Abstract
Objectives
The use of long-term corticosteroids during pregnancy has been growing over the past decades. Corticosteroids can be given when an auto-inflammatory disease like rheumatoid arthritis (RA) is too active. Several studies have shown that long-term corticosteroids use in pregnancy is associated with maternal and fetal adverse outcomes, like preeclampsia, shorter gestational age, lower birth weight, and rapid catch-up growth. These last two outcomes could influence the insulin resistance later in life. Our objective was to investigate whether prednisone use in pregnant women with RA induces insulin resistance in offspring.
Methods
One hundred three children were included after their mother had participated in a prospective cohort study on RA and pregnancy. Forty-two children were in utero exposed to prednisone and 61 were non-exposed. To assess insulin resistance, we measured homeostasis model of assessment insulin resistance (HOMA-IR) and serum adiponectin and lipid levels, corrected for body fat distribution.
Results
An average of 6 mg prednisone on a daily use gave no difference in mean HOMA-IR (SD) between the children who were prednisone-exposed in utero (1.10 (0.84)) and those non-exposed (1.09 (0.49)). No difference was found in mean adiponectin level, body fat distribution, or lipid levels such as total cholesterol, fasting triglyceride, or high-density lipoprotein.
Conclusion
Children who are prednisone-exposed in utero (low dose) have no increased risk for insulin resistance at the age of approximately 7 years. These findings are reassuring because the prednisone use during pregnancy is increasing worldwide. Further research has to be performed to evaluate if the insulin resistance remains absent in the future.
Key Points • What is already known on this topic—long-term corticosteroids use in pregnancy is associated with fetal adverse outcomes, like lower birth weight and rapid catch-up growth which can influence the insulin resistance later in life. • What this study adds—long-term corticosteroids use in pregnant women with rheumatoid arthritis has no increased risk for insulin resistance in the offspring. • How this study might affect research, practice, or policy—findings are reassuring because prednisone use during pregnancy is increasing worldwide. Further research should evaluate if the insulin resistance remains absent in the future. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of long-term corticosteroids during pregnancy has been growing over the past decades. Recent study showed a steady increase from 2 to 81 per 100,000 pregnancies over more than a decade [1]. Emphasizing the magnitude of this trend in a variety of immunological and inflammatory diseases, various studies show that long-term corticosteroids use in pregnancy is associated with adverse maternal and fetal adverse outcomes, like preeclampsia, lower gestational age, lower birth weight, and rapid cath-up growth [1,2,3]. These last two outcomes are associated with insulin resistance later in life [4].
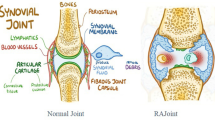
Rheumatoid arthritis (RA) is one of those inflammatory, autoimmune diseases that is contributing to this steady increase of long-term corticosteroid use during pregnancy. It is a systemic disease which often affects women of childbearing age. RA disease activity declines in only half of the pregnancies [5]. Therefore, medication like prednisone can be critical. It is not clear to which extent prednisone can pass the placenta [6]. At least in early gestation, when the placenta has not yet fully developed, prednisone may influence the fetal programming in humans [6,7,8]. Fetal programming is a theory that suggests that certain actions during certain points of pregnancy may cause permanent effects on the fetus and also later in life. In fetal development, the maternal glucocorticoids are critical in normal development of the fetus, as they are involved in the growth and maturation of many organ systems [9].
Experimental studies suggested that in utero exposure to prednisone can lead to fetal programming with persistently increased glucocorticoid effects throughout childhood, creating insulin resistance later in life [7].
In healthy, young children, the Homeostasis Model of Assessment Insulin Resistance (HOMA-IR) is an appropriate ethically accepted method to measure insulin resistance [10, 11]. Serum adiponectin levels will also indicate whether children have signs of insulin resistance. Adiponectin is a hormone mainly produced by white adipose tissue and levels are significantly lower in obese people [12]. High levels of adiponectin are associated with a lower risk of myocardial infarction and development of atherosclerosis. Adiponectin plays an important role in the pathogenesis of metabolic disease, like obesity and type 2 diabetes [13,14,15].
The aim of our study was to explore an association between maternal prednisone use during pregnancy and the risk on insulin resistance in the offspring. We hypothesized that exposure to synthetic glucocorticoids in utero increases insulin resistance in the children. We therefore determined the insulin resistance in children who had been exposed to synthetic glucocorticoids in utero. If prednisone-exposure in utero would affect the manifestation of insulin resistance in the prepubertal offspring, it would increase the risk for a less favourable health profile later in life.
Methods
The study cohort consisted of 103 healthy children born from mothers participating in the PARA-study (pregnancy-induced amelioration of rheumatoid arthritis). In this prospective, nationwide cohort study, pregnant women with RA (n = 255) were visited several times at their home address were a physical examination was performed and information on disease activity including medication use was collected [5]. To calculate the RA disease activity score (DAS28), we examined 28 joints and used 3 variables to make the calculation: number of swollen joints, number of tender joints, and serum C-reactive protein (CRP) level [16, 17]. Information on medical history regarding gestational age, birth weight, and postnatal complications were conducted. Birth weight was expressed as birth weight standard deviation scores (birth weight SDS), corrected for gestational age and gender [18].
After participating in the PARA-study, all mothers were contacted by mail and phone to participate in the follow-up study. Children aged 5 years or older were invited to visit the Sophia Children’s Hospital in Rotterdam. During this visit, fasting blood samples were taken, anthropometric measurements were performed, and a DXA-scan (dual-energy X-ray absorptiometry) to evaluate fat distribution was executed. This study has approved by the Medical Ethics Committee at the Erasmus Medical Centre (Rotterdam, The Netherlands). All parents gave their written informed consent.
HOMA-IR
Fasting blood samples were collected between 0800 and 1000 h to determine glucose and insulin level. One child was excluded from analyses concerning insulin sensitivity due to a non-fasting blood sample. Plasma glucose was measured on a Roche modular P analyser (Roche Diagnostics, Almere, The Netherlands). Plasma insulin concentrations were measured using an Immulite 2000 (Siemens healthcare Diagnostics B.V. Den Haag, The Netherlands). For glucose, the intra- and inter-assay coefficient of variation was 0.7% and 1.2% and for insulin 5.5% and 7.3%, respectively.
Insulin resistance was calculated using the Homeostasis Model of Assessment Insulin Resistance (HOMA-IR: [insulin (μIU/mL) x glucose (mmol/L)] / 22.5) [13, 14]. Healthy children have a HOMA-IR score of 1, and insulin resistance is present when the HOMA-IR ≥ 2.5 [11, 19, 20]. Due to the skewed distribution of the HOMA-IR, analyses were performed after log-transformation.
Adiponectin
Fasting levels of adiponectin were measured on a Roche modular P analyser (Roche Diagnostics, Almere, The Netherlands). The intra- and inter-assay coefficient of variation for samples was less than 3.82% and 5.15%.
Fat distribution
Other factors that can contribute to the presence and development of insulin resistance are weight, more specifically body fat mass, and the distribution of the body fat. Abdominal distribution of body fat has significant impact on the development of insulin resistance and creates an increased risk for metabolic disease independent of total body fat, while fat in the lower body is protective [21,22,23,24]. We therefore measured height and weight of the child. Body mass index (BMI) was calculated by dividing weight (kilograms) by the square of height (meters).
Visceral fat distribution has significant impact on decrease in adiponectin levels, but this decrease in adiponectin levels was not seen in case of subcutaneous fat [25, 26]. Visceral fat, also known as organ fat or intra-abdominal fat, is located between internal organs and subcutaneous fat is found underneath the skin. Therefore, circumferences of the arm, waist, and hip, but also skinfolds of triceps, biceps, subscapular, and suprailiac were performed. Visceral fat distribution was assessed by the ratio waist to hip circumference and by the ratio skinfolds trunk (subscapular + suprailiac) to peripheral (triceps + biceps). All measurements were executed by the same doctor and with the same scale. Measurements were performed 3 times and the mean value was used for analysis. All values were transformed to standard deviation scores (SDS) for age and gender according to Dutch reference values [27, 28], using the Growth Analyser (version 4.0; Growth analyser BV, Rotterdam, the Netherlands, www.growthanalyser.org).
All children underwent a DXA-scan (dual-energy X-ray absorptiometry scan, type Lunar-Prodigy; GE Healthcare, Chalfont St. Giles, UK) to further describe the fat distribution of the child. The fat mass was assessed and the percentage fat mass (fat mass in grams total body / fat mass in grams total body + lean mass in grams total body) and trunk fat ratio (fat mass in grams trunk/ fat mass in grams total body) were calculated. All scans were made with the same machine, and quality assurance was performed daily. Coefficient of variation was 1.2% for the total fat mass. Fat mass and the percentage fat mass distribution were both transformed into SDS for age and gender [29,30,31,32].
Lipid profile
Fasting levels of high-density lipoprotein (HDL), triglycerides (TG), and total cholesterol were measured on a Roche modular P analyser (Roche Diagnostics, Almere, The Netherlands), with the following intra- and inter-assay coefficient of variation: HDL, intra = 0.6% and inter = 0.9%; TG, intra = 0.7% and inter = 1.9%; total cholesterol, intra = 1.1%, and inter = 1.6%.
Statistical analysis
The main purpose of our study was to assess the difference in insulin resistance in children with and without early exposure to prednisone in utero. Unpaired Student’s t-tests were performed to assess the differences between the exposed and the non-exposed group in clinical characteristics, insulin resistance (HOMA-IR and serum adiponectin), differences in lipid profiles (high-density lipoprotein, triglycerides, and total cholesterol), and differences in body fat distribution (total fat mass percentage fat, trunk fat ratio, skinfolds, and body circumference). In these analyses, prednisone use was entered as a dichotomous variable, ever use or no use.
Multivariate linear regression models were used to describe the association between HOMA-IR, plasma adiponectin, trunk fat ratio, and the maternal prednisone use during pregnancy. In these models, we added gender, age, and RA disease activity during pregnancy and also included all variables that were statistically different between the prednisone-exposed and non-exposed group. All variables were entered simultaneously in the model.
Finally, to investigate if there was a prednisone dose effect, the prednisone dose was entered as a continues variable in the third model. To determine whether the impact of the use of prednisone was greater when used early in in pregnancy, the analyses were also performed with entering prednisone use in first trimester, instead of prednisone use during the entire pregnancy. All statistical analyses were performed using STATA software (version 12.0 for Mac; StataCorp LP, Texas, USA). Statistical significance was defined as p < 0.05.
Results
Pregnancy outcome measures
Prednisone was used by 41% (42/103) of the mothers during pregnancy. Of the 42 women that used prednisone, two mothers stopped prednisone after the first trimester and five mothers started. This resulted in 83% (35/42) of the women continuing their prednisone throughout the entire pregnancy. The median prednisone dose was 6.0 mg/day (IQR: 1–15 mg). Other medication included sulfasalazine 33% (34/103) and hydroxychloroquine 2% (2/103), sometimes in combination with prednisone. The median dose of sulfasalazine was 2000 mg/day (range 500–4000 mg) (Table 1). In total, RA medication was used by 47% (48/103) of the mothers during pregnancy.
Mean DAS28 (SD) was significantly higher in women who used prednisone during pregnancy. In first trimester, DAS28 was 4.26 (1.28) in the prednisone-exposed group and 3.25 (0.97) in the non-exposed (p < 0.001). In third trimester, the RA disease activity declined in both groups to, 3.74 (1.19) and 3.07 (1.07), respectively (p < 0.01). The mean gestational age (SD) was 39.1 (1.89) weeks in the prednisone-expose and 39.7 (1.75) in the non-exposed (p- = 0.12). Mean (SD) birth weight SDS was − 0.03 (1.06) in the prednisone exposed group and 0.11 (1.18) in the non-exposed (p = 0.53) (Table 1). Less than 5% (4/103) of the mothers smoked during pregnancy of which only 1 mother used prednisone.
Clinical outcome measures of children during follow-up study
At the follow-up visits of the children, the mean age (SD) in the prednisone-exposed group was 6.78 (1.14) years and in the non-exposed 7.04 (1.32) years (p: 0.30). The mean weight SDS, height SDS, and BMI SDS (SD) did not differ between the 2 groups (Table 1).
Insulin resistance outcome measures
HOMA-IR
No difference in fasting glucose, insulin levels, or HOMA-IR was observed between the children who were in utero exposed to prednisone and those who were not exposed. The mean (SD) fasting glucose level was 4.87 (0.37) mmol/L in the children exposed to prednisone and 4.94 (0.42) in the non-exposed. Fasting insulin was 4.95 (3.57) µU/mL and 4.92 (2.03) µU/mL, respectively. A total of 2.9% (3/103) of children had mild fasting hyperglycaemia (> 5.6 mmol/L) and normal fasting plasma insulin levels, but none of these children had been exposed to prednisone in utero. The median (SD) HOMA-IR score was 1.10 (0.84) in the children exposed to prednisone and 1.09 (0.49) in the non-exposed (Table 2). Four children had a HOMA-IR ≥ 2.5 (3.9%) of whom 3 were exposed to prednisone in utero. The prednisone dose of the 3 children who were exposed was low, 2.5, 3.5, and 4.0 mg prednisone per day, respectively. There was no difference between the presence of HOMA-IR (≥ 2.5) in the prednisone-exposed and non-exposed group (p = 0.16).
The multivariate linear regression model showed no association between maternal prednisone use during pregnancy and the HOMA-IR of the offspring. Age was associated with the HOMA-IR, ß = 0.12, p < 0.01 (Table 3).
Adiponectin
Children exposed to prednisone in utero had higher serum levels of adiponectin, but not significantly (p = 0.17). The mean (SD) adiponectin level was 16.5 (4.1) mg/L in the children exposed to prednisone and 15.4 (3.6) mg/L in the non-exposed. We did find a higher adiponectin levels in girls 16.7 (4.0) mg/L than in boys 15.1 (3.5) mg/L (p < 0.03).
The multivariate linear regression model showed no association between maternal prednisone use during pregnancy and serum adiponectin levels of the offspring. Gender was again associated with the adiponectin level, ß = 1.70, p < 0.03 (Table 3), indicating that girls have higher adiponectin levels than boys.
Fat distribution
No difference in weight, height, or fat distribution including total fat mass, percentage fat, trunk fat ratio, skinfolds, or body circumference was observed between the children who were in utero exposed to prednisone and the children who were not exposed. The mean fat mass SDS (SD) was 0.09 (1.01) in the prednisone-exposed children and 0.26 (0.89) in the non-exposed. The trunk fat ratio was 0.36 (0.04) and 0.35 (0.04), respectively. The ratio skinfolds trunk (subscapular + suprailiac) to peripheral (triceps + biceps) was 0.11 (1.76) in the prednisone-exposed children and 0.64 (1.18) in the non-exposed (Table 2).
Skinfolds were all within the normal range and similar to the reference mean, except for the suprailiac skinfold, which was significantly lower than the mean of healthy controls (− 1.61 (0.98) SDS, p < 0.001) (Table 2). Circumference of the arm, waist, and hip was also all within the normal range and similar to the reference mean. The waist to hip ratio (SD) was 1.03 (0.92) in the prednisone-exposed children and 0.96 (0.93) in the non-exposed (Table 2).
The multivariate linear regression model showed no association between maternal prednisone use during pregnancy and trunk fat ratio of the offspring. Age was associated with the trunk fat ratio (ß = 0.01, p < 0.01) (Table 3).
Other outcome measures
Lipid profile
The mean total cholesterol (SD) was 4.51 (0.79) mmol/L in the prednisone-exposed group and 4.35 (0.58) mmol/L in the non-exposed. Also, the fasting triglyceride level and HDL level did not differ in the prednisone-exposed or non-exposed group (Table 2).
Prednisone dose
In the final models in Table 3, prednisone use during pregnancy was entered as a dichotomous variable (yes/no). When we entered the prednisone medication dose as a continues variable, no association was present between the HOMA-IR (p = 0.81), adiponectin level (p = 0.50), or trunk fat ratio (p = 0.56). We therefore concluded that there was no prednisone dose effect. It was not possible to investigate if there was a difference between prednisone use only in first trimester and prednisone use during the entire pregnancy because 84% of the women continued their prednisone throughout the entire pregnancy. Only two women stopped their prednisone after the first trimester and five started prednisone after the first trimester.
Discussion
Children born from mothers with RA and in utero exposed to prednisone had no signs of insulin resistance at the age of approximately 7 years. Our hypothesis that prednisone-exposure in the first trimester of pregnancy is associated with early determinants of insulin resistance in the offspring is therefore refuted. This conclusion is reassuring because the prednisone use during pregnancy is increasing worldwide not only in patients with RA.
Interpretation of the date
Our conclusion is mainly based on the HOMA-IR, which was similar between the exposed and non-exposed. Furthermore, both groups did not differ significantly from 1.00, which is the normal value for the HOMA-IR. HOMA-IR is an appropriate method to measure insulin resistance among healthy children. The method is preferred above other fasting methods like the fasting glucose/insulin ratio (FGIR) or quantitative insulin sensitivity check index (QUICKI) [10, 11]. In line with literature, the HOMA-IR logscore was positively associated with the BMI of the child [33].
In our population, the children who were in utero exposed to synthetic glucocorticoids had similar adiponectin levels than the non-exposed. Adiponectin is mainly secreted by white adipose tissue, but expression can also be found in bone marrow, osteoblasts, and fetal tissue [34]. Circulating adiponectin concentration can be regulated by various hormonal, nutritional, and pharmacological factors, but can be downregulated by prolactin, growth hormone, and glucocorticoids [35, 36]. Furthermore, pro-inflammatory cytokines such as tumor necrosis factor α (TNFα) and interleukin-6 (IL-6) are potent inhibitors of adiponectin gene expression [36]. Adiponectin plays a role in fetal growth. In the beginning of pregnancy, maternal adiponectin levels increase and later in pregnancy the levels decrease proportionally to weight gain and the physiological decline in insulin resistance [34].
In our study population, we found a gender difference in adiponectin plasma concentration. The mean adiponectin level was higher in girls than in boys. Literature described this difference, although it was reported that the difference usually starts after puberty [37, 38]. Even though our study population was at prepubertal age, we had the same observation of a significant higher adiponectin level in the girls. Gender was also the only significant determinant of adiponectin in the multivariate analyses.
Glucocorticoids regulate multiple steps in the process of adipogenesis. They play an important role in the development of obesity, particularity fat deposits in the trunk and the pathogenesis of obesity related diseases [22]. Consequently, when investigating insulin resistance, the trunk fat ratio needs to be taken into account. Children exposed in utero to prednisone had similar body fat percentage and fat distribution compared to children without prednisone-exposure, and compared to the normal population. These findings are reassuring, because these variables have a great predictive value on the fat mass throughout adulthood [39, 40].
Strength and limitations
The main strength of this study is that all pregnancies were prospectively followed. Medication intake and RA disease activity was followed throughout the entire pregnancy and always assessed by the same research assistants. Also all data concerning the prepubertal children were measured and collected by one doctor to preserve the continuity. Although only 54% of all eligible children participated, there was no statistical difference between the participating and non-participating group (Supplementary Table). We conducted a nationwide study, but all children had to be seen Sophia Children’s Hospital in Rotterdam. Main reason for non-participation was the distance to the hospital (38%). Other reason was that parents felt that our investigations were too much of a burden for their child (30%). Another limitation could be that no hyperinsulinemic euglycemic clamp (HEC), intravenous, or oral glucose tolerance test (OGTT) was used to quantify the insulin resistance. Taking our objective, we used the less-invasive and therefore ethically approved HOMA-IR calculation to assess the insulin resistances in this healthy study population between 5 and 10 years old [10]. Several studies have shown a reasonable correlation between HOMA-IR levels and results from HEC measurements or OGTT [41,42,43,44].
Use of prednisone during pregnancy has been rapidly growing over the past decade [1]. This use is associated with maternal and fetal adverse outcomes. The aim of this study was to explore an association between prednisone use during early pregnancy and the risk of insulin resistance later in life of the offspring. We can now conclude that children who are exposed to “low dose” of synthetic glucocorticoids in utero have no higher risk for insulin resistance at the age of approximately 7 years. Nevertheless, further research has to be performed to evaluate if these risk factors remain absent in the future.
References
Cai E, Czuzoj-Shulman N, Abenhaim HA (2021) Maternal and fetal outcomes in pregnancies with long-term corticosteroid use. J Matern Fetal Neonatal Med 34(11):1797–1804. https://doi.org/10.1080/14767058.2019.1649392 (publishedOnlineFirst:2019/08/21)
de Man YA, Hazes JM, van der Heide H et al (2009) Association of higher rheumatoid arthritis disease activity during pregnancy with lower birth weight: results of a national prospective study. Arthritis Rheum 60(11):3196–3206. https://doi.org/10.1002/art.24914 (publishedOnlineFirst:2009/10/31)
de Steenwinkel FD, Hokken-Koelega AC, de Ridder MA et al (2014) Rheumatoid arthritis during pregnancy and postnatal catch-up growth in the offspring. Arthritis Rheumatol 66(7):1705–1711. https://doi.org/10.1002/art.38519
Kerkhof GF, Willemsen RH, Leunissen RW et al (2012) Health profile of young adults born preterm: negative effects of rapid weight gain in early life. J Clin Endocrinol Metab 97(12):4498–4506. https://doi.org/10.1210/jc.2012-1716 (published Online First: 2012/09/21)
de Man YA, Dolhain RJ, van de Geijn FE et al (2008) Disease activity of rheumatoid arthritis during pregnancy: results from a nationwide prospective study. Arthritis Rheum 59(9):1241–1248
Li XQ, Zhu P, Myatt L et al (2014) Roles of glucocorticoids in human parturition: a controversial fact? Placenta 35(5):291–296. https://doi.org/10.1016/j.placenta.2014.03.005 (published Online First: 2014/04/01)
Cottrell EC, Seckl JR (2009) Prenatal stress, glucocorticoids and the programming of adult disease. Front Behav Neurosci 3:19. https://doi.org/10.3389/neuro.08.019.2009
O’Connor TG, Ben-Shlomo Y, Heron J et al (2005) Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biol Psychiatry 58(3):211–217. https://doi.org/10.1016/j.biopsych.2005.03.032
Moisiadis VG, Matthews SG (2014) Glucocorticoids and fetal programming part 2: mechanisms. Nat Rev Endocrinol 10(7):403–411. https://doi.org/10.1038/nrendo.2014.74 (published Online First: 2014/05/28)
Borai A, Livingstone C, Kaddam I et al (2011) Selection of the appropriate method for the assessment of insulin resistance. BMC Med Res Methodol 11:158. https://doi.org/10.1186/1471-2288-11-158
Keskin M, Kurtoglu S, Kendirci M et al (2005) Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics 115(4):e500–e503. https://doi.org/10.1542/peds.2004-1921
Lihn AS, Pedersen SB, Richelsen B (2005) Adiponectin: action, regulation and association to insulin sensitivity. Obes Rev 6(1):13–21. https://doi.org/10.1111/j.1467-789X.2005.00159.x (published Online First: 2005/01/19)
Arita Y, Kihara S, Ouchi N et al (2002) Adipocyte-derived plasma protein adiponectin acts as a platelet-derived growth factor-BB-binding protein and regulates growth factor-induced common postreceptor signal in vascular smooth muscle cell. Circulation 105(24):2893–2898
Koerner A, Kratzsch J, Kiess W (2005) Adipocytokines: leptin–the classical, resistin–the controversical, adiponectin–the promising, and more to come. Best Pract Res Clin Endocrinol Metab 19(4):525–546. https://doi.org/10.1016/j.beem.2005.07.008
Yamauchi T, Kamon J, Waki H et al (2003) Globular adiponectin protected ob/ob mice from diabetes and ApoE-deficient mice from atherosclerosis. J Biol Chem 278(4):2461–2468. https://doi.org/10.1074/jbc.M209033200
de Man YA, Hazes JM, van de Geijn FE et al (2007) Measuring disease activity and functionality during pregnancy in patients with rheumatoid arthritis. Arthritis Rheum 57(5):716–722
Van Riel P, van Gestel A, Scott D (2000) Interpreting disease course. In: van Riel P, Van Gestel A, Scott D (eds) Eular handbook of clinical assessments in rheumatoid arthritis. Van Zuiden Communications B.V, Alphen aan den Rijn, pp 39–43
Niklasson A, Ericson A, Fryer JG et al (1991) An update of the Swedish reference standards for weight, length and head circumference at birth for given gestational age (1977–1981). Acta Paediatr Scand 80(8–9):756–762
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27(6):1487–1495. (published Online First: 2004/05/27)
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Patel P, Abate N (2013) Body fat distribution and insulin resistance. Nutrients 5(6):2019–2027. https://doi.org/10.3390/nu5062019
Lee MJ, Pramyothin P, Karastergiou K et al (2013) Deconstructing the roles of glucocorticoids in adipose tissue biology and the development of central obesity. Biochim Biophys Acta. https://doi.org/10.1016/j.bbadis.2013.05.029 (publishedOnlineFirst:2013/06/06)
Tchernof A, Despres JP (2013) Pathophysiology of human visceral obesity: an update. Physiol Rev 93(1):359–404. https://doi.org/10.1152/physrev.00033.2011 (publishedOnlineFirst:2013/01/11)
Lee MJ, Wu Y, Fried SK (2013) Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med 34(1):1–11. https://doi.org/10.1016/j.mam.2012.10.001 (publishedOnlineFirst:2012/10/17)
Ohashi N, Ito C, Fujikawa R et al (2009) The impact of visceral adipose tissue and high-molecular weight adiponectin on cardio-ankle vascular index in asymptomatic Japanese subjects. Metabolism 58(7):1023–1029. https://doi.org/10.1016/j.metabol.2009.03.005 (publishedOnlineFirst:2009/04/21)
Indulekha K, Surendar J, Anjana RM et al (2012) Circulating levels of high molecular weight (HMW) adiponectin and total adiponectin in relation to fat distribution, oxidative stress and inflammation in Asian Indians. Dis Markers 33(4):185–192. https://doi.org/10.3233/DMA-2012-0924 (publishedOnlineFirst:2012/09/11)
Gerver WJM dBB (2001) Paeditric morphometrics: a reference manual. University Press Maastricht, Maastricht
Talma H BB, HiraSing RA, van Buuren S (2010) Groeidiagrammen 2010 Handleiding bij het meten en wegen van kinderen en het invullen van groeidiagrammen. Leiden, the Netherlands
Bonnick SL, Johnston CC Jr, Kleerekoper M et al (2001) Importance of precision in bone density measurements. J Clin Densitom 4(2):105–110. (publishedOnlineFirst:2001/07/31)
Kiebzak GM, Leamy LJ, Pierson LM et al (2000) Measurement precision of body composition variables using the lunar DPX-L densitometer. J Clin Densitom 3(1):35–41. (publishedOnlineFirst:2000/04/04)
Shepherd JA, Fan B, Lu Y et al (2006) Comparison of BMD precision for Prodigy and Delphi spine and femur scans. Osteoporos Int 17(9):1303–1308. https://doi.org/10.1007/s00198-006-0127-9 (publishedOnlineFirst:2006/07/11)
Boot AM, Bouquet J, de Ridder MA et al (1997) Determinants of body composition measured by dual-energy X-ray absorptiometry in Dutch children and adolescents. Am J Clin Nutr 66(2):232–8 (published Online First: 1997/08/01)
Whitrow MJ, Davies MJ, Giles LC et al (2013) Effects of birth size, post-natal growth and current size on insulin resistance in 9-year-old children: a prospective cohort study. Eur J Pediatr. https://doi.org/10.1007/s00431-013-2017-4
Brochu-Gaudreau K, Rehfeldt C, Blouin R et al (2010) Adiponectin action from head to toe. Endocrine 37(1):11–32. https://doi.org/10.1007/s12020-009-9278-8
Fasshauer M, Klein J, Kralisch S et al (2004) Growth hormone is a positive regulator of adiponectin receptor 2 in 3T3-L1 adipocytes. FEBS Lett 558(1–3):27–32. https://doi.org/10.1016/S0014-5793(03)01525-4
Fasshauer M, Klein J, Neumann S et al (2002) Hormonal regulation of adiponectin gene expression in 3T3-L1 adipocytes. Biochem Biophys Res Commun 290(3):1084–1089. https://doi.org/10.1006/bbrc.2001.6307
Al-Daghri NM, Al-Attas OS, Alokail MS et al (2011) Gender differences exist in the association of leptin and adiponectin levels with insulin resistance parameters in prepubertal Arab children. J Pediatr Endocrinol Metab 24(7–8):427–432
Combs TP, Berg AH, Rajala MW et al (2003) Sexual differentiation, pregnancy, calorie restriction, and aging affect the adipocyte-specific secretory protein adiponectin. Diabetes 52(2):268–276
Morrison JA, Friedman LA, Wang P et al (2008) Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr 152(2):201–206. https://doi.org/10.1016/j.jpeds.2007.09.010
Cnop M, Vidal J, Hull RL et al (2007) Progressive loss of beta-cell function leads to worsening glucose tolerance in first-degree relatives of subjects with type 2 diabetes. Diabetes Care 30(3):677–682. https://doi.org/10.2337/dc06-1834 (publishedOnlineFirst:2007/03/01)
Laakso M (1993) How good a marker is insulin level for insulin resistance? Am J Epidemiol 137(9):959–65 (published Online First: 1993/05/01)
Atabek ME, Pirgon O (2007) Assessment of insulin sensitivity from measurements in fasting state and during an oral glucose tolerance test in obese children. J Pediatr Endocrinol Metab 20(2):187–95 (published Online First: 2007/04/03)
Quon MJ (2001) Limitations of the fasting glucose to insulin ratio as an index of insulin sensitivity. J Clin Endocrinol Metab 86(10):4615–7 (published Online First: 2001/10/16)
Gungor N, Saad R, Janosky J et al (2004) Validation of surrogate estimates of insulin sensitivity and insulin secretion in children and adolescents. J Pediatr 144(1):47–55. https://doi.org/10.1016/j.jpeds.2003.09.045 (publishedOnlineFirst:2004/01/15)
Acknowledgements
We would like to thank all parents and their children for their voluntary contributions. We would like to emphasize the great effort made by Dr. Y.A. de Man and Dr. F.E. van de Geijn in obtaining most the PARA data. We are grateful to the research assistants, for data collection, and all laboratory technicians, for their assistance with laboratory research.
Funding
This study was supported by the Dutch Arthritis Association (Reumafonds), a non-profit fund-raising organization (DAA 08–1-306). The sponsors had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Steenwinkel, F.D.O., Dolhain, R.J.E.M., Hazes, J.M.W. et al. Does prednisone use in pregnant women with rheumatoid arthritis induce insulin resistance in the offspring?. Clin Rheumatol 42, 47–54 (2023). https://doi.org/10.1007/s10067-022-06347-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-022-06347-0