Abstract
Objective
Connective tissue disease (CTD) might occur during the course of idiopathic pulmonary fibrosis (IPF). Clinical factors associated with CTD development in IPF patients have still not been identified. We investigated which antibodies have a significant association with the development of CTD during the clinical course of IPF.
Methods
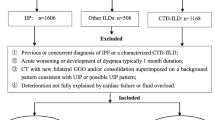
We retrospectively reviewed the records of 527 patients with a first diagnosis of IPF between January 2007 and March 2014 and investigated the time to CTD development after IPF diagnosis in these patients.
Results
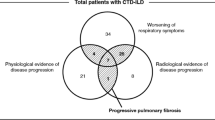
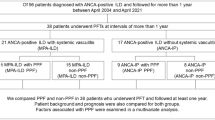
CTD developed in 15 patients at a median of 2.1 years (range 1.2–4.8) after IPF diagnosis. All patients had anti-neutrophil cytoplasmic antibodies (ANCA) or autoantibodies that met the serology criteria for interstitial pneumonia with autoimmune features (IPAF). Survival duration for IPF patients with progression to CTD was 5.3 (3.8, 6.7) years, which was significantly longer than for IPF patients without progression to CTD [2.9 (1.7, 4.8), p = 0.001]. Independent risk factors for CTD development in IPF patients included female gender [adjusted hazard ratio (HR) 5.319, p = 0.0082], titer of rheumatoid factor (RF; adjusted HR, 1.006; p = 0.022), titer of anti-citrullinated protein antibody (ACPA; adjusted HR, 1.009; p = 0.0011), and titer of myeloperoxidase (MPO)-ANCA (adjusted HR, 1.02; p < 0.0001).
Conclusion
Progression to CTD is uncommon in IPF patients. However, a significant number of IPF patients with high titers of RF, ACPA, or MPO-ANCA progressed to CTD. RF, ACPA, and MPO-ANCA might be significantly associated with CTD development in IPF patients.
Key Points • A significant number of IPF patients with high titers of RF, ACPA, or MPO-ANCA progressed to CTD. • IPF/UIP with high titers of RF, ACPA, or MPO-ANCA might be the initial clinical manifestation of CTD. • RF, ACPA, and MPO-ANCA may be significantly associated with the development of pulmonary fibrosis in patients with CTD. |


Similar content being viewed by others
Data availability
Upon a reasonable request, the authors are be prepared to send relevant documentation or data.
Change history
15 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10067-021-05732-5
References
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier JF, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King te Jr, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ, ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183(6):788–824
Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, Behr J, Cottin V, Danoff SK, Morell F, Flaherty KR, Wells A, Martinez FJ, Azuma A, Bice TJ, Bouros D, Brown KK, Collard HR, Duggal A, Galvin L, Inoue Y, Jenkins RG, Johkoh T, Kazerooni EA, Kitaichi M, Knight SL, Mansour G, Nicholson AG, Pipavath SNJ, Buendía-Roldán I, Selman M, Travis WD, Walsh S, Wilson KC, American Thoracic Society, European Respiratory Society, Japanese Respiratory Society, and Latin American Thoracic Society (2018) Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 198(5):e44–e68
Song JW, Do KH, Kim MY, Jang SJ, Colby TV, Kim DS (2009) Pathologic and radiologic differences between idiopathic and collagen vascular disease-related usual interstitial pneumonia. Chest. 136(1):23–30
Liu GY, Ventura IB, Achtar-Zadeh N, Elicker BM, Jones KD, Wolters PJ, Collard HR, Adegunsoye A, Strek ME, Ley B (2019) Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in North American patients with idiopathic pulmonary fibrosis. Chest. 156(4):715–723
Ando M, Miyazaki E, Ishii T, Mukai Y, Yamasue M, Fujisaki H, Ito T, Nureki SI, Kumamoto T (2013) Incidence of myeloperoxidase anti-neutrophil cytoplasmic antibody positivity and microscopic polyangitis in the course of idiopathic pulmonary fibrosis. Respir Med 107(4):608–615
Kagiyama N, Takayanagi N, Kanauchi T, Ishiguro T, Yanagisawa T, Sugita Y (2015) Antineutrophil cytoplasmic antibody-positive conversion and microscopic polyangiitis development in patients with idiopathic pulmonary fibrosis. BMJ Open Respir Res 2(1):e000058
Hosoda C, Baba T, Hagiwara E, Ito H, Matsuo N, Kitamura H, Iwasawa T, Okudela K, Takemura T, Ogura T (2016) Clinical features of usual interstitial pneumonia with anti-neutrophil cytoplasmic antibody in comparison with idiopathic pulmonary fibrosis. Respirology. 21(5):920–926
Moua T, Zamora Martinez AC, Baqir M, Vassallo R, Limper AH, Ryu JH (2014) Predictors of diagnosis and survival in idiopathic pulmonary fibrosis and connective tissue disease-related usual interstitial pneumonia. Respir Res 15:154
Park JH, Kim DS, Park IN, Jang SJ, Kitaichi M, Nicholson AG, Colby TV (2007) Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease-related subtypes. Am J Respir Crit Care Med 175(7):705–711
Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, Arriola E, Silver R, Strange C, Bolster M, Seibold JR, Riley DJ, Hsu VM, Varga J, Schraufnagel DE, Theodore A, Simms R, Wise R, Wigley F, White B, Steen V, Read C, Mayes M, Parsley E, Mubarak K, Connolly MK, Golden J, Olman M, Fessler B, Rothfield N, Metersky M (2006) Cyclophosphamide versus placebo in scleroderma lung disease. N Engl J Med 354(25):2655–2666
Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, Goldin J, Arriola E, Volkmann ER, Kafaja S, Silver R, Steen V, Strange C, Wise R, Wigley F, Mayes M, Riley DJ, Hussain S, Assassi S, Hsu VM, Patel B, Phillips K, Martinez F, Golden J, Connolly MK, Varga J, Dematte J, Hinchcliff ME, Fischer A, Swigris J, Meehan R, Theodore A, Simms R, Volkov S, Schraufnagel DE, Scholand MB, Frech T, Molitor JA, Highland K, Read CA, Fritzler MJ, Kim GHJ, Tseng CH, Elashoff RM, Sclerodema Lung Study II Investigators (2016) Mycophenolate mofetil versus oral cyclophosphamide in scleroderma-related interstitial lung disease (SLS II): a randomised controlled, double-blind, parallel group trial. Lancet Respir Med 4(9):708–719
Izumi S, Iikura M, Hirano S (2012) Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med 367(9):869–871
Ghang B, Lee J, Chan Kwon O, Ahn SM, Oh JS, Hong S, Kim YG, Yoo B, Jeong WS, Kim J, Lee CK (2019) Clinical significance of autoantibody positivity in idiopathic pulmonary fibrosis. Respir Med 155:43–48
Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, Brozek JL, Collard HR, Cunningham W, Homma S, Johkoh T, Martinez FJ, Myers J, Protzko SL, Richeldi L, Rind D, Selman M, Theodore A, Wells AU, Hoogsteden H, Schünemann HJ, American Thoracic Society, European Respiratory society, Japanese Respiratory Society, Latin American Thoracic Association (2015) An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline. Am J Respir Crit Care Med 192(2):e3–e19
Fischer A, Antoniou KM, Brown KK, Cadranel J, Corte TJ, du Bois RM, Lee JS, Leslie KO, Lynch DA, Matteson EL, Mosca M, Noth I, Richeldi L, Strek ME, Swigris JJ, Wells AU, West SG, Collard HR, Cottin V (2015) An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J 46(4):976–987
Lightfoot RW Jr, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ et al (1990) The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum 33(8):1088–1093
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd et al (2010) 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62(9):2569–2581
Shiboski SC, Shiboski CH, Criswell L, Baer A, Challacombe S, Lanfranchi H et al (2012) American College of Rheumatology classification criteria for Sjogren’s syndrome: a data-driven, expert consensus approach in the Sjogren’s International Collaborative Clinical Alliance cohort. Arthritis Care Res 64(4):475–487
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CGM, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DGI, Specks U, Stone JH, Takahashi K, Watts RA (2013) 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65(1):1–11
Mosca M, Neri R, Bombardieri S (1999) Undifferentiated connective tissue diseases (UCTD): a review of the literature and a proposal for preliminary classification criteria. Clin Exp Rheumatol 17(5):615–620
Wilfong EM, Lentz RJ, Guttentag A, Tolle JJ, Johnson JE, Kropski JA, Kendall PL, Blackwell TS, Crofford LJ (2018) Interstitial pneumonia with autoimmune features: an emerging challenge at the intersection of rheumatology and pulmonology. Arthritis Rheum 70(12):1901–1913
Vij R, Strek ME (2013) Diagnosis and treatment of connective tissue disease-associated interstitial lung disease. Chest. 143(3):814–824
Hu Y, Wang LS, Wei YR, Du SS, Du YK, He X et al (2016) Clinical characteristics of connective tissue disease-associated interstitial lung disease in 1,044 Chinese patients. Chest. 149(1):201–208
Fischer A, Solomon JJ, du Bois RM, Deane KD, Olson AL, Fernandez-Perez ER, Huie TJ, Stevens AD, Gill MB, Rabinovitch AM, Lynch DA, Burns DA, Pineiro IS, Groshong SD, Duarte Achcar RD, Brown KK, Martin RJ, Swigris JJ (2012) Lung disease with anti-CCP antibodies but not rheumatoid arthritis or connective tissue disease. Respir Med 106(7):1040–1047
Kim EJ, Collard HR, King TE Jr (2009) Rheumatoid arthritis-associated interstitial lung disease: the relevance of histopathologic and radiographic pattern. Chest. 136(5):1397–1405
Doyle TJ, Dellaripa PF (2017) Lung manifestations in the rheumatic diseases. Chest. 152(6):1283–1295
Homma S, Suzuki A, Sato K (2013) Pulmonary involvement in ANCA-associated vasculitis from the view of the pulmonologist. Clin Exp Nephrol 17(5):667–671
Mohammad AJ, Mortensen KH, Babar J, Smith R, Jones RB, Nakagomi D, Sivasothy P, Jayne DRW (2017) Pulmonary Involvement in Antineutrophil Cytoplasmic Antibodies (ANCA)-associated vasculitis: the influence of ANCA subtype. J Rheumatol 44(10):1458–1467
Schirmer JH, Wright MN, Vonthein R, Herrmann K, Nolle B, Both M et al (2016) Clinical presentation and long-term outcome of 144 patients with microscopic polyangiitis in a monocentric German cohort. Rheumatology (Oxford) 55(1):71–79
Fernandez Casares M, Gonzalez A, Fielli M, Caputo F, Bottinelli Y, Zamboni M (2015) Microscopic polyangiitis associated with pulmonary fibrosis. Clin Rheumatol 34(7):1273–1277
Sahatciu-Meka V, Rexhepi S, Manxhuka-Kerliu S, Rexhepi M (2010) Extra-articular manifestations of seronegative and seropositive rheumatoid arthritis. Bosn J Basic Med Sci 10(1):26–31
Correia CS, Briones MR, Guo R, Ostrowski RA (2019) Elevated anti-cyclic citrullinated peptide antibody titer is associated with increased risk for interstitial lung disease. Clin Rheumatol 38(4):1201–1206
Wells AU, Denton CP (2014) Interstitial lung disease in connective tissue disease--mechanisms and management. Nat Rev Rheumatol 10(12):728–739
Kono M, Nakamura Y, Enomoto N, Hashimoto D, Fujisawa T, Inui N, Maekawa M, Suda T, Colby TV, Chida K (2014) Usual interstitial pneumonia preceding collagen vascular disease: a retrospective case control study of patients initially diagnosed with idiopathic pulmonary fibrosis. PLoS One 9(4):e94775
Kim HC, Lee JH, Chae EJ, Song JS, Song JW (2020) Long-term clinical course and outcome of interstitial pneumonia with autoimmune features. Respirology. 25(6):636–643
Lee SH, Kim SY, Kim DS, Kim YW, Chung MP, Uh ST, Park CS, Jeong SH, Park YB, Lee HL, Shin JW, Lee EJ, Lee JH, Jegal Y, Lee HK, Kim YH, Song JW, Park SW, Park MS (2016) Predicting survival of patients with idiopathic pulmonary fibrosis using GAP score: a nationwide cohort study. Respir Res 17(1):131
Acknowledgments
We would like to thank Hyojung Choi from the Department of Clinical Research Information at Asan Medical Center for her assistance in preparing this manuscript. We thank Dr. Joon Seo Lim from the Scientific Publications Team at Asan Medical Center for his editorial assistance.
Funding
This work was supported by the research fund of the Rheumatology Research Foundation (RRF-2018-04)
Author information
Authors and Affiliations
Contributions
The authors all meet the journal's criteria for authorship.
Corresponding author
Ethics declarations
Competing interests
The authors have declared no conflicts of interest.
Ethical approval
The study was approved by the Institutional Review Board of Asan Medical Center (IRB number: 2016-0222), and conforms to the ethical guidelines of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Under the Discussion section of this article, "IPA patients" was changed to "IPF patients".
Supplementary Information
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Ghang, B., Nam, S.H., Lee, J. et al. Risk of progression of idiopathic pulmonary fibrosis to connective tissue disease: a long-term observational study in 527 patients. Clin Rheumatol 40, 2447–2456 (2021). https://doi.org/10.1007/s10067-021-05659-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05659-x