Abstract
Objective
To identify clinical characteristics and risk factors related to the progression of interstitial lung disease (ILD) in patients with primary Sjögren’s syndrome (pSS).
Methods
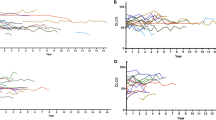
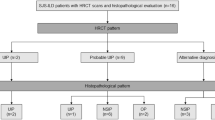
In this single-centered, retrospective study, a total of 83 identified pSS-ILD patients with relatively complete clinical data were finally enrolled. Clinical symptoms, laboratory data, high-resolution computed tomography (HRCT), and pulmonary function test (PFT) results were collected. A logistic regression analysis was performed to determine the independent risk factors for ILD progression, and a nomogram was plotted to construct a predictive model.
Results
The prevalence of pSS-ILD in our study was 18.89%. Among the 83 enrolled patients, 32 (38.6%) underwent ILD progression. The characteristic features associated with the progression of ILD included male sex, non-sicca onset, reticular pattern on HRCT, higher levels of baseline lactic dehydrogenase (LDH), and low baseline forced vital capacity (FVC). The results of multivariate logistic regression indicated that LDH (OR 1.008, p = 0.030) was an independent risk factor for ILD progression, while sicca onset (OR 0.254, p = 0.044) and FVC (OR 0.952, p = 0.003) were protective factors for ILD progression. A simple predictive model for ILD progression in pSS was developed and validated.
Conclusion
pSS patients with non-sicca onset, high baseline LDH level, and low baseline FVC were at higher risk of ILD progression.
Key Points • Male sex and reticular pattern in HRCT are more common in pSS patients with progressive ILD compared to those with stable ILD. • Non-sicca onset, high baseline LDH level, and low baseline FVC are independent risk factors of pSS-ILD progression. |



Similar content being viewed by others
References
Mariette X, Criswell LA (2018) Primary Sjogren’s syndrome. N Engl J Med 378:931–939. https://doi.org/10.1056/NEJMcp1702514
Flament T, Bigot A, Chaigne B, Henique H, Diot E, Marchand-Adam S (2016) Pulmonary manifestations of Sjogren’s syndrome. Eur Respir Rev 25:110–123. https://doi.org/10.1183/16000617.0011-2016
Peredo RA, Beegle S (2021) Sjogren’s syndrome and pulmonary disease. Adv Exp Med Biol 1303:193–207. https://doi.org/10.1007/978-3-030-63046-1_12
Reina D, Roig Vilaseca D, Torrente-Segarra V et al (2016) Sjogren’s syndrome-associated interstitial lung disease: a multicenter study. Reumatol Clin 12:201–205. https://doi.org/10.1016/j.reuma.2015.09.003
Zhao R, Wang Y, Zhou W et al (2020) Associated factors with interstitial lung disease and health-related quality of life in Chinese patients with primary Sjogren’s syndrome. Clin Rheumatol 39:483–489. https://doi.org/10.1007/s10067-019-04753-5
Gao H, Zhang XW, He J et al (2018) Prevalence, risk factors, and prognosis of interstitial lung disease in a large cohort of Chinese primary Sjogren syndrome patients: a case-control study. Medicine (Baltimore) 97:e11003. https://doi.org/10.1097/MD.0000000000011003
Buvry C, Cassagnes L, Tekath M et al (2020) Anti-Ro52 antibodies are a risk factor for interstitial lung disease in primary Sjogren syndrome. Respir Med 163:105895. https://doi.org/10.1016/j.rmed.2020.105895
Luppi F, Sebastiani M, Silva M et al (2020) Interstitial lung disease in Sjogren’s syndrome: a clinical review. Clin Exp Rheumatol 38(Suppl 126):291–300
Li X, Xu B, Ma Y et al (2015) Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: a retrospective analysis of 315 patients. Int J Rheum Dis 18:439–446. https://doi.org/10.1111/1756-185X.12583
Roca F, Dominique S, Schmidt J et al (2017) Interstitial lung disease in primary Sjogren’s syndrome. Autoimmun Rev 16:48–54. https://doi.org/10.1016/j.autrev.2016.09.017
Kamiya Y, Fujisawa T, Kono M et al (2019) Prognostic factors for primary Sjogren’s syndrome-associated interstitial lung diseases. Respir Med 159:105811. https://doi.org/10.1016/j.rmed.2019.105811
Zhang T, Yuan F, Xu L, Sun W, Liu L, Xue J (2020) Characteristics of patients with primary Sjogren’s syndrome associated interstitial lung disease and relevant features of disease progression. Clin Rheumatol 39:1561–1568. https://doi.org/10.1007/s10067-019-04906-6
Vitali C, Bombardieri S, Jonsson R et al (2002) Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61:554–558. https://doi.org/10.1136/ard.61.6.554
Dong X, Zhou J, Guo X et al (2018) A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjogren’s syndrome-related interstitial lung disease in a Chinese population. Clin Rheumatol 37:2981–2988. https://doi.org/10.1007/s10067-018-4289-6
Enomoto Y, Takemura T, Hagiwara E et al (2013) Prognostic factors in interstitial lung disease associated with primary Sjogren’s syndrome: a retrospective analysis of 33 pathologically-proven cases. PLoS ONE 8:e73774. https://doi.org/10.1371/journal.pone.0073774
Travis WD, Hunninghake G, King TE Jr et al (2008) Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med 177:1338–1347. https://doi.org/10.1164/rccm.200611-1685OC
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824. https://doi.org/10.1164/rccm.2009-040GL
Gupta S, Ferrada MA, Hasni SA (2019) Pulmonary manifestations of primary Sjogren’s syndrome: underlying immunological mechanisms, clinical presentation, and management. Front Immunol 10:1327. https://doi.org/10.3389/fimmu.2019.01327
Sambataro G, Ferro F, Orlandi M et al (2020) Clinical, morphological features and prognostic factors associated with interstitial lung disease in primary Sjgren’s syndrome: a systematic review from the Italian Society of Rheumatology. Autoimmun Rev 19:102447. https://doi.org/10.1016/j.autrev.2019.102447
Spagnolo P, Lee JS, Sverzellati N, Rossi G, Cottin V (2018) The lung in rheumatoid arthritis: focus on interstitial lung disease. Arthritis Rheumatol 70:1544–1554. https://doi.org/10.1002/art.40574
Khanna D, Tashkin DP, Denton CP, Renzoni EA, Desai SR, Varga J (2020) Etiology, risk factors, and biomarkers in systemic sclerosis with interstitial lung disease. Am J Respir Crit Care Med 201:650–660. https://doi.org/10.1164/rccm.201903-0563CI
Chung A, Wilgus ML, Fishbein G, Lynch JP 3rd (2019) Pulmonary and bronchiolar involvement in Sjogren’s syndrome. Semin Respir Crit Care Med 40:235–254. https://doi.org/10.1055/s-0039-1688448
Fu Q, Wang L, Li L, Li Y, Liu R, Zheng Y (2019) Risk factors for progression and prognosis of rheumatoid arthritis-associated interstitial lung disease: single center study with a large sample of Chinese population. Clin Rheumatol 38:1109–1116. https://doi.org/10.1007/s10067-018-4382-x
Khanna D, Mittoo S, Aggarwal R et al (2015) Connective tissue disease-associated interstitial lung diseases (CTD-ILD) - report from OMERACT CTD-ILD Working Group. J Rheumatol 42:2168–2171. https://doi.org/10.3899/jrheum.141182
Uffmann M, Kiener HP, Bankier AA, Baldt MM, Zontsich T, Herold CJ (2001) Lung manifestation in asymptomatic patients with primary Sjogren syndrome: assessment with high resolution CT and pulmonary function tests. J Thorac Imaging 16:282–289. https://doi.org/10.1097/00005382-200110000-00009
Flaherty KR, Wells AU, Cottin V et al (2019) Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med 381:1718–1727. https://doi.org/10.1056/NEJMoa1908681
Wu W, Guo L, Fu Y et al (2021) Interstitial lung disease in Anti-MDA5 positive dermatomyositis. Clin Rev Allergy Immunol 60:293–304. https://doi.org/10.1007/s12016-020-08822-5
du Bois RM, Weycker D, Albera C et al (2011) Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 184:459–466. https://doi.org/10.1164/rccm.201011-1790OC
Ciancio N, Pavone M, Torrisi SE et al (2019) Contribution of pulmonary function tests (PFTs) to the diagnosis and follow up of connective tissue diseases. Multidiscip Respir Med 14:17. https://doi.org/10.1186/s40248-019-0179-2
Kusume K (1991) Lung injury in idiopathic pulmonary fibrosis and measurement of immunoreactive neutrophil elastase and alpha 1-protease inhibitor in blood. Nihon Kyobu Shikkan Gakkai Zasshi 29:1254–1260
Li L, Liu R, Zhang Y et al (2020) A retrospective study on the predictive implications of clinical characteristics and therapeutic management in patients with rheumatoid arthritis-associated interstitial lung disease. Clin Rheumatol 39:1457–1470. https://doi.org/10.1007/s10067-019-04846-1
Kamiya H, Panlaqui OM (2020) Systematic review and meta-analysis of prognostic factors of acute exacerbation of idiopathic pulmonary fibrosis. BMJ Open 10:e035420. https://doi.org/10.1136/bmjopen-2019-035420
Manfredi A, Sebastiani M, Cerri S et al (2017) Prevalence and characterization of non-sicca onset primary Sjogren syndrome with interstitial lung involvement. Clin Rheumatol 36:1261–1268. https://doi.org/10.1007/s10067-017-3601-1
Gao H, Zou YD, Zhang XW et al (2018) Interstitial lung disease in non-sicca onset primary Sjogren’s syndrome: a large-scale case-control study. Int J Rheum Dis 21:1423–1429. https://doi.org/10.1111/1756-185X.13334
du Bois RM, Albera C, Bradford WZ et al (2014) 6-Minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur Respir J 43:1421–1429. https://doi.org/10.1183/09031936.00131813
Vandecasteele E, De Pauw M, De Keyser F et al (2016) Six-minute walk test in systemic sclerosis: a systematic review and meta-analysis. Int J Cardiol 212:265–273. https://doi.org/10.1016/j.ijcard.2016.03.084
Santus P, Radovanovic D, Frassanito F, Cristiano A, Rizzi M (2017) Is the six-minute walk test useful or useless in systemic sclerosis? Eur J Intern Med 43:e37–e39. https://doi.org/10.1016/j.ejim.2017.05.018
Pugnet G, Marjanovic Z, Deligny C et al (2018) Reproducibility and utility of the 6-minute walk test in systemic sclerosis. J Rheumatol 45:1273–1280. https://doi.org/10.3899/jrheum.170994
Funding
This study was supported by the grants from the National Natural Science Foundation (U1704177 and 8187811).
Author information
Authors and Affiliations
Contributions
TFL contributed to the study conception and design. YJH and XL contributed to the acquisition of data. SHH, KJG, and SSL analyzed the data. SHH drafted the manuscript. YJH and TFL revised the manuscript. All authors approved the final version of the manuscript to be published.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Written informed consent was not required owing to the retrospective nature of the study.
Disclosures
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, SH., He, YJ., Guo, KJ. et al. Risk factors for progression of interstitial lung disease in Sjögren’s syndrome: a single-centered, retrospective study. Clin Rheumatol 41, 1153–1161 (2022). https://doi.org/10.1007/s10067-021-05984-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05984-1