USA) and presented using GraphPad Prism 8.0 software (GraphPad Software Inc., San Diego, CA, USA). The adopted significance levels in all analyses were set at 5%.
Result
Clinical characteristics of patients with SLE
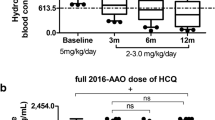
The study included 111 patients who were receiving the same daily dose of HCQ (400 mg/day every day). The median concentration of HCQ was 1096 ng/ml (range 116–8240 ng/ml). The analysis was conducted after dividing patients into two groups according to the blood concentration of HCQ. The patients with an HCQ blood concentration equal to or lower than the median (1096 ng/ml) were classified as the low concentration group (n = 55), and the patients with an HCQ blood concentration higher than the median (1096 ng/ml) were classified as the high concentration group (n = 56). The characteristics of both groups are shown in Table 1. The weight (p = 0.008), body mass index (p = 0.036), and weight-adjusted HCQ dose (p < 0.001) were significantly different between the two groups. The age, sex ratio, medication duration time, cumulative dose and combination therapy (prednisone and immunosuppressive drugs) were similar for the low and high blood concentration groups. We also examined the association between laboratory values and HCQ blood concentrations, and a less significant relationship was observed (Table 2). The patients with low concentrations of HCQ had a higher estimated glomerular filtration rate (eGFR) than those with high HCQ concentrations [: mean-standard deviation: (106.21 ± 14.95) vs. (99.22 ± 25.65), p = 0.011] (Fig. 1). By drawing the scatter plot, it is intuitively judged that there is a linear relationship between HCQ concentrations and the eGFR (F = 4.099, P < 0.045) (Fig. 2).
The relationship of renal function to blood concentrations of HCQ
Through multivariate analysis, we identified independent factors related to high blood concentrations of HCQ. The eGFR was independently associated with a high blood concentration of HCQ. There was a significant relationship between the eGFR and blood HCQ concentration in unadjusted models (p = 0.006) and in Model 1, which was adjusted for age, sex, BMI, weight-adjusted dose, use of prednisone and immunosuppressive drugs (p = 0.005) (Table 3).
When patients were categorized according to CKD stage, only 6 patients had chronic renal insufficiency (eGFR < 60 ml/min); among them, five people had CKD stage 3, and one person had CKD stage 4. These patients also took the same daily dose of HCQ (400 mg/day every day), and it was not adjusted to take CKD into account. The median blood concentration of HCQ was 2404.04 ng/ml (950.80–8240.20 ng/ml) and was significantly higher than the median blood concentration of HCQ in the 105 patients of the study who also received 400 mg/day (1046 ng/ml [range 116–7374.89 ng/ml]; P = 0.049). There was no significant difference in HCQ blood concentration according to the five different CKD stages, but there was a trend towards a difference but, perhaps due to the small sample size, the difference was not significant. When one patient had CKD stage 4, the HCQ blood concentration was especially high (n = 1, 8240.0 ng/mL) (Table 4).
Discussion
In this study, we identified factors that might explain interindividual variations in blood concentrations of HCQ in patients with SLE. Interestingly, we identified a clear correlation between eGFR and blood concentration of HCQ. Although several previous studies [12,13,14,15] examined the relationship between HCQ blood concentrations and variables such as age, BMI, smoking, drug-drug interactions, dosage, laboratory examination (white blood cell, blood platelet, hemoglobin, neutrophil, etc.), few have studied renal function. We found a significant association of low eGFR with high blood concentrations of HCQ.
Similarly, Ji Yeon Lee et al. conducted a cross-sectional study to explore the relationship between renal function and blood concentration of HCQ. They found high blood HCQ concentrations in 4 patients with abnormal eGFR compared with 23 SLE patients with normal eGFR [13]. Another study performed by M. Jallouli et al. also found an inverse correlation between the estimated glomerular filtration rate and HCQ blood concentration, and in their study, they also studied three patients receiving long-term dialysis and confirmed that HCQ was not dialyzable [12].
However, a study including 15 patients with renal dysfunction (creatinine: 1.4–4.9 mg/ml) and 6 patients with more severe renal dysfunction (creatinine > 5.0 mg/ml) showed a trend toward lower HCQ concentrations with renal failure, suggesting that renal failure dosing led to suboptimum HCQ concentrations [15]. Although our study had an opposite conclusion to the above two studies, we thought the reason for the inconsistency was the lower than usual doses, in which the patients only received HCQ doses of 200 mg/d. On the other hand, it suggested that blindly reducing the dose was not the best way to quantitate renal disease with respect to HCQ dosing. Moreover, another study also found no statistically significant association between renal function and [HCQ] or [DHCQ]. However, the author recognized that the study population was not ideal for studying the relationship due to low power [14]. Although it is still controversial to conclude that HCQ blood concentrations are associated with renal function, our positive finding could be attributed to high power. As previously described, retinal toxicity [18, 19], neuromyotoxicity [20] and cardiotoxicity [21] of HCQ may be enhanced by renal dysfunction. HCQ can lead to retinal toxicity, and an increasing number of patients with advanced HCQ retinopathy have been had identified in recent publications, thus suggesting a need for guidelines that focus on recommending appropriate dosing and toxicity monitoring [22, 23]. The most important risk factor is greatly dependent on daily dose, which is calculated using body weight. Guidelines aimed at preventing retinal toxicity recommend using less than 5 mg/kg/day of actual body weight per day instead of 6.5 mg/kg/day of ideal body weight. To date, there are few guidelines for dose adjustment in patients with renal dysfunction. The Joint European League Against Rheumatism and European Renal Association–European Dialysis and Transplant Association (EULAR/ERA–EDTA) guidelines [22] state that HCQ is recommended for all patients without contraindications, with a maximum dose of 5 mg/kg/day. When GFR < 30 ml/min, the dose can be reduced by 50%. Kidney Disease: Improving Global Outcomes (KDIGO) guidelines [23] also state that HCQ is appropriate for all patients without contraindications, but the recommended dosage varies. Guidelines recommend an initial dose of 6.5 mg/kg/day of ideal body weight or 400 mg/ day, and 4–5 mg/kg/day during maintenance treatment. A dose reduction of at least 25% is recommended when eGFR is less than 30 ml/min/1.73m2. We think that HCQ blood monitoring will be useful. Therefore, further studies are needed in patients with renal dysfunction to confirm our findings and to examine the association among renal function, HCQ blood concentration and toxicity.
Conclusion
In conclusion, we provide novel evidence that a higher HCQ blood concentrations are associated with low eGFR. This finding reinforces the importance of routine HCQ measurement to maintain normal blood concentrations. HCQ blood monitoring will be useful for dose modification in patients with renal dysfunction. With the popularization of blood drug concentration determination, such data might be useful for clinicians.
Data Availability
The original contributions presented in the study are included in the article, and further inquiries can be directed to the corresponding author.
References
Ruiz-Irastorza G, Martín-Iglesias D, Soto-Peleteiro A (2020) Update on antimalarials and systemic lupus erythematosus. Curr Opin Rheumatol 32:572–582. https://doi.org/10.1097/BOR.0000000000000743
Chi CM, Hamijoyo L, Kasitanon N, Chen DY, Tanaka Y (2021) The asia-pacific league of associations for rheumatology consensus statements on the management of systemic lupus erythematosus. The Lancet Rheumatol 3:e517–e531. https://doi.org/10.1016/S2665-9913(21)00009-6
Costedoat-Chalumeau N, Galicier L, Aumaître O, Francès C, Le Guern V, Lioté F, Smail A, Limal N, Perard L, Desmurs-Clavel H, du Boutin LT, Asli B, Kahn JE, Pourrat J, Sailler L, Ackermann F, Papo T, Sacré K, Fain O, Stirnemann J, Cacoub P, Jallouli M, Leroux G, Cohen-Bittan J, Tanguy ML, Hulot JS, Lechat P, Musset L, Amoura Z, Piette JC, Group PLUS (2013) Hydroxychloroquine in systemic lupus erythematosus: results of a French multicentre controlled trial (PLUS Study). Ann Rheum Dis 72:1786–1792. https://doi.org/10.1136/annrheumdis-2012-202322
Costedoat-Chalumeau N, Amoura Z, Hulot JS, Aymard G, Leroux G, Marra D, Lechat P, Piette JC (2007) Very low blood hydroxychloroquine concentration as an objective marker of poor adherence to treatment of systemic lupus erythematosus. Ann Rheum Dis 66:821–824. https://doi.org/10.1136/ard.2006.067835
Costedoat-Chalumeau N, Le Guern V, Piette JC (2014) Determining adherence to therapeutic regimens in patients with chronic illness: comment on the article by Waimann et AI. Arthritis Rheumatol 66:770. https://doi.org/10.1002/art.38243
Costedoat-Chalumeau N, Pouchot J, Guettrot-Imbert G, Le Guern V, Leroux G, Marra D, Morel N, Piette JC (2013) Adherence to treatment in systemic lupus erythematosus patients. Best Pract Res Clin Rheumatol 27:329–340. https://doi.org/10.1016/j.berh.2013.07.001
Ting TV, Kudalkar D, Nelson S, Cortina S, Pendl J, Budhani S, Neville J, Taylor J, Huggins J, Drotar D, Brunner HI (2012) Usefulness of cellular text messaging for improving adherence among adolescents and young adults with systemic lupus erythematosus. J Rheumatol 39:174–179. https://doi.org/10.3899/jrheum.110771
Petri M, Elkhalifa M, Li J, Magder LS, Goldman DW (2020) Hydroxychloroquine Blood Levels Predict Hydroxychloroquine Retinopathy. Arthritis Rheumatol 72:448–453. https://doi.org/10.1002/art.41121
Carmichael SJ, Day RO, Tett SE (2013) A cross-sectional study of hydroxychloroquine concentrations and effects in people with systemic lupus erythematosus. Intern Med J 43:547–553. https://doi.org/10.1111/imj.12100
Costedoat-Chalumeau N, Amoura Z, Hulot JS, Hammoud HA, Aymard G, Cacoub P, Francès C, Wechsler B, du Huong LT, Ghillani P, Musset L, Lechat P, Piette JC (2006) Low blood concentration of hydroxychloroquine is a marker for and predictor of disease exacerbations in patients with systemic lupus erythematosus. Arthritis Rheum 54:3284–3290. https://doi.org/10.1002/art.22156
Tett S, Day R, Cutler D (1996) Hydroxychloroquine relative bioavailability: within subject reproducibility. Br J Clin Pharmacol 41:244–246. https://doi.org/10.1111/j.1365-2125.1996.tb00190.x
Jallouli M, Galicier L, Zahr N, Aumaître O, Francès C, Le Guern V, Lioté F, Smail A, Limal N, Perard L, Desmurs-Clavel H, Le Thi Huong D, Asli B, Kahn JE, Pourrat J, Sailler L, Ackermann F, Papo T, Sacré K, Fain O, Stirnemann J, Cacoub P, Leroux G, Cohen-Bittan J, Sellam J, Mariette X, Blanchet B, Hulot JS, Amoura Z, Piette JC, Costedoat-Chalumeau N, Plaquenil Lupus Systemic Study Group (2015) Determinants of hydroxychloroquine blood concentration variations in systemic lupus erythematosus. Arthritis Rheumatol 67:2176–84. https://doi.org/10.1002/art.39194
Yeon Lee J, Lee J, Ki Kwok S, Hyeon JuJ, Su Park K, Park SH (2017) Factors Related to Blood Hydroxychloroquine Concentration in Patients With Systemic Lupus Erythematosus. Arthritis Care Res (Hoboken) 69:536–542. https://doi.org/10.1002/acr.22962
Lee JY, Luc S, Greenblatt DJ, Kalish R, McAlindon TE (2013) Factors associated with blood hydroxychloroquine level in lupus patients: renal function could be important. Lupus 22(5):541–542. https://doi.org/10.1177/0961203313476361
Durcan L, Clarke WA, Magder LS, Petri M (2015) Hydroxychloroquine Blood Levels in Systemic Lupus Erythematosus: Clarifying Dosing Controversies and Improving Adherence. J Rheumatol 42:2092–2097. https://doi.org/10.3899/jrheum.150379
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1-266
Melles RB, Marmor MF (2014) The risk of toxic retinopathy in patients on long-term hydroxychloroquine therapy. JAMA Ophthalmol 132:1453–1460. https://doi.org/10.1001/jamaophthalmol.2014.3459
Marmor MF, Kellner U, Lai TY, Melles RB, Mieler WF, American Academy of Ophthalmology (2016) Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision). Ophthalmology 123:1386–1394. https://doi.org/10.1016/j.ophtha.2016.01.058
Stein M, Bell MJ, Ang LC (2001) Hydroxychloroquine neuromyotoxicity. J Rheumatol 27:927–2931
Costedoat-Chalumeau N, Hulot JS, Amoura Z, Leroux G, Lechat P, Funck-Brentano C, Piette JC (2007) Heart conduction disorders related to antimalarials toxicity: an analysis of electrocardiograms in 85 patients treated with hydroxychloroquine for connective tissue diseases. Rheumatology (Oxford) 46:808–810. https://doi.org/10.1093/rheumatology/kel402
Fanouriakis A, Kostopoulou M, Cheema K, Anders HJ, Aringer M, Bajema I, Boletis J, Frangou E, Houssiau FA, Hollis J, Karras A, Marchiori F, Marks SD, Moroni G, Mosca M, Parodis I, Praga M, Schneider M, Smolen JS, Tesar V, Trachana M, van Vollenhoven RF, Voskuyl AE, Teng YKO, van Leew B, Bertsias G, Jayne D, Boumpas DT (2020) 2019 Update of the Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis. Ann Rheum Dis 79:713–723. https://doi.org/10.1136/annrheumdis-2020-216924
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int 100:S1–S276. https://doi.org/10.1016/j.kint.2021.05.021
Acknowledgements
We gratefully thank Dr. Zhan-guo Li of the department of rheumatology & immunology and Dr. Lin Huang of the department of pharmacy of the Peking University People's Hospital in China for their contribution to platform support.
Funding
The research was supported by the Beijing Natural Science Foundation (grant number 7184254).
Author information
Authors and Affiliations
Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Jing He had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Xue Zhong; Analysis and interpretation: Xue Zhong, Jing He; Data collection: Xue Zhong, Yue-bo Jin and Qin Zhang; Sample processing: Si-Lu Liu; Writing: Xue Zhong; Editing: Jing He.
Corresponding author
Ethics declarations
Ethics approval
The human ethics committees at the Peking University People’s Hospital approved the study (2020PHB209-01). All research adhered to the tenets of the Declaration of Helsinki. All subjects gave written informed consent.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Research funding played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, X., Jin, Yb., Zhang, Q. et al. Low estimated glomerular filtration rate is an independent risk factor for higher hydroxychloroquine concentration. Clin Rheumatol 42, 1943–1950 (2023). https://doi.org/10.1007/s10067-023-06576-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06576-x