Abstract
Socio-economic gradients in occurrence of diseases have been reported for many chronic conditions. However, whether the magnitude of socio-economic gradients differs across diseases and the extent to which lifestyle mediates such relationships are not known. Cross-sectional data from The National Monitor on Musculoskeletal System was used. Respondents (> 18 years) completed a questionnaire including gender, education, social status, lifestyle, and physician-diagnosed diseases. Logistic regressions investigated the relationship between education and the major chronic diseases (musculoskeletal diseases (MSKD), diabetes, cardiovascular (CVD), cancer, mental, respiratory, any disease). Next, analyses were repeated in individuals with potential to have paid work (i.e., those < 65 having paid work, being unemployed, or receiving living allowance (minimum income)). The mediating role of smoking and BMI between education and occurrence of diseases was assessed by testing indirect effects. From 8904 individuals (mean age 54 years, 46% male), 4378 (49%) had at least one disease. Gradients in occurrence of disease by education were present for all diseases except cancer and mental disease, with the strongest gradient in diabetes (OR 2.0 [95%CI 1.4;2.8]). Unemployment and especially living on minimum income were associated with increased odds to have MSKD and mental and respiratory disease, after adjusting for education. Smoking and obesity mediated part of the relationship between education and disease, with obesity playing more pronounced role. Association between deprivation and occurrence of all major chronic diseases is of comparable magnitude, with education having most consistent contribution. Our results support the notion of the generic (i.e., non-disease specific) mechanisms underlying socio-economic gradients in health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic diseases present the largest part of the disease burden in developed countries, leading to loss of health and premature deaths [1]. According to the most recent Burden of Disease report, musculoskeletal diseases (MSKDs) together with cardiovascular (CVD), respiratory and mental diseases, cancer, and diabetes are among the diseases causing the highest health burden in Western countries and this burden has increased over the last decades despite the rapid development of new medical technologies [1].
Previous studies in a number of MSKDs such as rheumatoid arthritis, gout, osteoarthritis, and systemic lupus erythematosus consistently showed that low socio-economic (SE) status measured by income, education, age, race, ethnical background, or area deprivation was associated with increased occurrence and poorer outcome of disease in many countries [2,3,4,5,6,7,8]. Similar observations have been made for almost all chronic diseases studied. On that line, some researchers suggest that socio-economic inequities may be generic and independent of the type of disease [9,10,11,12,13,14]. However, a direct comparison of the impact of the socio-economic factors on the presence of different chronic diseases is scarce.
Socio-economic factors that identify groups at risk for health inequities are brought together in the PROGRESS-plus framework, which is an acronym for Place of Residence, Race/Ethnicity, Occupation, Gender, Religion, Education, Socio-economic status (SES), Social Capital, and Plus for Age, Disability, Sexual Orientation and Literacy [15,16,17,18]. However, the relative importance of various socio-economic factors in the occurrence of different clinical conditions has not been thoroughly explored. Most studies concentrate on the role of one specific determinant and it remains unclear whether they reinforce each other or have mainly independent impact. Last but not least, it is not only particularly important to uncover which specific socio-economic factors influence disparities, but also to understand which common underlying behaviours, such as lifestyle, might explain their influence.
Insight into the specific socio-economic factors that infer the highest risk for health disparities and into the specific diseases for which patients with low socio-economic status are at risk would be useful, especially as recent evidence shows that the socio-economic gap in health is widening not only between poor and rich countries but also within countries. Such insights would help to integrate actions targeted to halt the increasing health disparities in deprived groups [19].
The objective of this study was (1) to assess and compare the contribution of the available PROGRESS factors and the occurrence of MSKD, CVD, diabetes, mental and respiratory diseases, and cancer, and (2) if relevant relationships are found, to explore the possible mediating role of BMI and smoking.
Patients and methods
Subjects
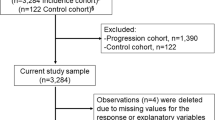
Data from The National Monitor on Musculoskeletal System (2010) was used [20]. Information on socio-demographics, lifestyle, and major chronic diseases was collected. The questionnaire was sent to a random sample of 40,000 household addresses, selected from an address registry of a subsidiary undertaking of the Dutch Thomas Nationwide Transport (TNT) post [20, 21]. In each household, the person who was 18 years or older and was first to have next birthday was asked to complete the questionnaire. The study was approved by the Ethical Committee of the Leiden University Medical Centre. Participants provided consent for use of anonymized data for research purposes and no specific consent was necessary for the analyses presented in this manuscript.
Assessments
Participants completed a questionnaire including several PROGRESS factors (age, gender, highest attained educational level (no education or primary education, lower professional education, middle or professional secondary education, secondary general education, and university diploma), social status (paid work, (early) retirement, unemployed, work disabled, receiving state living allowance, housewife/man, or student), ethnic origin (respondent’s place of birth and parents’ place of birth), and place of residence (4-digit postal code)). The standard definition of Statistics Netherlands was further used to define ethnic origin [22], i.e., a person was considered to be of non-Western origin if at least one of the parents was born in a non-Western country or continent, i.e., Turkey, Africa, Latin America, or Asia.
The presence of 13 common chronic diseases was inquired, with three possible answer categories (no; yes, but not diagnosed by a physician; yes, and diagnosed by a physician). Only diagnoses made by a physician were considered for the analyses. Ten of the 13 diagnoses of interest were combined, resulting in six groups of chronic diseases as revealed by the Burden of Disease project as most important: MSKD (severe or persistent symptoms in/or around joints (pain, stiffness, and/or swelling)), CVD (hypertension, cerebral haemorrhage, myocardial infarction, other heart diseases, and peripheral vascular disease), diabetes, cancer, mental disorders, and respiratory diseases. The category “any morbidity” groups subjects with at least one of the conditions of the six groups listed above, or either skin disease, bowel disease, or migraine. Finally, smoking status (never smoked, smoked before, current smoking) and height (cm) and weight (kg) were collected. Body mass index (BMI) was computed and categorized into underweight (BMI < 18.5 kg/m2), normal weight (18.5 < BMI < 25.0), overweight (25.0 < BMI ≤ 30.0), and obese (BMI > 30.0) [23, 24].
Statistical analysis
To investigate the relationship between the socio-economic determinants with the occurrence of selected chronic diseases (MSKD, diabetes, CVD, cancer, mental disorder, respiratory disease) and the occurrence of any chronic disease, series of logistic regressions with separate models for each outcome (disease) were computed. First, univariable logistic regressions were performed with several available PROGRESS factors (education, age, gender, and origin) and potential confounders (smoking and BMI) as independent variables and the presence of the disease of interest as the dependent variable. Second, those factors that were significant in the univariable models for at least one of the diseases (cutoff p value < 0.10), were entered into the multivariable models (model I). Further, a multivariable multilevel logistic regression model with individuals nested within place of residence was computed to explore possible effects of place of residence. The likelihood ratio test was used to decide whether a two-level model showed significantly better fit compared to a one-level model (cutoff p value < 0.05). Next, the sample was limited to individuals who had potential to have a paid work (i.e., those having paid work, unemployed, or receiving minimum income, and < 65 years old). New statistical models were built using the procedure described above, with social status added among explanatory variables (model II). The two final models (model I and model II) with the presence of each of the six diseases groups of interest and the presence of any morbidity had an identical set of independent variables so that impact of relevant PROGRESS factors with regard to the occurrence of diseases could be compared. Interactions between education, social status, age, and gender were tested, and if significant (a priori defined as p value < 0.05), analyses were repeated in strata.
The mediating role of smoking and BMI in the relationship between level of education and occurrence of the diseases (except mental, for which no plausible hypothesis could be made) was assessed by calculating indirect effects and the proportion of the total effect mediated by the indirect effect using the product of coefficient approach [25].
As alternative analyses to the logistic regressions, modified Poisson regressions were performed, because in a number of models, the outcome occurred in > 10% of subjects (so-called common outcome) and methodological literature suggests that in this case, odds ratio (OR) is not a good estimate of a prevalence ratio (PR) [26].
Missing cases on age, gender, education, social status, origin, smoking status, and BMI were imputed using multiple imputation (imputed datasets n = 20). Chained imputations using a regression-based method were used [27,27,29]. Predictive mean matching was used for a continuous variable, logistic regression for binary variables, and multinomial logistic regression for a nominal variable. Main analyses were performed on imputed data. To assess robustness of findings, we repeated the statistical models in complete cases (no missing value in any variable) only and compared the results. Stata Statistical Software v12 was used [30].
Results
Study sample
Total group
In the total group of 8904 individuals (response rate 22.4%), MSKD confirmed by a physician was reported by 1766 (20%) participants, 547 (6%) persons reported diabetes, 1855 (21%) CVD, 270 (3%) cancer, 526 (6%) a mental disorder, 679 (8%) a respiratory disease, and 4378 (49%) had at least one disease. Mean age was 54 (SD 16) years and 46% of participants were men. Thirty-nine percent (n = 3360) had university education (largest group), and 5% had lowest level of educational attainment (n = 420), equivalent to no education or primary education degree only. Ninety-five percent of respondents were of Western origin (n = 8332) (Table 1).
Subset of persons < 65 with a potential to have a paid work
In the sample limited to subjects younger than 65 years and potential to have paid work (i.e., having paid work, unemployed, or receiving state living allowance) (n = 5046 (57%)), MSKD confirmed by a physician was reported by 773 (15%) participants, diabetes by 134 (3%) persons, CVD by 549 (11%), cancer by 70 (1%), respiratory disease by 289 (6%) and a mental disorder by 255 (5%). In total, 1946 (39%) had at least one disease. Mean age was 45 (SD 11) years and 45% of the participants were men. Ninety-five percent (n = 4805) had a paid job, 4% (n = 184) were unemployed, and 1% of respondents (n = 57) were receiving minimum income (Table 1).
PROGRESS factors and prevalence of chronic diseases
Total group
In the multivariable models based on the total group (sample model I), gradients in prevalence of disease by level of educational attainment were present for all diseases except for cancer and mental disease. Educational differences in the prevalence of disease were strongest in diabetes (OR 2.0 [95%CI 1.4;2.8] for a person with primary school education vs university diploma), followed by respiratory diseases, MSKD, and CVD (1.7 [1.3;2.6], 1.9 [1.3;2.2], and 1.4 [1.1;1.8], respectively). Older age was always a risk factor with the exception of mental diseases, where older persons showed lower odds to have mental disease. Female gender was associated with presence of MSKD, mental and respiratory diseases (1.8 [1.6;2.0], 1.9 [1.6;2.4], and 1.6 [1.3;1.8], respectively), and decreased occurrence of diabetes (0.7 [0.6;0.8]), while there were no gender differences in the occurrence of cancer or CVD. Origin appeared to be a risk factor only for the occurrence of diabetes, as persons of the 1st-generation non-Western origin (one of the parents born in a non-Western country) had 1.8 [1.2;2.9] higher odds to have diabetes compared to those of Western origin. For all other conditions, origin did not play a significant independent role in occurrence of the disease. In the model with any morbidity as an outcome, lower education, older age, female gender, and non-Western origin were risk factors (Table 2, Fig. 1 (model I)).
Association between education (Model I) and social status (Model II) with the occurrence of musculoskeletal diseases (MSKD), diabetes, cardiovascular diseases (CVD), cancer, mental disorders, respiratory diseases and any morbidity. Odds ratios are derived from multivariable logistic regression models, adjusted for age, gender, BMI, smoking and, model I, additionally for origin
Subset of persons < 65 with a potential to have a paid work
In the subgroup limited to subjects with potential to have paid work (sample model II), those being unemployed or relying on living allowance were more likely to have a MSKD (1.6 [95% CI 1.1;2.3] and 2.8 [1.6;5.0], respectively) or mental disorder (3.2 [2.1;5.1] and 7.1 [3.6;14.4], respectively) when compared to those who had a paid employment, and those relying on living allowance were also more likely to be diagnosed with a respiratory disease (3.0 [95%CI 1.4;6.2]). In the other diseases, except cancer, the influence of unemployment and reliance on a living allowance went in the same directions but did not reach statistical significance (Table 3, Fig. 1 (model II)). Odds to have any morbidity were also higher in those with adverse social status (Tables 2 and 3, Fig. 1). When exploring the relation between education and social status, persons with lower education were also more frequently unemployed or receiving living allowance (data not shown). While education continued to have an independent contribution to the occurrence of MSKD, CVD, and respiratory disease, the effect was attenuated compared to the univariable relation (Table 3, Online Tables 1 and 2).
The two-level model did not show a better fit compare to one-level structure in models I and II, indicating that place of residence (measure at 4-digit postal code) did not have a relevant contribution. Interactions were not significant or not clinically relevant after stratification. PR estimates (derived modified Poisson regression model) were in the same direction but lower than estimated ORs (Online Tables 3 and 4). Complete case analyses yielded similar results as those computed after multiple imputations.
Role of smoking and obesity in the relationship between education and occurrence of disease
In the total sample, 5, 5, and 1% of relationship between low education and higher likelihood of occurrence of MSKD, respiratory disease, and diabetes were mediated by smoking behaviour, respectively. No or negligible mediation effect was observed for CVD and cancer. Obesity mediated 29, 26, 59, and 75%, for MSKD, respiratory disease, diabetes, and CVD, respectively, for the lowest vs the highest education category.
Discussion
For the majority of conditions studied, gradients in the presence of disease across educational level or social status were observed, where persons with lower education and lower social status tended to more frequently report having the disease. Female gender was associated with higher odds to have any of the diseases studied, expect for diabetes and CVD, which is a pattern previously shown in the literature [31]. Gender differences have essentially a mixed character reflecting the biologic and social differences. On the same line, older age is a classic risk factor for the majority of diseases, as confirmed in our analyses. As an exception, mental diseases were slightly more prevalent in younger adults. While ethnical origin was only a significant risk factor for diabetes, negative findings for other diseases should be interpreted with caution due to very low numbers of non-Western respondents [32]. Unexpectedly, smoking was not a significant risk factor for CVD or diabetes in a model adjusted for BMI. While it is plausible that obesity is a stronger risk factor for both conditions, we cannot exclude potential over adjustment or the fact that individuals quitted smoking after being diagnosed with the disease (while changes in BMI are more difficult to achieve).
As these results were obtained in a country with comprehensive and accessible health insurance coverage, it is unlikely that the effect of socio-economic differences can be attributed to differential access to health care services; however, there is some concern that health promotion and behavioural change interventions do not always reach the lower socio-economic groups [33]. While in the conventional modelling approach, the observed effect of education and social status remained after adjusting for the major lifestyle factors such as obesity (proxy for unhealthy nutrition and low physical activity), additional analyses showed they also played a mediating role. Smoking and obesity mediated part of the relationship between education and disease occurrence in case of MSKD, respiratory diseases, and diabetes, whereas the pathway to CVD was only mediated by obesity. Within limitations of the mediation analyses in a cross-sectional data, our major observation was that obesity played a more pronounced role compared to smoking. Notwithstanding, additional mechanisms are also known to underlie this relationship, such as genetics, stress, low health literacy, and suboptimal communication with physicians with regard to disease prevention.
When social status and education were added to the models, effect of both became notably weaker due to known clustering of social deprivation factors (i.e., lower educated are more frequently less employed). Of note, in several conditions, namely MSKD and mental and respiratory, social status appeared to have stronger association than education. However, the numbers of unemployed and receiving minimum income were small, and, importantly, causality of association between social status and health can be challenged. While education is likely to be acquired early in life and before chronic diseases develop (an assumption that we could not test empirically in the existing data), social status can be both a cause and consequence morbidities. Cross-sectional design as the absence of data on disease onset hindered further investigation of these patterns.
Differences in morbidity by socio-economic position have been reported previously. Cavelaars et al. have reported in 1998 to comparable gradients in chronic morbidity among men across occupational class in several Western European countries [34]. Study by Dalstra et al. based on health surveys from the 1990s among 3700 to 41,200 subjects per country across eight European countries demonstrated that lower educated individuals tended to more frequently have a cardiovascular, musculoskeletal, and neurological diseases, but not cancer, kidney, or skin diseases [35]. Our study reveals that these gradients remain visible more than two decades later and persist even after adjusting for well-known risk factors such as smoking and obesity indicating that these lifestyles cannot fully explain the existing inequalities. Furthermore, another study has shown that socially disadvantaged persons with chronic diseases report worse physical and mental health-related quality of life compared to those with a disease but more favourable socio-economic status [36]. The current study additionally shows that socially disadvantaged persons are also more likely to have a disease, thus emphasizing the double vulnerability of these population groups. Further research should aim at uncovering the specific pathways between socio-economic disadvantage and health (such as issues around broader understanding of health literacy including knowledge around health, empowerment, access to and uptake of health care), which could be potentially addressed in health care but also outside health care sector.
Several limitations should be mentioned. First, generalizability of the findings might be limited due to a low response rate (22.4%). However, such response is common for such surveys that otherwise provide a valuable population level data, and it has been argued that low response is not necessarily an indicator of the poor quality [37, 38]. We additionally compared socio-demographic characteristics of the sample with data from the Statistics Netherlands, and study sample was comparable to the general population, except lower representation of lower educated respondents. It is expected, as surveys are likely to leave out the most disabled, least literate and in other senses deprived groups, which could lead to underestimation of the socio-economic gaps. Second, while self-reported nature of data collected on the diseases may be less accurate, previous research showed good agreement with the data from medical records [39, 40]. Furthermore, respondents were asked to only report the diagnoses confirmed by a doctor, which increases the reliability of the collected data [39, 40]. National Dutch statistics estimates that 48% of the adult population has at least one chronic disease, and this corresponds well with 49% observed in our data [41]. Next, a number of PROGRESS factors were not available in the survey, namely, reliable data on occupation, religion, income, social capital, and sexual orientation and literacy. Hopefully, our study stimulates researchers to include these factors in future observational studies. Last but not least, generalizability of our findings to countries with less socio-economic welfare and less liberal access to health services may not be possible; however, it is plausible to assume that limited access to health and social care would sharpen the differences observed in a more favourable context [42].
To our knowledge, this is the first study that explored and compared the role of several PROGRESS factors across several diseases in a large, national-level dataset. We have found that effect of socio-economic factors (in particular, education) is largely independent of the disease, emphasizing the presence of generic mechanisms underlying the disadvantage and calling for a non-disease-specific approach in health promotion and disease prevention. Although lifestyle factors played a relevant role in explaining socio-economic differences in occurrence of chronic diseases, they did not explain the entire impact. Other exposures, biological factors, and their interaction should be further explored.
References
Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–2223
Hayward RA, Rathod T, Roddy E, Muller S, Hider SL, Mallen CD (2013) The association of gout with socioeconomic status in primary care: a cross-sectional observational study. Rheumatology (Oxford) 52(11):2004–2008
Brennan SL, Turrell G (2012) Neighborhood disadvantage, individual-level socioeconomic position, and self-reported chronic arthritis: a cross-sectional multilevel study. Arthritis Care Res (Hoboken) 64(5):721–728
Callahan LF, Cleveland RJ, Shreffler J, Schwartz TA, Schoster B, Randolph R, Renner JB, Jordan JM (2011) Associations of educational attainment, occupation and community poverty with knee osteoarthritis in the Johnston County (North Carolina) osteoarthritis project. Arthritis Res Ther 13(5):R169
Massardo L, Pons-Estel BA, Wojdyla D, Cardiel MH, Galarza-Maldonado CM, Sacnun MP, Soriano ER, Laurindo IM, Acevedo-Vásquez EM, Caballero-Uribe CV, Padilla O, Guibert-Toledano ZM, da Mota LM, Montufar RA, Lino-Pérez L, Díaz-Coto JF, Achurra-Castillo AF, Hernández JA, Esteva-Spinetti MH, Ramírez LA, Pineda C, Furst DE (2012) Early rheumatoid arthritis in Latin America: low socioeconomic status related to high disease activity at baseline. Arthritis Care Res (Hoboken). 64(8):1135–1143
Harrison MJ, Tricker KJ, Davies L, Hassell A, Dawes P, Scott DL, Knight S, Davis M, Mulherin D, Symmons DP (2005) The relationship between social deprivation, disease outcome measures, and response to treatment in patients with stable, long-standing rheumatoid arthritis. J Rheumatol 32(12):2330–2336
Camacho EM, Verstappen SM, Symmons DP (2012) Association between socioeconomic status, learned helplessness, and disease outcome in patients with inflammatory polyarthritis. Arthritis Care Res (Hoboken). 64(8):1225–1232
Singh JA (2013) Racial and gender disparities among patients with gout. Curr Rheumatol Rep 15(2):307
Mackenbach JP (1992) Socio-economic health differences in The Netherlands: a review of recent empirical findings. Soc Sci Med 34(3):213–226
Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, Kunst AE, European Union Working Group on Socioeconomic Inequalities in Health (2008) Socioeconomic inequalities in health in 22 European countries. N Engl J Med 358(23):2468–2481
Stirbu I, Looman C, Nijhof GJ, Reulings PG, Mackenbach JP (2012) Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Community Health 66(12):1159–1166
Wilkinson R, Marmot M (2003) Social determinants of health. The solid facts, 2nd edn. WHO Regional Office for Europe, Copenhagen
Mackenbach JP, Kunst AE, Cavelaars AE, Groenhof F, Geurts JJ (1997) Socioeconomic inequalities in morbidity and mortality in western Europe. The EU Working Group on Socioeconomic Inequalities in Health. Lancet 349(9066):1655–1659
Chandola T (1998) Social inequality in coronary heart disease: a comparison of occupational classifications. Soc Sci Med 47(4):525–533
O'Neill J, Tabish H, Welch V, Petticrew M, Pottie K, & Clarke M (2014) Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 67:56–64
Evans T, Brown H (2003) Road traffic crashes: operationalizing equity in the context of health sector reform. Inj Control Saf Promot 10(1–2):11–12
Evans TWM, Diderichsen F, Bhuiya A, Wirth M (editors) (2001) Introduction. in: Challenging inequities in health: from ethics to action: Oxford University Press
Whitehead M (1991) The concepts and principles of equity and health. Health Promotion Int 6(3):217–228
Mol GD, van de Lisdonk EH, Smits JP, van den Hoogen JM, Bor JH, Westert GP (2005) A widening health gap in general practice? Socio-economic differences in morbidity between 1975 and 2000 in The Netherlands. Public Health 119(7):616–625
Chorus A, Schokker D (2010) National monitor on musculoskeletal system 2010. Leiden
Elske van den Akker-van Marle M, Chorus AM, Vliet Vlieland TP, van den Hout WB (2012) Cost of rheumatic disorders in the Netherlands. Best Pract Res Clin Rheumatol 26(5):721–731
Keij-Deerenberg I (2000) Numbers of foreigners according to several definitions (Aantallen allochtonen volgens verschillende definities). Maandstatistiek Bevolking 5:14–17
WHO (2000) Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva
Mackinnon D, Dwyer J (1993) Estimating mediated effects in prevention studies. Eval Rev 17:144–158
Lieffers JR, Baracos VE, Winget M, Fassbender K (2011) A comparison of Charlson and Elixhauser comorbidity measures to predict colorectal cancer survival using administrative health data. Cancer 117(9):1957–1965
Schafer JL (1999) Multiple imputation: a primer. Stat Methods Med Res 8(1):3–15
Royston P (2005) Multiple imputation of missing values: update. Stata J 5:188–201
van Buuren S, Boshuizen HC, Knook DL (1999) Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 18(6):681–694
StataCorp (2011) Stata statistical software: release 12. StataCorp LP, College Station
Abad-Diez JM, Calderon-Larranaga A, Poncel-Falco A, Poblador-Plou B, Calderon-Meza JM, Sicras-Mainar A et al (2014) Age and gender differences in the prevalence and patterns of multimorbidity in the older population. BMC Geriatr 14:75
Bos V, Kunst AE, Keij-Deerenberg IM, Garssen J, Mackenbach JP (2004) Ethnic inequalities in age- and cause-specific mortality in The Netherlands. Int J Epidemiol 33(5):1112–1119
Beenackers M, Nusselder W, Oude Groeniger J, van Lenthe V (2015) Het terugdringen van gezondheidsachterstanden: een systematisch overzicht van kansrijke en effectieve interventies
Cavelaars AE, Kunst AE, Geurts JJ, Helmert U, Lundberg O, Mielck A, Matheson J, Mizrahi A, Mizrahi A, Rasmussen N, Spuhler T, Mackenbach JP (1998) Morbidity differences by occupational class among men in seven European countries: an application of the Erikson-Goldthorpe social class scheme. Int J Epidemiol 27(2):222–230
Dalstra JA, Kunst AE, Borrell C, Breeze E, Cambois E, Costa G, Geurts JJM, Lahelma E, van Oyen H, Rasmussen NK, Regidor E, Spadea T, Mackenbach JP (2005) Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol 34(2):316–326
Putrik P, Ramiro S, Chorus AM, Keszei AP, Boonen A (2015) Socioeconomic inequities in perceived health among patients with musculoskeletal disorders compared with other chronic disorders: results from a cross-sectional Dutch study. RMD Open 1(1):e000045
Groves RM (2006) Nonresponse rates and nonresponse bias in household surveys. Public Opin Q 70(5):646–675
American association for public opinion research (AAPOR) (2014) [Available from: http://www.aapor.org/Response_Rates_An_Overview1.htm#.U8LxqrFjPO6
Wijnands JM, Boonen A, Arts IC, Dagnelie PC, Stehouwer CD, van der Linden S (2011) Large epidemiologic studies of gout: challenges in diagnosis and diagnostic criteria. Curr Rheumatol Rep 13(2):167–174
Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I (1997) Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol 145(8):762–769
CBS (2012) Central Bureau of Statistics (The Netheralands). Gezondheid aandoeningen beperkingen; persoonskenmerken
Hosseinpoor AR, Bergen N, Mendis S, Harper S, Verdes E, Kunst A, Chatterji S (2012) Socioeconomic inequality in the prevalence of noncommunicable diseases in low- and middle-income countries: results from the World Health Survey. BMC Public Health 12:474
Funding
The data collection was initiated and financially supported by the Dutch Arthritis Foundation.
Author information
Authors and Affiliations
Contributions
AB has conceived the idea; PP and SR have performed the analyses and drafted the first version of the manuscript. All authors have contributed to the interpretation of results and critically reviewed and approved the last version.
Corresponding author
Ethics declarations
The study was approved by the Ethical Committee of the Leiden University Medical Centre. Participants provided consent for use of anonymized data for research purposes and no specific consent was necessary for the analyses presented in this manuscript.
Disclosures
None.
Additional information
P. Putrik and S. Ramiro are joint first authors.
Electronic supplementary material
ESM 1
(DOCX 34 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Putrik, P., Ramiro, S., Chorus, A.M. et al. Socio-economic gradients in the presence of musculoskeletal and other chronic diseases: results from a cross-sectional study in the Netherlands. Clin Rheumatol 37, 3173–3182 (2018). https://doi.org/10.1007/s10067-018-4158-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-018-4158-3