Abstract
Thrombotic events are the most frequent causes of death in patients with antiphospholipid syndrome (APS). Previous studies have reported infection to be the most important trigger of thrombosis in APS, with molecular mimicry considered to be a major mechanism. Although timely management of infections has been recommended in patients with high suspicion of infection, anti-infective therapy would not take effect in a short time due to the dilemma in determining the origins of infection, especially in patients undergoing immunosuppressive therapy. Here, we describe a 26-year-old patient with systemic lupus erythematosus with triple antiphospholipid antibody positivity who had a stroke involving her dorsolateral medulla, despite timely anti-infective treatment within the context of skin infection caused by Stenotrophomonas maltophilia. To the best of our knowledge, it is the first report about the association between Stenotrophomonas maltophilia infection and thrombotic complications in APS. Thus, solely focusing on anti-infective therapy by the current recommendation for the management of APS may be insufficient within the context of infection; early initiation of effective anticoagulation should also be suggested until the anti-infective therapy becomes effective, especially in patients with high-risk antiphospholipid antibody profiles, in whom the potential benefit would outweigh the risk of bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiphospholipid syndrome (APS) is a systemic autoimmune disorder characterized by the occurrence of venous and arterial thrombosis as well as obstetric manifestations due to the presence of pathogenic autoantibodies known as antiphospholipid antibodies (aPLs), including lupus anticoagulant (LA), anti-cardiolipin antibodies (anti-CL), and anti-β2 glycoprotein I antibodies (anti-β2GPI) [1]. APS can occur as an isolated diagnosis or can coexist with systemic lupus erythematosus (SLE) or other autoimmune diseases. Thrombotic events are the most frequent causes of death in patients with APS [2]. Accumulating evidence has proposed a variety of independent risk factors for thrombotic events, such as concurrent other systemic autoimmune diseases and the presence of a high-risk aPL profile (defined as persistently high aPL titers, LA, or multiple aPL positivity) [3]. Thromboprophylaxis with low-molecular-weight heparin has been shown to be effective in reducing thrombotic events and therefore recommended in patients with persistently positive aPLs during high-risk periods, including pregnancy pre- and peri-partum, recent surgery, and concurrent SLE with low albumin levels [3,4,5].
Previous studies have revealed that infections may be the most important triggers of elevated aPL levels and thrombosis and even catastrophic APS (CAPS), which is a lethal condition characterized by thrombotic events in various organs over multiple days [6]. Molecular mimicry is considered to be a major mechanism in the association between APS and infection [7]. Although prompt treatment of infection by the early use of anti-infective medications has been recommended in patients with APS [3], it may be not effective in a short time, mainly due to the difficulties in determining the origins of infection, especially in patients undergoing immunosuppressive therapy. Therefore, to avoid the enhanced risk of thrombosis caused by infection, a question arises as to whether early initiation of effective anticoagulation should be suggested until the anti-infective therapy takes effect, especially in patients with high-risk aPL profiles. Here, we describe a high-risk patient with concurrent SLE who had a stroke involving her dorsolateral medulla, despite timely anti-infective treatment under infection caused by Stenotrophomonas maltophilia (S. maltophilia). To the best of our knowledge, this is the first report about the association between S. maltophilia infection and thrombotic complications in APS.
Case presentation
A 26-year-old Chinese woman was referred to our hospital due to a 10-day history of numbness, pain, and ecchymoses in the lower extremities, polyarthralgia, and fever (T-max 39.4 °C). She admitted hypersensitivity to sunlight but denied any other symptoms, including rash, oral ulcers, headache, or dizziness. She had two healthy children without a history of pathological pregnancy. She denied relevant past medical or family histories, and she did not smoke.
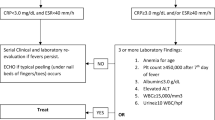
On admission, the patient had normal vital signs, and her physical examination did not reveal any abnormal findings except for ecchymosis and small ulcers on both lower extremities. The results of her laboratory tests showed elevated C-reactive protein (46.63 mg/L; normal range < 5 mg/L), erythrocyte sedimentation rate (115 mm/h; normal range < 20 mm/h), and D-Dimer (3622.99 ng/mL; normal range < 100 ng/mL) as well as a prolonged activated partial thromboplastin time (56.3 s, 29.7 s in the control). Her complete blood cell count, basic metabolic panel, and levels of complement components C3 and C4 were normal. A comprehensive infectious workup, including repeated blood cultures, was negative. Rheumatological evaluation yielded a high titer of anti-nuclear antibodies, positivity for anti-dsDNA and anti-Smith antibodies, and high levels of anti-CL IgG (> 120 GPLU/mL; normal range < 12 GPLU/mL) and anti-ß2GPI-IgG (97.7 AU/mL; normal range < 24 AU/mL). In addition, LA and direct Coomb’s test were positive. Echocardiography revealed thickened anterior mitral valve leaflets with vegetations and moderate mitral regurgitation (Fig. 1), which was consistent with Libman-Sacks endocarditis. Electromyography showed different degrees of myogenic lesions and damage to peripheral nerve motor and sensory conduction in the extremities. Other investigations involving normal Doppler ultrasound and computed tomography angiography (CTA) of the lower extremities as well as unremarkable magnetic resonance imaging (MRI) of the head and CT of the lungs were notable.
A definitive diagnosis of SLE was made, with an SLE disease activity index of 9 (mild disease activity). Therefore, on hospital day 3, methylprednisolone (40 mg/day) and hydroxychloroquine (200 mg, twice/day) were initiated. The patient’s complaints were dramatically reduced, without fever for 2 weeks. However, more exudates gradually appeared on the surface of the ulcers in her lower extremities, and the patient began to have intermittent fever (T-max 38.3 °C) starting from hospital day 19. The result of her repeated echocardiography was almost the same as before. On hospital day 20, levofloxacin was initiated immediately, and the skin exudate culture later tested to be positive for S. maltophilia (with sensitivity to levofloxacin according to the result of a drug sensitivity test). The peak temperature decreased, but her fever still persisted in the following days.
On hospital day 25, the patient suddenly complained of dizziness, perioral numbness, dysphagia, and dysarthria. An urgent head MRI revealed a region of hyperintensity in the left dorsolateral medulla (Fig. 2), which was confirmed by neurosurgeons as acute dorsolateral medullary infarction. Enoxaparin was started immediately and later successfully bridged to warfarin for long-term anticoagulation (target INR, 2.5–3.5), with aspirin and statin commenced; piperacillin and tazobactam were added to better control the skin infection. She gradually showed substantial improvement in symptoms during the next 2 weeks and was subsequently discharged. Four months after initial presentation, the diagnosis of APS was confirmed due to the episode of stroke and the persistent presence of LA with high titers of anti-CL IgG and anti-ß2GPI IgG. No thrombotic events reoccurred during the 13-month follow-up period under the therapy of low-dose steroids and hydroxychloroquine, along with a combined regimen of anticoagulation with warfarin (target INR, 2.0–3.0) and aspirin as an antiplatelet agent.
Discussion
Diagnosis of APS
We depict an SLE patient with triple aPL positivity who experienced a sudden dorsolateral medullary infarction despite timely anti-infective treatment within the context of skin infection caused by S. maltophilia. A definitive diagnosis of APS requires at least one clinical manifestation (thrombotic or adverse pregnancy events) and one laboratory criterion (persistent presence of aPLs), measured at least 12 weeks apart [8]. Using these updated Sapporo classification criteria often results in a lack of sensitivity and might fail to encompass APS patients with aPL-related clinical manifestations other than thrombosis or pathological pregnancy. Accordingly, although this case did not fulfill the classification criteria of APS before the occurrence of stroke, the patient had triple aPL positivity and several “extra-criteria” features [9], such as heart valve disease (Libman-Sacks endocarditis) and leg ulcers. In addition, the stroke episode and persistent presence of aPLs remeasured 4 months after the initial presentation supported the diagnosis of APS in this patient.
Risk stratification of thrombotic events
Thrombotic events are the most common causes of death in patients with APS, accounting for approximately 40% of mortality [2]. Identifying the presence of factors associated with high risk for thrombotic events is critical in APS patient management. As the most likely factor related to thrombosis, aPLs mainly interact with endothelial cells and monocytes and stimulate platelet activation, resulting in a pro-thrombotic phenotype [10]. Accordingly, the high-risk aPL profile, such as the presence of LA, triple aPL positivity, and the presence of persistently high aPL titers are major risk factors for thrombosis. According to a retrospective study, the cumulative incidence rates of recurrent thrombotic events in patients with APS who had triple aPL positivity were 12.2%, 26.1%, and 44.2% after 1, 5, and 10 years of follow-up, respectively [11]. Additional risk factors for thrombosis include coexistence of other systemic autoimmune diseases (especially SLE), a history of thrombotic events, and the presence of traditional cardiovascular risk factors [3]. Therefore, to prevent thrombosis, a risk-stratified approach is needed for individuals with APS. The aPL score has been reported to be a predictive marker for thrombosis in APS, and an aPL score of > 30 is an independent risk factor for thrombosis [12]. The global APS score (GAPSS) is another quantitative scoring system for risk prediction of APS-related thrombosis, taking into account the aPL profile and conventional cardiovascular risk factors. GAPSS values ≥ 10 have been reported to have the best diagnostic accuracy [13]. The patient discussed herein had a high-risk aPL profile and coexistence of SLE, with aPL scores ≥ 45 and GAPSS values ≥ 13, regardless of anti-phosphatidylserine/prothrombin antibodies (not detected), resulting in a considerably high risk of thrombosis.
Stroke is one of the most frequent thrombotic events in APS, being present in 5.3% of a total cohort of 1000 patients during the 10-year follow-up [2]. Accordingly, the patient with concurrent SLE and APS in this study experienced medullary infarction, which has also been reported previously as a complication in patients with APS or aPLs [14, 15]. Intriguingly, Risse et al. recently reported a case of reversible APS due to minocycline in a patient who experienced recurrent strokes including an acute infarct in the left medulla oblongata [16].
Infection as a trigger of thrombosis in APS
Studies have shown that the presence of aPLs may be associated with different infections [6], in which β2GPI has been established as the culprit in the interactions between infections and APS. In vitro and in vivo studies suggest that molecular mimicry between β2GPI-related peptides and structures of microbial pathogens may be a major mechanism in the correlation between infections and APS [17,18,19]. Initial studies showed that aPLs induced by infections did not possess anti-β2GPI activity and had no relationship with thrombotic complications [20]. However, increasing evidence has revealed that increased levels of infection-related aPLs were associated with APS features including thrombosis [21,22,23,24].
Various infections can be associated with thrombotic events in patients with APS, skin infections being reported as the main associated infection [25]. A systematic review of case reports revealed that the most common preceding infection was viral (55.6%) in the development of APS or APS-related manifestations [26]. In addition, a strikingly high prevalence of aPLs was observed in patients with coronavirus disease 2019 (COVID-19), accounting for up to 96% (24/25) [27]. A Dutch study confirmed a high cumulative incidence of thrombotic complications (49%) in 184 critically ill patients with COVID-19 despite all patients receiving pharmacological thromboprophylaxis [28]. Recently, aPLs have been considered to be implicated in the higher thrombotic burden in patients with COVID-19 [29,30,31]. On the other hand, aPLs have also been reported to be associated with various bacterial infections (36.9%) [26], with Mycoplasma pneumonia the most common bacteria associated with thrombosis. As shown in Table 1, various infections have been reported to be associated with thrombotic events in aPL-positive situations and APS as well as CAPS [29, 31,32,33,34,35,36,37,38,39,40]. Intriguingly, the patient in this study experienced a stroke in the context of skin infection caused by S. maltophilia, which is, to our knowledge, the first report about the association between S. maltophilia infection and thrombosis in APS. Notably, Carrillo-Córdova et al. previously described a patient with SLE complicated by rheumatoid arthritis and positive aPLs who developed community-acquired S. maltophilia endocarditis, suggesting that autoimmunity could be a possible predisposing factor for S. maltophilia endocarditis [41].
According to the “two-hit hypothesis,” the presence of aPLs provides the “first hit” by activating interactions with endothelial cells, neutrophils, platelets, and monocytes, and “second hit” factors, such as infections and trauma, further contribute to thrombosis [9]. Infectious agents may lead to a disproportionate immune response involving both the innate and adaptive immune systems by generating pathogenic anti-β2GPI antibodies. In this patient, dorsolateral medullary infarction occurred within the context of her skin infection. It is reasonable to speculate that the skin infection in this patient with APS may have played the role of the postulated “second hit,” leading to the thrombotic event. Therefore, it is extremely important to eliminate the triggering factor of infection, and early recognition and timely management of infections have been recommended in patients with high suspicion of infection [3]. Importantly, S. maltophilia, a ubiquitous Gram-negative and aerobic bacillus, has emerged as an increasingly prevalent opportunistic pathogen with widespread antimicrobial resistance in debilitated patients. Trimethoprim-sulfamethoxazole and levofloxacin are generally considered to be the first-line antibiotics in the treatment of S. maltophilia infections. Nevertheless, studies have revealed a higher resistance and decreased susceptibility to these first-line agents [42, 43]. This may partially explain the unsatisfactory outcome of the initial anti-infective therapy with levofloxacin in our patient. Moreover, given the additional susceptibility of thrombosis within the context of infection, one question is whether combination therapy of effective anticoagulation and timely management of infection is advisable to secure such a high-risk patient.
Antithrombotic therapy in APS
Antithrombotic therapy in APS depends on the indication and risk of bleeding. In fact, the number of deaths associated with fatal bleeding secondary to anticoagulant treatment is considerably lower than those related to recurrent thrombosis in patients with APS [44]. According to the 2019 EULAR recommendations for the management of APS [3], patients with definite APS and first venous thrombosis should be treated with vitamin K antagonists, with a target INR 2.0–3.0. Notably, a systematic review revealed that recurrent thrombotic complications were uncommon in patients administered sufficient oral anticoagulation to a target INR of 3.0–4.0 [44]. In addition, the intensity of anticoagulation may be overestimated in patients with LA positivity because INR is not reliable in reflecting the true level of anticoagulation, leading to a subtherapeutic warfarin dose [45]. Therefore, it remains to determine the best evidence-based strategy to prevent thrombotic events in patients with APS.
An effective thromboprophylaxis with low-molecular-weight heparin has been shown to be protective in thrombotic events and therefore has been recommended in patients with persistently positive aPLs during some high-risk situations such as pregnancy pre- and peri-partum, recent surgery, and SLE patients with nephritic syndrome and low albumin levels [3,4,5]. Notably, a recent study revealed that anticoagulation therapy at admission was associated with a lower risk of thrombotic complications [28]. Therefore, in decision-making about the timing of prophylactic antithrombotic therapy, we should promptly recognize transient high-risk situations, where an early initiation of effective anticoagulation is required for a brief period.
As discussed above, infection is the most important precipitating factor for thrombotic events in APS, and it is critical to administer anti-infective therapy in a timely manner. However, anti-infective therapy does not take effect immediately due to the difficulties in determining the origins of infection, especially in patients undergoing immunosuppressive therapy. In this circumstance, in addition to prompt treatment of infections, early initiation of effective anticoagulation is advisable in high-risk patients in whom the potential benefit would outweigh the risk of bleeding. Although not supported by prospective controlled studies, combination therapy of effective anticoagulation and timely anti-infective treatment may be required to secure patients with high-risk aPL profiles during infection.
Conclusions
Infection is an important trigger of thrombotic events in APS. In addition to early diagnosis and management of infections, early initiation of effective anticoagulation should be suggested to secure patients with high-risk aPL profiles, in whom the potential benefit may outweigh the risk of bleeding. High-quality prospective controlled studies on strategies of antithrombotic therapy under infection in patients with high-risk aPL profiles are needed in the future.
Data availability
The files are available from the corresponding author on request.
References
Giannakopoulos B, Krilis SA (2013) The pathogenesis of the antiphospholipid syndrome. N Engl J Med 368:1033–1044
Cervera R, Serrano R, Pons-Estel GJ, Ceberio-Hualde L, Shoenfeld Y, de Ramón E, Buonaiuto V, Jacobsen S, Zeher MM, Tarr T, Tincani A, Taglietti M, Theodossiades G, Nomikou E, Galeazzi M, Bellisai F, Meroni PL, Derksen RH, de Groot PG, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quéré I, Hachulla E, Vasconcelos C, Fernández-Nebro A, Haro M, Amoura Z, Miyara M, Tektonidou M, Espinosa G, Bertolaccini ML, Khamashta MA, Euro-Phospholipid Project Group (European Forum on Antiphospholipid Antibodies) (2015) Morbidity and mortality in the antiphospholipid syndrome during a 10-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis 74:1011–1018
Tektonidou MG, Andreoli L, Limper M, Amoura Z, Cervera R, Costedoat-Chalumeau N, Cuadrado MJ, Dörner T, Ferrer-Oliveras R, Hambly K, Khamashta MA, King J, Marchiori F, Meroni PL, Mosca M, Pengo V, Raio L, Ruiz-Irastorza G, Shoenfeld Y, Stojanovich L, Svenungsson E, Wahl D, Tincani A, Ward MM (2019) EULAR recommendations for the management of antiphospholipid syndrome in adults. Ann Rheum Dis 78:1296–1304
Ruffatti A, Del Ross T, Ciprian M et al (2011) Risk factors for a first thrombotic event in antiphospholipid antibody carriers: a prospective multicentre follow-up study. Ann Rheum Dis 70:1083–1086
Arnaud L, Conti F, Massaro L, Denas G, Chasset F, Pengo V (2017) Primary thromboprophylaxis with low-dose aspirin and antiphospholipid antibodies: pro’s and con’s. Autoimmun Rev 16:1103–1108
Mendoza-Pinto C, Garcia-Carrasco M, Cervera R (2018) Role of infectious diseases in the antiphospholipid syndrome (including its catastrophic variant). Curr Rheumatol Rep 20:62
Blank M, Asherson RA, Cervera R, Shoenfeld Y (2004) Antiphospholipid syndrome infectious origin. J Clin Immunol 24:12–23
Miyakis S, Lockshin MD, Atsumi T et al (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
Sciascia S, Amigo M, Roccatello D, Khamashta M (2017) Diagnosing antiphospholipid syndrome: ‘extra-criteria’ manifestations and technical advances. Nat Rev Rheumatol 13:548–560
Chighizola CB, Andreoli L, Gerosa M, Tincani A, Ruffatti A, Meroni PL (2018) The treatment of anti-phospholipid syndrome: a comprehensive clinical approach. J Autoimmun 90:1–27
Pengo V, Ruffatti A, Legnani C et al (2010) Clinical course of high-risk patients diagnosed with antiphospholipid syndrome. J Thromb Haemost 8:237–242
Otomo K, Atsumi T, Amengual O, Fujieda Y, Kato M, Oku K, Horita T, Yasuda S, Koike T (2012) Efficacy of the antiphospholipid score for the diagnosis of antiphospholipid syndrome and its predictive value for thrombotic events. Arthritis Rheum 64:504–512
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta MA, Bertolaccini ML (2013) GAPSS: The Global Anti-Phospholipid Syndrome Score. Rheumatology 52:1397–1403
Delevaux I, Andre M, Marroun I et al (2005) Intractable hiccup as the initial presenting feature of systemic lupus erythematosus. Lupus 14:406–408
Horiki T, Moriuchi J, Kouzuma R et al (1995) A case of systemic lupus erythematosus with various central and peripheral neurological disorders presenting with motor paralytic bladder as a major manifestation. Ryumachi 35:821–826
Risse J, Vieira M, Beuret F et al (2017) Reversible drug-induced antiphospholipid syndrome. Lupus 27:333–335
Blank M, Shoenfeld Y, Cabilly S, Heldman Y, Fridkin M, Katchalski-Katzir E (1999) Prevention of experimental antiphospholipid syndrome and endothelial cell activation by synthetic peptides. Proc Natl Acad Sci U S A 96:5164–5168
Gharavi AE, Pierangeli SS, Espinola RG, Liu X, Colden-Stanfield M, Harris EN (2002) Antiphospholipid antibodies induced in mice by immunization with a cytomegalovirus-derived peptide cause thrombosis and activation of endothelial cells in vivo. Arthritis Rheum 46:545–552
Pierangeli SS, Blank M, Liu X, Espinola R, Fridkin M, Vega Ostertag M, Roye-Green K, Harris EN, Shoenfeld Y (2004) A peptide that shares similarity with bacterial antigens reverses thrombogenic properties of antiphospholipid antibodies in vivo. J Autoimmun 22:217–225
Elbeialy A, Strassburger-Lorna K, Atsumi T, Bertolaccini ML, Amengual O, Hanafi M, Khamashta MA, Hughes GR (2000) Antiphospholipid antibodies in leprotic patients: a correlation with disease manifestations. Clin Exp Rheumatol 18:492–494
Hojnik M, Gilburd B, Ziporen L, Blank M, Tomer Y, Scheinberg MA, Tincani A, Rozman B, Shoenfeld Y (1994) Anticardiolipin antibodies in infections are heterogenous in their dependency on beta 2-glycoprotein I: analysis of anticardiolipin antibodies in leprosy. Lupus 3:515–521
Loizou S, Cazabon JK, Walport MJ, Tait D, So AK (1997) Similarities of specificity and cofactor dependence in serum antiphospholipid antibodies from patients with human parvovirus B19 infection and from those with systemic lupus erythematosus. Arthritis Rheum 40:103–108
Fiallo P, Nunzi E, Cardo PP (1998) beta2-Glycoprotein I-dependent anticardiolipin antibodies as risk factor for reactions in borderline leprosy patients. Int J Lepr Other Mycobact Dis 66:387–388
Blank M, Shani A, Goldberg I, Kopolovic J, Amigo MC, Magrini L, Shoenfeld Y (2004) Libman–Sacks endocarditis associated with antiphospholipid syndrome and infection. Thromb Res 114:589–592
Cervera R (2004) Antiphospholipid syndrome associated with infections: clinical and microbiological characteristics of 100 patients. Ann Rheum Dis 63:1312–1317
Abdel-Wahab N, Lopez-Olivo MA, Pinto-Patarroyo GP, Suarez-Almazor ME (2016) Systematic review of case reports of antiphospholipid syndrome following infection. Lupus 25:1520–1531
Pineton DCM, Frere C, Miyara M et al (2020) High frequency of antiphospholipid antibodies in critically-ill COVID-19 patients: a link with hypercoagulability? J Intern Med. https://doi.org/10.1111/joim.13126
Klok FA, Kruip M, van der Meer N et al (2020) Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res 191:148–150
Goldberg MF, Goldberg MF, Cerejo R, Tayal AH (2020) Cerebrovascular disease in COVID-19. AJNR Am J Neuroradiol 41:1170–1172. https://doi.org/10.3174/ajnr.A6588
Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, Chen H, Ding X, Zhao H, Zhang H, Wang C, Zhao J, Sun X, Tian R, Wu W, Wu D, Ma J, Chen Y, Zhang D, Xie J, Yan X, Zhou X, Liu Z, Wang J, du B, Qin Y, Gao P, Qin X, Xu Y, Zhang W, Li T, Zhang F, Zhao Y, Li Y, Zhang S (2020) Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 382:e38
Sung J, Anjum S (2020) Coronavirus disease 2019 (COVID-19) infection associated with antiphospholipid antibodies and four-extremity deep vein thrombosis in a previously healthy female. Cureus 12:e8408
Flateau C, Asfalou I, Deman AL, Ficko C, Andriamanantena D, Fontan E, Viant E, Bonnevie L, Rapp C (2013) Aortic thrombus and multiple embolisms during a Mycoplasma pneumoniae infection. Infection 41:867–873
Vázquez Fuentes N, Tejero García S, Carnicero González F, Martínez Bagur I, de Torres RM, Querol Gutiérrez JJ, Laza Laza EM, Querol Gutiérrez JC (2008) Gangrena como manifestación inicial de un síndrome antifosfolipídico catastrófico. Reumatol Clín 4:119–122
Dong R, Weng L, Guo T et al (2017) The 455th case: swollen leg, jaundice and mental disturbance. Zhonghua Nei Ke Za Zhi 56:316–320
Tanizawa K, Nakatsuka D, Tanaka E et al (2009) Pulmonary thrombosis with transient antiphospsholipid syndrome after mononucleosis-like illness. Int Med (Tokyo, 1992) 48:1231–1234
Catoggio C, Alvarez-Uría A, Fernandez PL, Cervera R, Espinosa (2012) Catastrophic antiphospholipid syndrome triggered by fulminant disseminated herpes simplex infection in a patient with systemic lupus erythematosus. Lupus 21:1359–1361
Durkin ML, Marchese D, Robinson MD, Ramgopal M (2013) Catastrophic antiphospholipid syndrome (CAPS) induced by influenza A virus subtype H1N1. BMJ Case Rep 2013:bcr2013200474
Yegneswaran Prakash P, Pandit V, Rao SP (2012) Fulminant antiphospholipid antibody syndrome complicated by Aspergillus tracheobronchitis. Med Mycol Case Rep 1:99–102
Niitsuma T, Nukaga M, Izawa A, Tsuyuguchi M, Tsuboi N, Hayashi T (2003) Antiphospholipid syndrome during allergic bronchopulmonary aspergillosis. Allergy 58:454–455
Pers YM, Puygrenier M, Borlot F, Simorre B, Barazer I, Oziol E, Reny JL (2009) Acute Q fever, antiphopholipid antibodies and renal artery thrombosis: case report and literature review. Rev Med Interne 30:250–254
Carrillo-Córdova JR, Amezcua-Guerra LM (2012) Autoimmunity as a possible predisposing factor for Stenotrophomonas maltophilia endocarditis. Arch Cardiol Méx 82(3):204–207
Wei C, Ni W, Cai X, Cui J (2015) A Monte Carlo pharmacokinetic/pharmacodynamic simulation to evaluate the efficacy of minocycline, tigecycline, moxifloxacin, and levofloxacin in the treatment of hospital-acquired pneumonia caused by Stenotrophomonas maltophilia. Infect Dis (Lond) 47:846–851
Matson HH, Jones BM, Wagner JL, Motes MA, Bland CM (2019) Growing resistance in Stenotrophomonas maltophilia? Am J Health Syst Pharm 76:2004–2005
Guillermo Ruiz-Irastorza, Beverley J. Hunt, Munther A. Khamashta (2007) A systematic review of secondary thromboprophylaxis in patients with antiphospholipid antibodies. Arthritis & Rheumatism 57 (8):1487-1495
Moll S, Ortel TL (1997) Monitoring warfarin therapy in patients with lupus anticoagulants. Ann Intern Med 127:177–185
Acknowledgments
All authors wish to thank the patient in this study and Dr. Fa-Jin Dong for supplying the images of echocardiography and magnetic resonance in this paper.
Funding
This study was financially supported by the Sanming Project of Medicine in Shenzhen (grant number SYJY201901); National Natural Science Foundation of China (grant number 81971464); and National Key Research and Development Program of China (grant number 2019YFC0840600).
Author information
Authors and Affiliations
Contributions
All authors contributed to the final manuscript. Yu-Lan Chen and Hai-Tao Yang analyzed documents and drafted the manuscript. Corresponding authors Dong-Zhou Liu and Jiu-Liang Zhao read and revised the manuscript. Li-Xiong Liu and Cui-Hong Chen participated in drafting the manuscript. Qin Huang and Xiao-Ping Hong performed the clinical assessment and collected the clinical data. All authors have read and approved the final submitted version.
Corresponding authors
Ethics declarations
Disclosures
None.
Ethics approval and consent to participate
This patient gave her written informed consent before clinical data collection. This study was conducted in compliance with the Helsinki Declaration and was approved by the Medical Ethics Committee of Shenzhen People’s Hospital (identifier LL-KT-2018358).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, YL., Yang, HT., Liu, LX. et al. Dorsolateral medullary infarction during skin infection by Stenotrophomonas maltophilia in a patient with triple antiphospholipid antibody positivity: a case-based review. Clin Rheumatol 40, 2965–2971 (2021). https://doi.org/10.1007/s10067-020-05489-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05489-3