Abstract
Cardiac involvement is very rare in patients with Henoch-Schönlein purpura (HSP). In this case study, we present an 8-year-old girl presenting with HSP-induced myocarditis and thrombus in the right atrium and HSP nephritis. To date, 15 cases of HSP-related cardiac involvement have been reported in the PubMed/MEDLINE, Scopus, and Google Scholar databases. These cases, together with our case, are included in this review. We excluded those patients with other rheumatologic diseases (acute rheumatic fever, acute post-streptococcal glomerulonephritis, Kawasaki disease) accompanied by HSP. Three were children and 13 were adults and all were male except our case. This review revealed tachyarrhythmia, chest pain, dyspnea, murmur, and heart failure as the major signs. Cardiac tests, electrocardiogram (ECG), and imaging methods (echocardiography in all patients, cardiac magnetic resonance imaging (MRI) in three, cardiac biopsy in one, and post-mortem necropsy in three) showed that the cardiac involvements were pericardial effusion, intra-atrial thrombus, myocarditis, coronary artery changes, myocardial ischemia, infarction and necrosis, subendocardial hemorrhage, and left ventricular dilatation. Kidney involvement was not observed in three patients. As the treatment, high-dose prednisolone and cyclophosphamide, oral corticosteroid, azathioprine, nadroparin calcium, ACE inhibitors, calcium antagonists, beta-blockers, and diuretics were used. Eleven patients (all three children and eight of the adults) had a complete cardiac recovery. Cardiac involvement in adults was more likely to be fatal. Death (three patients), ischemia, and infarct have been reported only in adults. We suggested that early and aggressive treatment can be life-saving. MRI examination is effective at identifying cardiac involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Henoch-Schönlein purpura (IgA vasculitis) is the most common childhood vasculitis. It is characterized by the deposition of immune complexes containing the antibody immunoglobulin A (IgA) on small vessels (arterioles, capillaries, and venules). In addition to the typical lesions in the lower extremities, children with Henoch-Schönlein purpura (HSP) often have gastrointestinal system, joint, and kidney involvement, and rarely central nervous system, pulmonary, ocular, and scrotal involvement. Indeed, kidney involvement in patients with HSP determines the prognosis [1, 2]. Moreover, cardiac involvement is rare in Henoch-Schönlein purpura, and few case reports have been published in the literature [3,4,5,6,7,8,9,10,11,12,13,14,15,16]. Here, we present the clinical follow-up, treatment, and prognosis of a patient with cardiac involvement due to HSP, which is a rare condition in HSP.
Case report
An 8-year-old girl presented to our clinic with a complaint of decreased urine output, rashes on the hips, legs, and ankles, and swelling of the ankles. It was learned from her anamnesis that she used antibiotics for 10 days due to tonsillitis 15 days previously, while her antibiotic treatment continued, she had swelling in her left hand and a rash on her feet 2 days later. Medical history of the patient and the family revealed that there was no feature rheumatological disease, Behçet’s disease, kidney disease, or heart disease. There was no kinship between parents.
On physical examination, her body temperature was 36.5 °C, and anthropometric measurements were within normal limits according to age and gender. Blood pressure was evaluated as 130/90 mmHg (> p95/> p95) stage I hypertension [17]. There were palpable purpuric rashes that started from the gluteal region and intensified in the ankle, which did not fade with compression (Fig. 1). Pretibial edema was 2+. Other system examination findings of the patient were normal.
In laboratory examinations, anemia, abnormalities in renal function tests, decrease in complement (C3 and C4), ASO elevation, hyperlipemia, hypoalbuminemia, and elevation in acute phase reactants were detected (Table 1). In the throat culture, there was normal throat flora. There was no positivity in multiplex real-time PCR for respiratory tract infection (mycoplasma, influenza A, influenza B, respiratory syncytial virus-A, influenza A virus subtype H1N1, coronavirus, rhinovirus, adenovirus, bocavirus, human parainfluenza virus, metapneumovirus, enterovirus, and parechovirus). Other biochemical parameters were normal and serological examinations were negative. Urinary examination revealed nephrotic proteinuria, and microscopic urine examination revealed dysmorphic erythrocytes and erythrocyte casts (Table 1). Skin biopsy of the patient resulted in IgA markedly stained leukocytoclastic vasculitis. The patient underwent kidney biopsy due to the findings of impaired kidney function, the coexistence of nephrotic and nephritic syndrome (mixed), typical HSP rashes, and hypocomplementemia. Kidney biopsy resulted in HSP nephritis. Diffuse mesangial cell proliferation and limited endocapillary proliferation without crescent was observed by periodic acid-Schiff staining in light microscopic evaluation, and immunofluorescence staining showed 2+ IgA and 1+ C3 deposits in mesangium in kidney biopsy. As a consequence, the patient was diagnosed with HSP and HSP nephritis, according to the EULAR/PreS criteria [18].
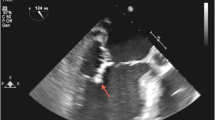
In the clinical follow-up of the patient, an echocardiographic examination based on the development of non-febrile tachycardia revealed a minimal pericardial effusion and a hyperechogenicity appearance in the right atrium with a size of 1.2 × 1.1 cm. At the same time, troponin T level was normal, but brain natriuretic peptide (BNP) level was high (6283 ng/L) (Table 1).
The contrast-enhanced functional cardiac magnetic resonance (MR) examination revealed a bilateral mid-grade (reaching 3 cm at its thickest spot) pleural effusion, a filling defect that was approximately 1 cm in diameter at the base of the right atrium, nearby the opening of the inferior vena cava, and compatible with the thrombus. Focal hypokinesia areas were determined in places where the left ventricular ejection fraction was reduced to 52% at the margin and more prominent in the interventricular septum in the left ventricle. In the late-phase (tenth minute) contrast images obtained after intravenous contrast medium, pathological late contrast involvement areas were noticeable at the level of the interventricular septum, and inferior and lateral walls of the left ventricle (Figs. 2 and 3). Transmural or mid-myocardial pathological late contrast involvement was observed in these areas and was evaluated in favor of myocardial inflammation (myocarditis) [19].
Initial cardiac magnetic resonance images of the patient. a Axial balanced-steady-state free precession (b-SSFP) image shows bilateral pleural effusion (arrowheads), pericardial effusion (*), and a hypointense filling defect into the right atrium. b Sagittal oblique b-SSFP image shows a filling defect into the right atrium base compatible with thrombus (arrow). Note the pleural effusion (arrowhead). c Short-axis and d four-chamber late gadolinium-enhanced images, which were obtained with phase-sensitive inversion recovery (PSIR) after 0.1 mg/kg gadoteric acid injection, shows pathological mid-myocardial, myo-pericardial, and transmural contrast-enhancement areas (arrows), compatible with myocarditis
Control cardiac magnetic resonance images of the patient. a Axial balanced-steady-state free precession (b-SSFP) image shows no pleural or pericardial effusion. b Coronal oblique b-SSFP image shows no filling defect into the right atrium. c Four-chamber late gadolinium-enhanced images, which were obtained with phase-sensitive inversion recovery (PSIR) after 0.1 mg/kg gadoteric acid injection, show no pathological contrast enhancement
The thrombosis panel was evaluated (MTHFR, factor V Leiden and prothrombin G20210A mutation analysis, protein C and protein S activity, and antithrombin III activity). There were no mutations and abnormalities in those activities. The level of D-Dimer was high, aPTT and INR were normal (Table 1).
The patient was diagnosed with HSP nephritis, acute renal failure, and HSP-related cardiac involvement, and two sessions of hemodialysis in the acute period were performed. Pulse methylprednisolone (30 mg/kg/day) was administered for five consecutive days plus a monthly pulse of cyclophosphamide (750 mg/m2/month, for 6 months). Then, oral prednisolone was continued at 30 mg/day (60 mg/m2/day) and tapered off monthly. Meanwhile, nadroparin calcium (100 mg/kg) was given for 2 weeks as an anticoagulant. Creatinine and eGFR (139 mL/min/1.73 m2) returned to normal on the 13th day of treatment. The level of BNP returned to normal (12 ng/L) by treatment within 30 days. Ramipril (4 mg/m2) was started after the acute period.
In the echocardiographic evaluation on the 15th day of treatment, the thrombus in the right atrium disappeared. On the 60th day, pericardial effusion disappeared, and heart functions were completely normal. In the sixth month of the treatment, myocardial inflammation, pericardial effusion, and thrombus appearance in the right atrium were observed to be completely improved by functional cardiac MR control. In the seventh month, anemia, hypoalbuminemia, kidney function, and acute phase reactants were normal. The patient’s proteinuria decreased gradually, and at the final control in the eighth month, the value was 140 mg/day (7 mg/m2/h). The patient is still being followed up with azathioprine, low-dose oral prednisolone (5 mg/day), and ramipril.
Search strategy
The literature was reviewed using the PubMed, Scopus, and Google Scholar databases and the following search term: “cardiac involvement” and “Henoch-Schönlein purpura” or “IgA vasculitis.” The articles or case reports that were published up to May 2020 were included in this report. The articles that solely included cardiac involvement associated with HSP were reviewed. Recent publications were favored. Other diseases associated with HSP (acute rheumatic fever, post-streptococcal glomerulonephritis, sepsis, disseminated intravascular coagulation) and any articles with suspected diagnosis and reports associated with other vasculitic diseases (such as Kawasaki and polyarteritis nodosa) were excluded from this review. All cases with the mentioned features were included, regardless of age restriction. We recorded common features obtained from study and case reports in the literature: age, gender, cardiac symptoms, type of cardiac involvement and findings of the involvement, and imaging and diagnostic methods (electrocardiogram [ECG], echocardiography and cardiac magnetic resonance imaging [MRI] and histopathological examinations) to determine cardiac involvement, whether there was concomitant renal involvement, and the final results of the patients.
Results
Along with the presented patient, a total of 16 patients were included in this review (Table 2). The ages of the patients ranged from 8 to 71 years old. No female cases were identified in the literature, except in our case. Three of the 16 patients were children (< 18 years). Regarding the symptoms due to cardiac involvement, there was tachycardia in five patients, chest/precordial pain in five patients, respiratory problems in five patients (dyspnea, orthopnea, shortness of breath, hemoptysis), murmur in one patient, and findings of congestive heart failure in two patients. No cardiac symptoms were reported in two patients. Almost all patients underwent biochemical examinations, ECG, and echocardiography, but only three patients had a cardiac MRI. Two patients underwent a cardiac biopsy, and the three patients who died underwent post-mortem necropsy.
Cardiac pathologies detected in the patients were as follows: myocarditis (imaging and/or histopathological) in eight patients, pericardial effusion in four patients (all ≤ 21 years old), ischemia/infarction/necrosis in nine patients (all ≥ 19 years), rhythm disorders in seven patients (four of seven patients were ≤ 19 years old), atrio-ventricular dilatation in two patients, coronary artery changes in two patients, and intra-atrial thrombus in one patient (Table 2). Kidney involvement of HSP occurred in 12 patients at the same time. The presence of renal involvement was proven by biopsy in seven patients, and biopsy was not performed in five patients. Three of five patients had the presence of proteinuria, and two of them had renal failure. In treatment, high-dose prednisolone and cyclophosphamide were used in three patients for immunosuppression, high-dose prednisolone and azathioprine in one patient, and prednisolone alone in seven patients. Non-immunosuppressive treatments (ACE inhibitors, calcium antagonists, beta-blockers, and diuretics) were administered based on the patient’s findings) (Table 2).
Three of the patients died from cardiac involvement secondary to HSP and its related complications. All of those patients were older than 60 years. Although the outcome is unknown in one patient, 11 of the remaining 12 patients had recovered completely in terms of cardiac involvement. However, one patient had a sequel as persistent cardiac dyskinesia (Table 2).
Discussion
To our knowledge, this patient is the first child case in the literature to show thrombus in the right atrium with HSP-related myocarditis. Biopsy-proven HSP nephritis was also detected in this patient. Functional cardiac MRI showed that actually, myocarditis and intra-atrial thrombus were together. Other concomitant causes (viral, autoimmune, and infectious diseases) that might account for the cardiac involvement were excluded, and both cardiac and renal involvements were treated with intensive immunosuppressive therapy.
Cardiac involvement is extremely rare in children with HSP, as well as in adults [1, 2]. To date, secondary cardiac involvement in HSP has been reported in only 16 patients, including this patient. Only three of these 16 patients were children and the remaining 13 were adults. More interestingly, all of the patients in the literature were male and only the case presented here was female. This review suggests that prognosis is worse in adults (three adult patients died; the deceased child patient has not been reported). The high mortality rate in adults might be due to the association of other comorbid conditions (e.g., atherosclerosis and hypertension) that occur with age (Table 2).
In this review, it is noteworthy that the tachycardia, murmur, chest pain, and shortness of breath are the primary findings of the cardiac involvement of the HSP. In adult patients, tachyarrhythmia, precordial (chest) pain, dyspnea, orthopnea, and even non-specific findings might be observed.
Regarding the type of cardiac involvement, myocarditis showed a homogenous distribution according to age. However, we observed that pericardial effusion occurred in children and young adults (all under the age of 21), and myocardial ischemia and infarct/necrosis occurred in adults (all over the age of 19). The first precursor of myocarditis in HSP patients might be rhythm-related changes, especially in children and young patients. It should not be forgotten that echocardiographic examination is insufficient in the diagnosis of myocarditis, whereas functional cardiac MR is diagnostically reliable. In a case of HSP reported by Lutz et al. [4], although no findings other than pericardial effusion were detected in the echocardiographic evaluation performed due to AV block, they detected myocardial involvement in the posterolateral wall on cardiac MR imaging. In our case, suspicious thrombus was detected in the echocardiographic examination conducted depending on the presence of tachycardia without fever, but no evidence of myocardial involvement was detected. Afterward, myocardial involvement was demonstrated, and thrombus was confirmed with functional cardiac MR (Fig. 3). There is strong evidence that myocarditis, present in patients undergoing endomyocardial biopsy and necropsy, is directly IgA-mediated leukocytoclastic vasculitis [9,10,11].
The reason for pericardial effusion that occurs in cardiac involvement in HSP patients has not been fully revealed. Likewise, the cause of coronary artery changes has not been fully established. However, Eleftheriadis et al. [20] reported that HSP causes coronary changes. Since HSP is a vasculitis that involves small vessels in the classification of vasculitis, such a situation might also be attributed to Kawasaki disease, which is concomitant with HSP. The authors concluded that dilatation in the coronary arteries could be secondary to chronic vasculitis developed due to previous HSP. Blomm et al. [21] reported a patient who had coronary artery enlargement with the presence of HSP clinic and who achieved complete recovery with treatment, such as Kawasaki disease. These results might support the hypothesis of the Kawasaki disease that occurred coincidentally during HSP. In contrast, Noval Rivas et al. [22] showed that strong evidence that intestinal IgA production is increased during the acute phase of Kawasaki disease in human patients and in a murine model of Kawasaki disease vasculitis. Moreover, they showed that intestinal epithelial barrier dysfunction in this model results in sIgA leakage and sIgA-C3 complex deposition in to vascular tissues and glomeruli. They concluded that these data suggest that Kawasaki disease may be a form of IgA vasculitis [22].
To date, HSP has not been reported as the sole cause of intracardiac thrombus. Ekici and Çakar [23] reported that in a 3.5-year-old patient with steroid-resistant nephrotic syndrome, intracardiac thrombus was detected in the right atrium with simultaneous HSP. The authors concluded that this condition depended on severe nephrotic syndrome [23]. Although our patient had proteinuria at the nephrotic level, there was no massive edema, and the blood albumin level was 24 g/dL. However, the presence of nephrotic proteinuria, central venous catheter insertion for hemodialysis, and myocardial involvement with the nephritic syndrome in our patient might have facilitated the development of thrombus in the right atrium. Although diuretic therapy can also facilitate the formation of thrombus in such patients, no diuretic has been administered to our case.
The tendency to develop thrombosis which is termed thrombophilia may be due to many causes in children. The reasons of thrombophilia are basically considered in two categories as hereditary or acquired. The mechanisms of hereditary and acquired thrombophilia summarize stasis, hypercoagulable state, and vascular injury. Hypercoagulable states in children with thrombophilia disorders are protein C and protein S deficiencies, antithrombin deficiency, factor V Leiden mutation, prothrombin 20210A mutation, MTHFR gene mutation, and elevated lipoprotein A level [24]. The states of blood flow stasis and vascular injury usually result from central venous lines and some congenital heart diseases. The other causes are septicemia, dehydration, total parenteral nutrition, antiphospholipid syndrome, malignancy, and usage of oral contraceptive. No abnormal finding was detected in our case regarding abovementioned causes except central venous catheter insertion (Table 1).
On the other hand, thrombophilia is an important complication of several forms of systemic vasculitis which are Behçet’s disease, granulomatosis with polyangiitis (formerly Wegener’s), eosinophilic granulomatosis with polyangiitis (Churg Strauss syndrome), microscopic polyangiitis, polyarteritis nodosa, and Takayasu’s arteritis. According to current data, there is a significant relationship between the pathways of inflammation and hemostasis. The mechanisms of the hypercoagulable state in systemic vasculitis remain incompletely understood, common pathways likely exist [25]. However, thrombophilia is not a reported condition in HSP, a common pediatric vasculitis.
Interestingly, valvular involvement due to HSP was not shown in the cases in this review. However, there are some case reports describing valvular involvement stemming from different diseases in some parts of the patients with HSP. The most known of these are patients with valvular involvement due to acute rheumatic fever associated with HSP. In almost all of these patients, valvular involvement was attributed to the presence of acute rheumatic fever at the same time [26,27,28,29,30,31,32]. However, there are also authors who claim the opposite. James et al. [33] presented a case with pulmonary hemorrhage and mitral insufficiency together with HSP as cardiac involvement due to HSP. In this report, the authors suggested that although the Jones criteria had one major (carditis) and two minor (high acute phase reactants, fever) criteria, and evidence of previous group A beta-hemolytic streptococcal infection, the authors suggested that carditis was secondary to severe vascular vasculitis. On the other hand, the cases of acute post-streptococcal glomerulonephritis (APSGN) coexistence and cardiac involvement have been reported with HSP patients [26,27,28,29,30,31,32]. Arslansoyu et al. [32] reported a 7-year-old girl who suffered from HSP, APSGN, and rheumatic carditis. This patient developed palpable purpura and arthritis in both ankles, then carditis had been characterized by mitral/aortic insufficiency, and glomerulonephritis had been characterized by mixed nephritic/nephrotic syndrome. A renal biopsy had shown endocapillary and extracapillary proliferative glomerulonephritis, and the patient was diagnosed with HSP and APSGN. It is noteworthy that valvular involvement is in the foreground in cases accompanied by acute rheumatic fever; however, there is no valve involvement in cases with cardiac involvement directly related to HSP.
The skin biopsy of our patient was compatible with leukocytoclastic vasculitis. In addition, the determination of predominant IgA intense (++) staining and being negative other immunological markers (C1q negative, C3 +, IgG negative) in kidney biopsy examination with immunofluorescence confirmed HSP nephritis. Both her kidney and cardiac involvement were recovered using intensive immunosuppressive therapy.
In conclusion, cardiac involvement is a rare but life-threatening complication of HSP. Cardiac involvement seems a better course in children, and intense immunosuppressive treatment can prevent fatal results. Cardiac symptoms, such as tachycardia, arrhythmia, chest pain, and dyspnea, should be carefully monitored in HSP cases. Biochemical parameters, ECG, and echocardiographic examinations might not always reveal cardiac involvement. Cardiac MRI is an effective method in detecting cardiac involvement in HSP, especially in myocarditis.
References
Yalcindag A, Sundel R (2001) Vasculitis in childhood. Curr Opin Rheumatol 13:422–427. https://doi.org/10.1097/00002281-200109000-00014
Petty RE, Cabral DA (2016) Vasculitis and its classification. In: Petty RE, Laxer RM, Lindsley CB, Wedderburn LR (eds) Textbook of pediatric rheumatology, 7th edn. Elsevier, Philadelphia, pp 448–451
Zaidi M, Singh N, Kamran M, Ansari N, Nasr SH, Acharya A (2008) Acute onset of hematuria and proteinuria associated with multiorgan involvement of the heart, liver, pancreas, kidneys and skin in a patient with Henoch-Schönlein purpura. Kidney Int 73:503–508. https://doi.org/10.1038/sj.ki.5002662
Lutz HH, Ackermann T, Krombach GA, Gröne HJ, Rauen T, Floege J, Mertens PR (2009) Henoch-Schönlein purpura complicated by cardiac involvement: case report and review of the literature. Am J Kidney Dis 54:9–15. https://doi.org/10.1053/j.ajkd.2009.04.017
Agraharkar M, Gokhale S, Le L, Rajaraman S, Campbell GA (2000) Cardiopulmonary manifestations of Henoc Schönlein purpura. Am J Kidney Dis 35:319–322. https://doi.org/10.1016/s0272-6386(00)70344-1
Osman A, Mc Creery CJ (2000) Cardiac vasculitis in Henoch Schönlein purpura. Circulation 101:69–70
Polizzotto MN, Gibbs SD, Beswick W, Seymour JF (2006) Cardiac involvement in Henoch-Schönlein purpura. Intern Med J 36:328–331
Abdel-Hadi O, Greenstone MA, Hartley RB, Kidner PH (1981) Myocardial infarction—a rare complication in Henoch Schönlein purpura. Postgrad Med J 57:390–392. https://doi.org/10.1136/pgmj.57.668.390
Satoh M, Mikuniya A, Mikami M, Higashiyama A, Sasaki N, Tahkahashi M, Fukushi K, Onodera K, Oike Y (1991) A case of Schönlein-Henoch purpura with myocardial complications. Kokyu To Junkan 39:273–277
Carmichael P, Brun E, Jayawardene S, Abdulkadir A, O’Donnell PJ (2002) A fatal case of bowel and cardiac involvement in Henoch-Schönlein purpura. Nephrol Dial Transplant 17:497–499. https://doi.org/10.1093/ndt/17.3.497
Kereiakes DJ, Ports TA, Finkbeiner W (1984) Endomyocardial biopsy in Henoch-Schönlein purpura. Am Heart J 107:382–385. https://doi.org/10.1016/0002-8703(84)90390-9
Cimaz R, Boccazzi A, Milone V, Careddu P (2000) Pericarditis as a presenting feature of Henoch-Schönlein purpura. Clin Exp Rheumatol 18:785
Sundriyal D, Grupta BB, Sharma B, Chawla MPS (2013) Cardiac involvement in Henoch-Schönlein purpura. JIACM 14:173–174
Hayakawa K, Shiohara T (2003) Two cases of Henoch-Schonlein purpura with transient myocardial ischemia. Acta Derm Venereol 83:393–394. https://doi.org/10.1080/00015550310012601
Michas G, Grigoriou K, Syrigos D, Alexopoulos N, Evdoridis C, Trikas A (2017) A rare cause of myocarditis resulting in acute heart failure in the setting of Henoch-Schönlein purpura. Hell J Cardiol 58:439–442. https://doi.org/10.1016/j.hjc.2017.05.002
Bando K, Maeba H, Shiojima I (2018) IgA vasculitis with simultaneous cardiopulmonary involvement. Intern Med 57:829–834. https://doi.org/10.2169/internalmedicine.9681-17
Flynn JT, Kaelber DC, Baker-Smith CM et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents [published correction appears in pediatrics]. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Ozen S, Ruperto N, Dillon MJ, Bagga A, Barron K, Davin JC, Kawasaki T, Lindsley C, Petty RE, Prieur AM, Ravelli A, Woo P (2006) EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Ann Rheum Dis 65:936–941. https://doi.org/10.1136/ard.2005.046300
Banka P, Robinson JD, Uppu SC, Harris MA, Hasbani K, Lai WW, Richmond ME, Fratz S, Jain S, Johnson TR, Maskatia SA, Lu JC, Samyn MM, Patton D, Powell AJ (2015) Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson 17:96. https://doi.org/10.1186/s12968-015-0201-6
Eleftheriadis D (2007) Severe coronary artery disease in the setting of Henoch–Schoenleinpurpura. Int J Cardiol 118:262–263. https://doi.org/10.1016/j.ijcard.2006.07.023
Bloom JL, Darst JR, Prok L, Soep JB (2018) A case of Henoch-Schonlein purpura with dilated coronary arteries. Pediatr Rheumatol Online J 16:54. https://doi.org/10.1186/s12969-018-0270-9
Noval Rivas M, Wakita D, Franklin MK et al (2019) Intestinal permeability and IgA provoke immune vasculitis linked to cardiovascular inflammation. Immunity 51:508–521.e6. https://doi.org/10.1016/j.immuni.2019.05.021
Ekici F, Çakar N (2013) A large intracardiac thrombus in a child with steroid-resistant nephrotic syndrome. Cardiol Young 23:440–442. https://doi.org/10.1017/S1047951112000923
Yang JY, Chan AK (2013) Pediatric thrombophilia. Pediatr Clin N Am 60:1443–1462. https://doi.org/10.1016/j.pcl.2013.09.004
Springer J, Villa-Forte A (2013) Thrombosis in vasculitis. Curr Opin Rheumatol 25:19–25. https://doi.org/10.1097/BOR.0b013e32835ad3ca
Kalyoncu M, Cakır M, Erduran E, Okten A (2006) Henoch-Schönlein purpura: a case with atypical presentation. Rheumatol Int 26:669–671. https://doi.org/10.1007/s00296-005-0032-0
Guven H, Ozhan B, Bakiler AR, Salar K, Kozan M, Bilgin S (2006) A case of Henoch Schönlein purpura and rheumatic carditis with complete atrioventricular block. Eur J Pediatr 165:395–397. https://doi.org/10.1007/s00431-006-0094-3
Eisenstein EM, Navon-Elkan P (2002) Acute rheumatic fever associated with Henoch-Schönlein purpura: report of three cases and review of the literature. Acta Paediatr 91:1265–1267. https://doi.org/10.1080/080352502320777559
Gulati T, Kumar P, Dewan V, Anand VK (2004) Henoch-Schönlein purpura with rheumatic carditis. Indian J Pediatr 71:371–372. https://doi.org/10.1007/BF02724113
Shin JI, Kim JH, Lee JS, Kim DS, Choi JY, Sul JH (2007) Cardiac manifestations of Henoch-Schöenlein purpura: IgA mediated vasculitis or rheumatic fever? Eur J Pediatr 166:627. https://doi.org/10.1007/s00431-006-0273-2
Ocal B, Karademir S, Oguz D, Erdogan OA, Senocak F (2000) Acute rheumatic carditis in Henoch-Schönlein purpura. Int J Cardiol 74:97–98. https://doi.org/10.1016/s0167-5273(00)00268-0
Arslansoyu Çamlar S, Soylu A, Akil İ, Ünlü M, Coşkun Ş, Ertan P, Kavukçu S (2018) Henoch-Schonlein purpura, post-streptococcal glomerulonephritis and acute rheumatic carditis after group A β-haemolytic streptococcal infection. Paediatr Int Child Health 38:73–75. https://doi.org/10.1080/20469047.2017.1284394
James CA, Gonzalez I, Khandhar P, Freij BJ (2017) Severe mitral regurgitation in a child with Henoch-Schönlein purpura and pulmonary hemorrhage. Glob Pediatr Health 4:2333794X17726940. https://doi.org/10.1177/2333794X17726940
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Neslihan Yılmaz, Selçuk Yüksel, Tülay Becerir, İlknur Girişgen, Furkan Ufuk, Dolunay Gürses, Münevver Yılmaz, and Nagihan Yalçın. The first draft of the manuscript was written by Neslihan Yılmaz. All authors commented on all versions of the manuscript. Supervision and critical review of the paper was performed by Selçuk Yüksel. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Code availability
Not applicable.
Consent to participate
Permission for participation and publications was obtained from the patient and their parents.
Consent for publication
Permission for participation and publications was obtained from the patient and her parents.
Availability of data and material
The data sets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yılmaz, N., Yüksel, S., Becerir, T. et al. Myocarditis and intracardiac thrombus due to Henoch-Schönlein purpura: case report and literature review. Clin Rheumatol 40, 1635–1644 (2021). https://doi.org/10.1007/s10067-020-05317-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05317-8