Abstract
This study aims to identify effective ways to design virtual rehabilitation to obtain physical improvement (e.g. balance and gait) and support engagement (i.e. motivation) for people with osteoporosis or other musculoskeletal disorders. Osteoporosis is a systemic skeletal disorder and is among the most prevalent diseases globally, affecting 0.5 billion adults. Despite the fact that the number of people with osteoporosis is similar to, or greater than those diagnosed with cardiovascular disease and dementia, osteoporosis does not receive the same recognition. Worldwide, osteoporosis causes 8.9 million fractures annually; it is associated with substantial pain, suffering, disability and increased mortality. The importance of physical therapy as a rehabilitation strategy to avoid osteoporosis fracture cannot be over-emphasised. However, the main rehabilitation challenges relate to engagement and participation. The use of virtual rehabilitation to address such challenges in the delivery of physical improvement is gaining in popularity. As there currently is a paucity of literature applying virtual rehabilitation to patients with osteoporosis, the authors broadened the search parameters to include articles relating to the virtual rehabilitation of other skeletal disorders (e.g. Ankylosing spondylitis, spinal cord injury, motor rehabilitation, etc.). This systematic review initially identified 130 titles, from which 23 articles (involving 539 participants) met all eligibility and selection criteria. Four groups of devices supporting virtual rehabilitation were identified: a head-mounted display, a balance board, a camera and more specific devices. Each device supported physical improvement (i.e. balance, muscle strength and gait) post-training. This review has shown that: (a) each device allowed improvement with different degrees of immersion, (b) the technology choice is dependent on the care need and (c) virtual rehabilitation can be equivalent to and enhance conventional therapy and potentially increase the patient’s engagement with physical therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
As one of the most common skeletal disorders in the world (Ho et al. 2021), osteoporosis is a disorder affecting the body’s musculoskeletal (muscular and skeletal) system (Ho et al. 2021) and results in the inner structure of bones breaking down, becoming more fragile and prone to breaking (Sözen 2017; Erjiang et al. 2020; Kanis et al. 2021). Osteoporosis is called a silent disease as there is usually no symptom until an osteoporotic fracture occurs (Sözen 2017; Erjiang et al. 2020). An osteoporotic fracture, also known as fragility fracture, usually occurs after a fall (Sözen 2017; Erjiang et al. 2020). While falls can occur at any time in life, their severity and frequency increase with ageing (Australian Commission on Safety and Quality in Health Care 2009). A fall is defined in this context as any event resulting in a person coming inadvertently to rest on the ground or any other lower level (Sözen 2017; Erjiang et al. 2020; Australian Commission on Safety and Quality in Health Care 2009). When the fall is the cause of the fracture, it is called an ‘injurious fall’ (Australian Commission on Safety and Quality in Health Care 2009). In 2019, 25.5 million women and 6.6 million men were estimated to have osteoporosis (European Union plus Switzerland, plus United Kingdom), whilst 4.3 million patients suffered from an osteoporotic fracture (Willers et al. 2022). The hospitalization rate for osteoporotic fractures is predicted to increase by 150% in 2046 (McCabe et al. 2020). Meanwhile, the projected growth in the population up to 2034, for those aged over 50 years, is 11.4% for men and women (Willers et al. 2022). Physical exercise is a powerful non-pharmaceutical fracture prevention strategy for people with osteoporosis or those at risk of falls (Dionyssiotis et al. 2014). However, despite the importance of physical exercise, the participation in and adherence to an exercise regimen by older adults is often low due to; a lack of time and motivation, boredom, a fear of falling, and/or environmental considerations such as inconvenience, accessibility, safety and/or cost (Valenzuela et al. 2018). To address this lack of participation and adherence, virtual rehabilitation is gaining in popularity (Valenzuela et al. 2018; Staiano and Flynn 2014).
Virtual reality (VR) is defined as an application that allows users to navigate through and interact with a completely virtual environment (Baus and Bouchard 2014). Meanwhile, augmented reality (AR) is described as a system which enhances the physical environment by overlaying virtual artefacts on the user’s perception of the real world (Baus and Bouchard 2014). Both VR and AR use virtual environments (VEs) which are accessible through immersive devices (Baus and Bouchard 2014) and can enable different forms of interaction through the capture of body pose and/or gesture (Baus and Bouchard 2014; Jerald 2015). A head-mounted display (HMD) (e.g., Oculus, Hololens, etc.) can be used to engage the user with a fully immersive audio-visual experience through movement detection (i.e. sensors, camera) and real-time visual, audio (and sometimes haptic) feedback (Jerald 2015). Less immersive experiences can be provided through the use of controllers (i.e. gaming controllers, Kinect camera, Wii balance board) and a screen (e.g. computer monitor, television screen, projection, etc.) displaying the environment in front of the user (Jerald 2015). Many interaction controllers can be used for the various levels of immersion including wearable inertial measurement unit (IMU) sensors [e.g. Xsens (Roetenberg et al. 2009)], body tracking cameras (e.g. Intel RealSense, Leap Motion, Kinect (Han et al. 2013)), and human pose detection libraries [e.g. OpenPose (Losilla and Rosique 2019)].
Virtual rehabilitation has been defined as the ability of virtual reality (VR) to provide therapy to patients using its hardware and simulation (Mubin et al. 2019). Exergames are games delivered through AR, VR or other forms of videogames and require the participants to be physically active (Song et al. 2011). Virtual rehabilitation and exergames allow various exercises mixing games and therapy, by enabling control (i.e., adaptation to the patients’ needs) and contact with the environment (i.e., real-time feedback) (Mubin et al. 2019). The potential of exergames for rehabilitation has been studied for older people from the viewpoint of physical and mental improvement (Staiano and Flynn 2014; Song et al. 2011).
To the best of our knowledge, there is no systematic review which explores and analyses existing technology-based approaches and exercises using virtual rehabilitation to support the physical rehabilitation of older adults and post-menopausal women with an emphasis on osteoporosis. As osteoporosis is a systemic skeletal disorder, this review addresses the following question; What is the most effective way to design virtual rehabilitation to obtain physical improvement (e.g. balance and gait) and support engagement (i.e. motivation) for people with musculoskeletal disorders?
2 Methodology
In this study, the authors followed the Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al. 2021). The PICO (patient/population, intervention, comparison, and outcomes) methodology was also used to define the research question. The term ‘older adults’ refers to people over 65 years old, and/or a vulnerable population when it comes to pharmacotherapy (Singh and Bajorek 2014).
2.1 Databases search
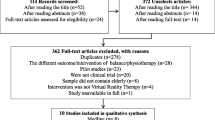
Given the clinical underpinnings of this review, we particularly focussed on the PubMed database, while also searching Google Scholar, and ACM. These three databases were searched between September and December 2021 (ET) and then validated by (AB, JJC, JD and MD) (Fig. 1). The following keywords and their combination were used: ‘Rehabilitation’, ‘AR’, ‘VR’, ‘Osteoporosis’, ‘Ageing’, ‘Therapy’, ‘Exercises’, ‘Fall Prevention’, ‘Human–Computer Interaction (HCI)’, ‘Task-oriented’, ‘Ankylosing spondylitis’, ‘Spinal Cord Injury’, ‘Balance’, ‘Muscular and Skeletal (MSK)’ and ‘Motion capture’. The inclusion criteria comprised: (a) content that focussed on physical exercise rehabilitation (e.g., balance, gait, muscle strength, flexibility); (b) VR/AR or exergames for therapy; (c) applicable to an older population; (d) accessible in open source; and (e) articles written in English or French. The exclusion criteria were: (a) studies not affecting physical rehabilitation; (b) content that focuses only on technology and not on therapy and (c) review or guideline content.
Flow chart of study's selection following PRISMA guidelines (Page et al. 2021)
All selected articles were published between 1986 and 2021. This period was selected as researchers started to explore the use of VR in non-entertainment settings (e.g. psychiatric treatment (Maples-Keller et al. 2017) in 1986.
Note: As there was a paucity of literature applying virtual rehabilitation to patients with osteoporosis, the authors broadened the search parameters to include articles relating to the virtual rehabilitation of other skeletal disorders (e.g., Ankylosing spondylitis, spinal cord injury, motor rehabilitation, etc.). These disorders were validated by this paper’s authors having a clinical background (JJC, BW) and are comparable to the physical therapy needs of patients with osteoporosis.
The selection process comprised (Fig. 1);
-
(i)
Identification: 130 articles (60% from PubMed, 26% from Google Scholar and 14% from ACM) were selected based on the keyword search and the inclusion and exclusion criteria. However, one article was excluded due to duplication reasons.
-
(ii)
Screening: In this stage, 24 articles were excluded due to access issues (i.e., not open-access and inaccessible by the authors’ institution).
-
(iii)
Eligibility: Of the remaining 105 (55% from PubMed, 28% from Google Scholar and 17% from ACM) articles, 59 were excluded based on details of the methods, studies and results; 25 were considered incompatible with this study for not focusing on the training or the design of the therapy or without any results, 22 were review articles, 10 were guidelines which focused on osteoporosis, 1 was rejected based on language issues, and 1 was excluded because it presented only an abstract (no full article). The remaining 46 articles were reviewed once more. 25 articles were excluded because they did not focus on physical training and older adults. This resulted in 21 articles (83% from PubMed, 13% from Google Scholar and 4% from ACM) being selected for this review.
3 Results
The 21 articles screened and included in this review cover a population total of 526 patients, aged between 18 and 88 years, 15 of the studies were exclusively related to older people and post-menopausal women while 7 focused on a mixture of younger and older populations. Note: The definition of older adults in this review is 65 years old and over (Singh and Bajorek 2014).
As outlined in the inclusion criteria, the selected articles do not focus exclusively on patients with osteoporosis but are extended to other care needs which also require physical rehabilitation, and/or training exercises. Hence the inclusion of eight different care needs in this study; fall prevention, general motor rehabilitation, spinal cord injury, post-stroke, shoulder abduction, ankylosing spondylitis, orthopaedic rehabilitation post-total knee arthroplasty (TKA) and Parkinson’s disease. Fall prevention and general motor rehabilitation are part of the useful training exercises for osteoporosis as they improve balance, gait, and/or motor abilities. Moreover, physical therapy for ankylosing spondylitis, spinal cord injury, post-stroke, shoulder abduction and orthopaedic rehabilitation post-total knee arthroplasty (TKA), is similar to that required for osteoporosis.
The studies included in this review have been categorised into the following groups; studies using a head-mounted display for virtual rehabilitation (see §3.1); studies using a Balance board (such as a Nintendo Wii Fit Plus) (see §3.2); studies using a camera for body recognition (see § 3.3) and studies using other examples of devices (e.g. data gloves) (see §3.4). In each group, the studies will be presented with the population, the setup, the design of the experiment and outcomes and results.
To avoid unnecessary duplication, we first define the measurement approaches prior to presenting them in the associated study results’ tables.
3.1 Group 1. use of a head-mounted display (HMD)
A summary of the study population and setup for Group 1 is shown in Table 1.
A summary of the interventions for each study in Group 1 is shown in the Table 2.
One study (Blomqvist et al. 2021) decided to keep the patients in one group (i.e. no control group). As the patients interacted with the virtual environment, they were required to track and catch an object. The training sessions had increasing levels of difficulty. Two studies (Yoo et al. 2013; Jung et al. 2012) separated the patients into two study groups. Yoo et al. (2013) developed Otago exercises using AR, while Jung et al. (2012) employed a VR treadmill exercise. Meanwhile, the control groups for both studies performed similar exercises to the intervention groups using conventional methods. The Otago exercise programme was developed by the New Zealand fall prevention research group to reduce falls in older adults (over 65 years of age) (Gardner et al. 2001). It consists of 17 strength and balance exercises and a walking progressive-resistance program (Yoo et al. 2013; Lee et al. 2017; Gardner et al. 2001). This program also includes five strengthening exercises (knee extensor, knee flexor, hip adductor, ankle plantar-flexors (calf raises) and ankle dorsiflexors (toe raises) and 12 balance exercises (knee bend, backwards walking, walking, and turning around, sideway walking, tandem stance (heel-toe stand), tandem walk (heel-toe walk), one leg stand, heel walking, toe walk, heel-toe walking backwards, sit to stand, stair walking) described in Gardner et al. (2001). The AR-Otago exercises used in Yoo et al. (2013) focussed on muscle strengthening and balance training. The VR treadmill exercise in Jung et al. (2012) comprised a conventional treadmill training without control over the slope for the control group and a walk-in-a-park stroll for the intervention group. Lee et al. (2017) separated their patients into three groups: one intervention group (AR-Otago) and two control groups (Yoga exercises and self-Otago). The AR-based group (with technology) and the self-Otago group practiced exercises focussing on knee flexion, walking in different conditions, and standing up. Yoga exercises were also proposed for the third group i.e. seven distinct positions proposed without the use of technology.
The four studies in this group used a combination of the following measurement approaches:
-
Falls Efficacy Scale-International (FES-I): is a 16-items scale used to measure the confidence of the patient in performing daily activities without falling (Delbaere et al. 2010). An FES-I score ranges between 16 and 64 (where a high score indicates low confidence and a high risk of falling) (Delbaere et al. 2010).
-
Falls Efficacy Scale Swedish Version (FES-SV): is a slight variation of the FES-I, adapted for the Swedish language.
-
Morse Fall Scale (MFS): is a scale to assess a patient's likelihood of falling based on their medical history (i.e. their history of falling, previous diagnoses, ambulatory aid needs, gait state and mental state) (Morse et al. 1989). An MFS score ranges between 0 and 125. The patient is considered at minimal risk for any score under 25, at moderate risk when the score is between 25 and 45, and at high risk of falling when the MFS score is greater than 45 (Morse et al. 1989).
-
Activity-Specific Balance Confidence (ABC): is a 16-item structured questionnaire used to measure an individual's confidence in performing daily activities without losing balance (Wildschut et al. 2020). The scores range from 0 to 100%. The patient is considered to have a high level of physical functioning for any score over 80%, a moderate physical functioning when the score is between 50 and 80%, and a low level of physical functioning when the ABC score is under 50%.
-
Force Platform: first measures the force exerted by the body on the ground and then determines the centre of pressure, the centre of gravity and the balance (Browne and O’Hare 2000). Force Plate and Ergopower Platform are similar in functionality to a Force Platform.
-
Berg Balance Scale (BBS): is a 14-item scale used to objectively determine the patient's ability to safely balance during a series of pre-determined tasks (Berg et al. 1989). The patient is considered at great risk of falling when the BBS score is under 45; they are considered to have a functional balance when the BBS score is greater than 56.
-
Short Physical Performance Battery (SPPB): is a series of time-recorded exercises [such as sit and stand and balance testing with the feet in a certain position (i.e. feet together, semi-tandem, full-tandem)] used to evaluate lower extremity function and mobility in older people (Gómez et al. 2013).
-
Time Up and Go (TUG): is a test to determine fall risk and measure a person’s balance. The TUG test consists of a sit-to-stand and walking exercise. An older adult who takes more than 12 seconds to complete the TUG test is considered at risk of falling (Kear et al. 2017)
-
Gait Rite system: is a three meters walkway used to measure spatio-temporal parameters (i.e. gait, velocity, cadence, step length and stride length) (Yoo et al. 2013; McDonough et al. 2001).
-
Raptor 4S (optical camera): detects and analyses body movements (Topley and Richards 2020).
-
Manual muscle test: is an important evaluating tool to assess impairments and deficits (including strength, power, and endurance) in muscle performance (Robertson 1984). By working against gravity or against an opposing manual resistance, the Manual Musce test evaluates the patient’s available range of motion. A score of 5 indicates that the patient’s muscle performance is considered to be of normal strength while a score of 0 indicates no strength (Robertson 1984).
-
Maximum voluntary contraction test: is a measures muscle strength using EMG electrode data (Boettcher et al 2008).
The feedback from the patients and physiotherapists regarding the interventions is presented in Table 3.
70% of the patients from Blomqvist et al. (2021) mentioned that the feedback provided during the training was positive and could help to motivate them to train more. However, the remainder of the patients felt that the feedback could be clearer and/or that the audio feedback did not always match the situation (Blomqvist et al. 2021). Each of the four studies concluded that the virtual therapy was not only feasible (Blomqvist et al. 2021) but provided opportunities to improve balance (Yoo et al. 2013), gait (Yoo et al. 2013), fall efficacy (Yoo et al. 2013), strength (Jung et al. 2012) and/or symmetry (Jung et al. 2012) while increasing engagement for the physical therapy with meaningful exercise (Blomqvist et al. 2021; Yoo et al. 2013; Jung et al. 2012; Lee et al. 2017).
3.2 Group 2. use of a balance board
Balance boards such as the Nintendo Wii Fit plus are often used in exergames for patient rehabilitation (Yen et al. 2011; Wall et al. 2015; Van den Heuvel et al. 2014). Six selected articles utilized a balance board for their study (Table 4).
All studies required a screen to display the training. The Wii balance board is a game controller for the Nintendo Wii system, released in 2007, and has been employed in clinical rehabilitation settings worldwide (Bartlett et al. 2014). The Wii balance board contains similar components to a typical force platform (Bartlett et al. 2014). A summary of the interventions for each study is shown in Table 5.
All studies, excluding (Wall et al. 2015) used a control group. During one-hour sessions, the patients played multiple commercial games from Nintendo Wii Fit Plus Aerobic exercises (i.e. Basic Run) and Balance games (i.e. Penguin plunge, Segway Circuit, island Cycling, rolling down the river, tightrope walk, obstacle course, ski jump, ski slalom and tilt table).
The six studies used a combination of the following measurement approaches:
-
Force platform: explained in 3.1.
-
Functional Reach Test (FRT): is a single item test developed for balance problems for older adults. In this test, the patients stand upright and are then instructed to reach forward along a yardstick without moving their feet. The maximum distance is then measured by the physiotherapist. A patient with a score of six or less is considered to have a significant increased risk for falling (Duncan et al. 1990).
-
Sensory Organization Test (SOT): is a form of computerized dynamic posturography designed to make a quantitative assessment of sensory integrative ability among the three main sensory systems (Szturm et al. 2011). During this test, the patient stands on a dual-force platform plate in a three-sided surround, with the anterior–posterior being recorded. The SOT test is usually made in three independent sensory conditions (i.e. on firm surface, with a sway referenced visual surround and with a sway referenced support surface) with eyes opened and eyes closed (Szturm et al. 2011; Yen et al. 2011). The outcome of the SOT is the equilibrium score (i.e. the average of the centre of gravity for each try), the composite equilibrium (i.e. a weighted average of the six conditions), the sensory analysis ratio (i.e. the computed averages to identify impairments of individual sensory systems), the centre of gravity, and the strategy analysis (i.e. hip and ankles strategy analysis) (Szturm et al. 2011).
-
Verbal Reaction Time (VRT): is the delay between the time when the patient sees the instructions and verbally explaining what they are doing (Yen et al. 2011).
-
BBS: explained in 3.1.
-
Time Up and Go Test (TUG): explained in 3.1.
-
Gait Rite Platform: explained in 3.1.
-
Activities-Specific Balance Confidence Scale (ABC): explained in 3.1.
-
Romberg Test: is a tool to diagnose sensory ataxia, and gait disturbance (Khasnis and Gokula 2003). For this test, the patient must stand upright with their eyes closed. A loss of balance (LOB) is interpreted as a positive Romberg sign (Khasnis and Gokula 2003).
-
10 Meter Walk Test (10MWT): is a test where the patient is asked to walk a short distance (between six and twelve meters) after which their speed result is compared against a table or normative value (average walking speed for men and women by age class) (Chan and Pin 2019).
-
Six minutes’ walk test (6MWT): is a test measuring the maximum walking distant of the patient in six minutes (Enright 2003).
-
WISCI II: is a tool to measure improvements in walking ability for spinal cord injury. The therapist observes the patient walking and gives a score out of 20 (Dittuno and Dittuno 2001).
-
Rand 36-Items Short Form Survey (RAND SF-36): is a self-reporting questionnaire composed of a set of generic, coherent, and easy quality of life measurements (Hays and Morales 2009).
-
Single Leg Stance test: In this test, the patient must stand unassisted on one leg, timed from the time the other foot leaves the ground until the moment the foot touches the ground again or the arms leave the hip (Omaña et al. 2021). If the time result is less than five seconds, the patient has a greater risk of injury from fall (Omaña et al. 2021).
-
FES: explained in 3.1.
-
Hoehn and Yahr scale: is a scale to evaluate the functional disability associated with Parkinson's disease (i.e. describing the disease through its various stages) and to highlight the severity of the case. The resulting stages are between one (unilateral involvement with minimal or no functional disability) and five (confinement to bed or wheelchair unless aided) (Goetz et al. 2004).
-
Unified Parkinson Disease Rating Scale (UPDRS): is a rating tool to gauge the severity and progression of Parkinson's disease in patients. It is separated in four parts: intellectual function, mood and behaviour, activity of daily living and motor examination & motor complication (Hauser et al. 2012; Perlmutter 2009). The UPDRS result can be between one and four with a higher score showing increased severity of the disease (Perlmutter 2009).
-
Parkinson’s Disease Questionnaire (PDQ39): is a 39-item questionnaire where a patient self-reports their health status and quality of life (Hagell and Nygren 2007). Essentially, this test assesses how often people with Parkinson's disease experience difficulties across eight dimensions of daily living (including relationships, social situations, and communication etc.). The lower the score, the better the quality of life (Hagell and Nygren 2007)
-
Hospital Anxiety and Depression (HAD) scale: is a self-assessment of depression and anxiety (Zigmond and Snaith 1983; Roberts et al. 2014). A score between 0 and 7 is considered normal; a score of 8–10: is considered borderline abnormal (borderline case) while 11–21 is regarded as being abnormal (case) (Zigmond and Snaith 1983).
-
Multidimensional Fatigue Inventory (MFI): is a 20-item scale to evaluate five dimensions of fatigue (i.e., general fatigue, physical fatigue, reduced motivation, reduced activity, and mental fatigue) with a total fatigue score between 20 and 100. A high score indicates a high level of fatigue for the patient (Dencker et al. 2015; Shahid et al. 2012).
An analysis of the studies’ results showed that although the FRT score improved in (Van den Heuvel et al. 2014; Wall et al. 2015; Lee et al. 2015) for both the experimental and the control group, there was a greater improvement for the experimental group. Cho et al. (2014) obtained significant balance improvement for both groups and greater overall improvements for the experimental group. Wall et al. (2015) declared no change in the TUG score after the training. This could be explained by the choice of exercises used during the training. The TUG test measures mobility, a complex task requiring many skills, however the Nintendo Wii fit alone doesn’t train many of the mobility skills. Wall et al. (2015) concluded that a lack of activity specificity (i.e. turn, sit-to-stand) within the training was one of the barriers to improving mobility, and by association, the patients’ TUG score. Yen et al. (2011) concluded that the experimental and conventional balance training group obtained better results than the control group (without training) under SOT-5 (unreliable somatosensation with eyes closed). Additionally, the experimental training group (with the technology) significantly improved under SOT-6 (unreliable vision and somatosensation) compared to the conventional training group. The improvement in equilibrium under one somatosensory condition for the experimental and the conventional balance training groups suggests that both groups achieved similar results. Moreover, the non-significant difference between these two groups in the SOT analysis can be related to their similar treatment principles (monitoring visual, somatosensory, and vestibular information during training), a short training duration and a small sample size. In addition, the conventional balance training group also had increases in the vestibular sensory ratio after the training, with no significant effect being recorded for the experimental training.
While the gait analysis performed by Wall et al. (2015) and Van den Heuvel et al. (2014) showed a significant increase in speed, there was no significant correlation between the intervention and its duration on gait and speed. Wall et al. (2015) did not find any significant correlation between and within the groups on the average walking speed and on spatio-temporal gait parameters. Table 6 shows the results of these interventions.
The Verbal Reaction Time (VRT) was analysed by Yen et al. (2011) but no significant result was found. The VRT was not reduced during postural control, which can be explained by the fact that the maximum resource capacity of a patient (i.e. the time when their brain is getting overloaded with information) was not reached during the training.
The improvement in RAND-SF36 results for Wall et al. (2015) was not significant. The explanation is that while RAND-SF36 addresses overall health, it may not capture minor changes in mobility.
Five of the studies determined that the experimental training was useful, feasible and positive for the patients (Yen et al. 2011; Szturm et al. 2011; Cho et al. 2014; Wall et al. 2015; Van den Heuvel et al 2014). Yen et al. (2011) concluded that the task-oriented training significantly improved dynamic balance. They also found that both the experimental and conventional balance therapies were useful and effective. This is supported by Cho et al. (2014) with the feasibility of coupled graded dynamic balance exercises on different surfaces with video-game tasks.
Three studies (Cho et al. 2014; Van den Heuvel et al. 2014; and Lee et al. 2015) also concluded that the results from the experimental training did not surpass those from conventional training. Because of the limitations of the studies (i.e. short duration, small sample), it is difficult to generalize. However, the experimental training was not worse than the conventional training because of benefits such as: low cost, accessibility and increase of patient motivation (Szturm et al. 2011; Cho et al. 2014; Wall et al. 2015).
3.3 Group 3. Use of a camera and a screen
Motion detection cameras (i.e. Kinect, IREX, Sony Eye Toy, VRRS and web-camera) provide opportunities for the user to be immersed in the virtual environment unconstrained by a physical device (i.e. no controllers, no glasses to wear, etc.). The Kinect is an RGB-D sensor, initially used as an input device by Microsoft for the Xbox game console (Han et al. 2013). It captures synchronized colour and depth images with an infrared projector and an infrared camera. Studies have shown a satisfactory performance by the Kinect’s skeletal tracking algorithm in posture recognition (Han et al. 2013). However, the detection of body joints is not always completely reliable, especially for cluttered and occluded scenes (Han et al. 2013). The immersive rehabilitation exercise (IREX) system from GestureTek is composed of: a body recognition camera, red gloves, a green screen, a background mat, and a television screen (An and Park 2018). The IREX system places the live real time full body image of the patient onto the screen where they can then see themselves immersed in dynamic virtual reality video games (An and Park 2018). This system is suitable for rehabilitation and balance training (i.e. more natural, and intuitive movement, adaptable to the patients, their needs and abilities, flexibility) (An and Park 2018; Kizony et al. 2005). The Sony Eye Toy is a game-oriented motion tracking sensor for the PlayStation 2 and provides an opportunity to interact with virtual objects (Rand et al. 2008). This system displays the real-time image of the user, so that they can see themselves manipulating virtual objects within a virtual environment superimposed on an image of the actual physical surrounding (Rand et al. 2008). The Virtual Reality Rehabilitation System (VRRS) is a commercial medical device for rehabilitation and tele-rehabilitation (Gianola et al. 2020). Table 7 presents the studies and their population.
Three studies included a mix of young, middle aged and older adults (Gianola et al. 2020; Trombetta et al. 2017; Da Gama et al. 2016). Aung and Al-Jumaily et al. (2011) did not provide information regarding the age of the study’s population. Note: we included three studies which did not reference older adults, (Khurana et al. 2017; An and Park 2018; Kizony et al. 2005). Based on advice from experts in Rheumatology, these studies can be adapted for older patients with osteoporosis. Overall, the ten studies in this group focussed on eight different care needs [i.e. post-stroke rehabilitation (Trombetta et al 2017; Khurana et al. 2017), shoulder abduction (Da Gama et al. 2016), general motor rehabilitation (Aung and Al-Jumaily 2011; Im et al. 2015), orthopaedic rehabilitation post TKA (Gianola et al. 2020), spinal cord injury (An and Park 2018; Andreikanich et al. 2019; Kizony et al. 2005), and ankylosing spondylitis (Kaharan et al. 2016)]. All ten studies required the patient to perform a specific movement to play the game and receive audio and/or visual feedback on their movements. Each study, excluding (Gianola et al. 2020) required a screen and provided real-time feedback to the patients (audio and/or visual).
Seven studies did not mention the existence of a control group (An and Park 2018; Khurana et al. 2017; Aung and Al-Jumaily 2011; Kaharan et al. 2016; Andreikanich et al. 2019; Im et al. 2015; Da Gama et al. 2016). A summary of the interventions for each study is shown in Table 8.
A combination of the following measurement approaches were used:
-
BBS: explained in 3.1.
-
ABC: explained in 3.1.
-
TUG: explained in 3.1.
-
Force platform: explained in 3.1.
-
FRT: explained in 3.2.
-
WISCI-II: explained in 3.2.
-
Limit of stability (LOS): challenges patients to move and control their centre of gravity within their base of support. LOS use eight targets (forward, backward, right, left, forward-right, forward-left, backward-right and backward left), randomly highlighted, that the patient must reach by weight shifting (An and Park 2018).
-
FRT modified version (used by Kizony et al. 2005): seven scores are measured and calculated for each patient. For FRT1, the patient stands with the right side of their body near a wall. They are asked to raise their right arm to 90° shoulder flexion, with their elbow fully extended, and to lean forward as far as possible. FRT2 is the same exercise but with the left side of the body adjacent to the wall and with the left arm reaching as far as possible. FRT3 is calculated by the sum of FRT1 and FRT2. For FRT4, the patient faces a wall and is asked to reach with their right arm as far as possible to the right. FRT5 is the same as FRT4 but with the left arm to the left. The sixth assessment (FRT6) is in the same position (facing a wall) and the patient is asked to maximally reach with their dominant arm (left or right) to the highest point possible on the wall in front of them. Finally, FRT7 is calculated by the sum of FRT4, FRT5 and FRT6.
-
Active knee Range of Motion (ROM): represents how much the knee can bend and straighten on its own (no external force for the active method) (Gianola et al. 2020; Sharma et al. 2021).
-
Isometric strength: measures the ability of the patient to hold a sustained contraction against a resistance for a specific duration. It is assessed with a dynamometer (Gianola et al. 2020; Sharma et al. 2021).
-
Frequency of medication: measures the need of medication pre-, post-, and during the training (Gianola et al. 2020).
-
Visual Analog Scale (VAS): is a pain intensity uni-dimensional Likert-like rating scale (Gianola et al. 2020; Kaharan et al. 2016; Weigl and Forstner 2020).
-
Maximum joint angle: represents the distance between the joints represents the maximum angle of the shoulders (Im et al. 2015).
-
Number of repetitions: represents how many repetitions the patient can realise without rest (Da Game et al. 2016).
-
Response time: is the duration between the moment when the patient is aware of the action and the start of their movement (Kizony et al. 2005; Im et al. 2015).
-
Success rate: is the percentage of success corresponding to the number of correct movements during the training (Da Gama et al. 2016; Kizony et al. 2005; Im et al. 2015).
-
Pittsburgh rehabilitation participation scale (PRPS): is a one item scale designed to assess a patient's participation in therapy using a six-point Likert scale reflecting the therapist’s observation of patient participation (from 0 (None) to 6 (Excellent)) (Im et al. 2015; Lenze et al. 2004).
-
Interview: is carried out to understand the patient’s view of the virtual therapy (fun, motivation, therapeutic value) and their opinion of the system (interface, augmented reality characteristics) (Trombetta et al. 2017; Andreikanich et al. 2019; Kizony et al. 2005; Da Gama et al. 2016).
-
Euro-Quality of life five-dimension (EQ-5D): is a standardised measure of health to determine the evolution of patient health and quality of life through five dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) (Gianola et al. 2020; Rabin and Charro 2009).
-
Global Perceived Effect (GPE): is a scale where the patient numerically rates how much their condition has improved or deteriorated since a predefined time point (Kamper et al. 2010).
-
Functional independence measure (FIM): is an 18-items instrument to measure a disability (including measures of independence for self-care, locomotion, communication, and social recognition) on seven levels (a higher score indicates greater independence) (Gianola et al. 2020; Kizony et al. 2005).
-
Ankylosing spondylitis quality of life (ASQOL): is an 18-items rating scale used to assess the health related quality of life for patients with ankylosing spondylitis. A high score on this scale indicates a poor quality of life (Kaharan et al. 2016; Doward et al. 2007).
-
Bath ankylosing spondylitis disease activity index (BASDAI): is a 6-items rating scale from one (no problem) to ten (worst problem) related to fatigue, spinal pain, joint pain/swelling/areas of localized tenderness, morning stiffness duration and stiffness severity (Kaharan et al. 2016).
-
Bath ankylosing spondylitis functional index (BASFI): is an instrument to assess the degree of functional limitation in patients with ankylosing spondylitis (Calin et al. 1994; Kaharan et al. 2016)).
-
Spinal cord independence measure III (SCIM): is a scale of daily functioning assessment of patients with spinal cord lesion. The SCIM III contains 19 tasks divided in three sub-scales (self-scare, respiration/sphincter management, and mobility) on which the therapist will give a score corresponding to what the patient can achieve (Itzkovitch et al. 2018; Boswell-Ruys et al. 2009).
-
T-shirt test: is a time measurement of duration to put on and take off a t-shirt (Khurana et al. 2017).
-
Western Ontario and McMaster universities arthritis index (WOMAC): is a self-administered questionnaire consisting of 24 items divided into three sub-scales (pain, stiffness, physical function) and evaluating the hip and knee osteoarthritis. A high score on any of the sub-scales indicates worsening pain, stiffness, and/or functional limitations for the patient (Roos et al. 2009).
Six studies measured the patients’ progress in balance (An and Park 2018; Khurana et al. 2017; Da Gama et al. 2016; Im et al. 2015; Gianola et al. 2020; Kizony et al. 2005). Improvements in the BBS score and the lowest time for the TUG were noticed by An and Park (2018) and Im et al. (2015). The decrease of the TUG time could lead to an increase in standing balance and upright mobility. An and Park (2018) also obtained a significant increase of the overall loss of stability (LOS) score. The forward and backward LOS did not differ significantly, but the directional LOS did. The improvement of the overall and directional LOS means that the adjustment ability improved in the frontal plane due to the weight shifting provided by the training (An and Park 2018).
The patients’ success rate in the game improved for Im et al. (2015), Da Gama et al. (2016) and Kizony et al. (2005), which suggests that the game helped the users to learn the movements and to repeat them correctly (i.e., Da Game et al. 2016). Note:The experimental group usually had 70% more correct results compared to 0% for the control group. The improvement in performance resulted in an increase in the average number of repetitions during the training in the study by Kizony et al. (2005). In the most optimistic scenario, a patient was able to engage in 100 more repetitions while using the system (Da Game et al. 2016). Kizony et al. (2005) used the performance score to conclude that the 'Snowboard' game was the easiest (with the highest score in both groups) while the 'Soccer' game was the most difficult (with the lowest score for both groups but mostly for the patients with spinal cord injury).
A significant increase of the PRPS score to the maximum for every participant was noticed by Im et al. (2015). In four studies (Andreikanich et al. 2019; Trombetta et al. 2017; Kizony et al. 2005; De Gama et al. 2016), the majority of the patients reported interest and an improvement in their motivation for the therapy. However, patients reported feeling some physical and mental discomfort (Kizony et al. 2005) (i.e. fatigue. injury-related pain, embarrassment, lack of realism, eye-hand coordination).
Significant improvements for spinal cord injury of the WISCI II, tee-shirt test (change associated with the group effect) and SCIM III (change associated with time) were observed by Khurana et al. (2017) and An and Park (2018). The WOMAC test used by Gianola et al. (2020) showed a similar pattern between the experimental and control groups. This could be due to the lack of manual treatment in virtual reality.
Five of the studies concluded that virtual rehabilitation was safe, convenient, and more engaging than conventional training (An and Park 2018; Aung and Al-Jumaily 2011; Gianola et al. 2020; Kizony et al. 2005; Da Gama et al. 2016) obtained better outcomes (i.e. balance, fall prevention, spinal cord injury stage assessment) in the experimental group which might be due to the dynamic nature of the moving virtual stimuli. Three studies (Aung and Al-Jumaily 2011; Gianola et al. 2020; Trombetta et al. 2017), considered virtual rehabilitation an efficient, economical, and convenient alternative solution to traditional face-to-face therapy, particularly if the patients accept the technology. Moreover, Gianola et al. (2020) stated that the technology has the advantage of reducing the number of in-person sessions performed in rehabilitation centres. The ability to help in both learning and performing the movements correctly was highlighted by Da Gama et al. (2016) as an important characteristic of an unsupervised situation.
However, improvements can still be made. Da Gama et al. (2016) noted that the entertainment criteria was not consolidated because of the simplicity of the game. In the study of Andreikanich et al. (2019), the doctors and therapists involved in the study proposed some improvements (i.e. progressing skills levels, hand gesture control, adaptability, use of a seat wheel-chaired patients to protect them from falls). Gianola et al. (2020) declared that virtual reality-based training is not superior to tradition rehabilitation in relieving pain and improving other function outcomes. Gianola et al. (2020) concluded that the correlation between VAS and gender could have influenced the result. 60% of the studies reported limitations such as the sample size (An and Park 2018; Kizony et al. 2005), the use of old/cheap technology (Im et al. 2015), the lack of standard exercises and objective muscle power and balance measurement in the follow-up (Karahan et al. 2016) and the use of only healthy patients (Aung and Al-Jumaily 2011).
3.4 Group 4. Other devices
Devices such the CyberTouch Dataglove or the Youkicker rehabilitation system, which focus on a specific part of the body can also be used for exergames. The Youkicker is a VR lower limb rehabilitation system which presents a virtual representation of the feet and the legs in the first-person perspective (Villiger et al. 2017). The CyberTouch dataglove is a tactile feedback instrumented glove (Dimbwadyo-Terrer et al. 2016). Both devices require the use of a screen. Villiger et al. (2017) used the Youkicker to focus on ankle and foot movements whilst Dimbwadyo-Terrer et al. (2016) used the CyberTouch Dataglove and focussed on the movements of the hands and fingers (Table 9).
The size of the population for the two selected articles varied between nine and 12. The age of the total population ranged between 41 and 74 years. These two articles focussed on only one care need: Spinal Cord Injury (Villiger et al. 2017; Dimbwadyo-Terrer et al. 2016) (Table 10).
A combination of the following measurement approaches was used:
-
SCIM III: explained in 3.3.
-
WISCI II: explained in 3.2.
-
Manual muscle test: explained in 3.4.
-
Lower Extremity Motor Score (LEMS): is a scale between zero (complete paralysis) and fifty (normal strength), using the ASIA key muscle in bother lower extremities.
-
10 m walk test (10MWT): explained in 3.2.
-
Six minutes’ walk test (6MWT): explained in 3.2.
-
Berg Balance Scale (BBS): explained in 3.1.
-
Time Up and Go (TUG): explained in 3.1.
-
Scale Barthel (BI): is an ordinal scale to measure independence and mobility in ten daily life activities (Mahoney and Barthel 1965) (i.e. bowel control, bladder control, grooming, toilet use, feeding, transfer, mobility, dressing stairs, bathing). The time taken and the physical assistance required to perform each activity are used to assign the value of each item. The higher the score, the greater the patient is able to function independently.
-
Patients' Global Impression of Change (PGIC): is a self-reported scale reflecting a patient's belief about the efficacy of a treatment on a 7-item scale (from 'very much improved' to 'very much worse') (Scheman and Ferguson 2009).
-
Duration: is a measurement of the time to complete each task to evaluate the speed of the patient and their performance during the training.
-
Interview: captures the patients‘ opinion on the training (most challenging games, most attractive games, user experiment).
-
Jebsen Taylor Hand Test (JTHFT): is a standardised test composed of seven subsets to evaluate the fine and gross motor hand function (i.e. writing, simulated page turning, lifting small objects, simulated feeding, stacking, and lifting large, lightweight, and heavy object) (Fabbri et al. 2021).
-
Nine Hole Peg Test (NPHT): is a test administered by asking a patient to take pegs one by one from a container and then place them into holes on a board as quickly as possible, after which they have to put them back in the container (Wang et al. 2015). The score is based on the time to complete the task (Wang et al. 2015).
A significant improvement in balance and in dorsiflexion was obtained by Villiger et al. (2017). Meanwhile, Dimbwadyo-Terrer et al. (2016) reported improvements in dexterity with a lower time for the experimental group and an increase in time for the control group in the NPHT. This may be explained by the fact that 66% of the patients completed the third session in a shorter time. Hence, the learning of the movements might then have been transferred to real objects. Villiger et al. (2017) also recorded an increase in the patients’ motivation after the training. The patients evaluated the system positively (user-friendliness, visual approach). Patients indicated that they would like to continue to use the system. However, the 10MWT and 6MWT tests showed that the effect on gait was not significant. Some mobility characteristics of the 6MWT were perhaps partially assessed by the TUG, but no significant result was measured in the experimental group. The effect of the experimental training for the spinal cord injury was not significant for either the control or intervention groups (Villiger et al. 2017) while there was a more favourable result for the experimental group in Dimbwadyo-Terrer et al. (2016). This indicates that the dataglove and the exercises were more adapted to the spinal cord condition. The two studies concluded that significant improvements in lower limb, balance and functionality showed the feasibility of the training (Villiger et al. 2017; Dimbwadyo-Terrer et al. 2016). Moreover, despite the fact that the motivation after training was higher, the training programme needed to be more engaging. Dimbwadyo-Terrer et al. (2016) also concluded that it could be possible to have training based on functional reaching movements in a virtual environment (Tables 11, 12).
4 Discussion
There is no previous systematic review which explores and analyses existing technology-based approaches and exercises using virtual rehabilitation to support the physical rehabilitation of older adults and post-menopausal women with an emphasis on osteoporosis. Hence, this literature review seeks to identify effective ways to design virtual rehabilitation to obtain physical improvement (e.g. balance and gait) and support engagement (i.e. motivation) for people with skeletal disorders. In our review, we examined: the impact of four types of technology (i.e. HMD, balance board, camera, and more specific devices), the intervention method/s (i.e. exercises), and the measurement approaches with respect to physical improvement (i.e. balance, gait, muscle strength, body movement, dexterity, hand function, care-oriented) and the support of engagement, post-intervention.
Nine studies (Blomqvist et al. 2021; Yoo et al. 2013; Jung et al. 2012; Lee et al. 2017; An and Park 2018; Khurana et al. 2017; Da Gama et al. 2016; Gianola et al. 2020; Villiger et al. 2017) achieved significant overall improvements in balance and fall prevention through the use of an HMD, a body tracking camera or the YouKicker. While overall improvements in balance were also achieved with the balance board, the results were not significant for all studies in this review (i.e. significant results were achieved for Yen et al. (2011) whilst there were insignificant results for Van den Heuvel et al. (2014)), due to the limited mobility of the balance board. Wall et al. (2015) reported that as the balance board did not significantly improve mobility factors (e.g. gait) which are important for balance, there was a resultant lack of improvement in the TUG and other mobility tests. Wall et al. (2015) concluded that due to the limitation of the exercise design, balance improved only in the directional score.
With regard to gait improvement, the experimental groups using an HMD obtained significant improvement, whilst the group using a camera or alternative device (e.g. Youkicker) did not notice a significant effect of the training.
Villiger et al. (2017) noticed that not every patient was able to participate in the 10MWT and 6MWT. Training with an HMD, a Youkicker or a Dataglove appeared to achieve better results in terms of improving muscle strength. Lee et al. (2017) obtained a similar improvement for both experimental and control groups, which means that the improvement came from the exercise and not from the virtual intervention. Specific devices, such as the dataglove and/or Youkicker allowed more detailed work on one part of the body which may explain these results.
Training with an HMD or with a body tracking camera positively impacted overall body movement. Significant improvements in dexterity and hand functioning were found with the use of dataglove in exergames (Dimbwadyo-Terrer et al. 2016). This shows that in targeting specific physical improvements or overall bodily improvements, the choice of device and the precise definition of the training is critical. As an example, the datagloves and the Youkicker only improved a specific part of the body. Meanwhile, a balance board improved some (e.g. postural control, gait) but not all mobility characteristics. While an HMD or a body tracking camera can have a positive impact on full body training, they do not target specific areas. Ultimately, the type of training and its design are more important than the technology in order to have a bigger impact on the patient.
This review also identifies the most ‘effective’ approach to virtual training design in order to achieve physical improvement and support engagement. Effective virtual training design in this context refers to the design of virtual therapy which significantly improves the targeted areas while engaging the patient with their therapy. The user experience and opinion of both the patients and the therapists of the training has been analysed for interventions using HMDs, a camera, or specific devices. Blomqvist et al. (2021) obtained positive feedback on: the duration of the game and the fixed schedule, the entertainment in one of the training programmes, the helpful feedback in the game and the advantages of the technology (e.g. convenient, safe, easy, fun, cost effective and home-based practice capability). Negative feedback was also recorded with respect to training programme design (e.g. difficulty) and technology choice in relation to: device weight, poor fit and difficulty in calibration. Blomqvist et al. (2021) concluded that a fixed schedule may not suit everyone. They also suggested that short, patient adapted exercises can be more applicable to daily life while mitigating against boredom and pain.
The physiotherapists from these studies proposed solutions to avoid user pain and difficulty in games: wearing protective padding between the nose and headset (Blomqvist et al. 2021), providing clear instructions (Blomqvist et al. 2021; Andreikanich et al. 2019) and ensuring that the patients are also able to play the exergames in a seated position (Andreikanich et al. 2019). Universally positive feedback for exergames using cameras was recorded from the context of: entertainment (Aung and Al-Junaily 2011; Andreikanich et al. 2019; Kizony et al. 2005) and the ability to play from home (Kizony et al. 2005).
AR and VR applications for older adults typically target cognitive and physical rehabilitation, treatment of mental diseases etc. As there is a paucity of literature applying virtual rehabilitation to older patients with osteoporosis, our systematic review resulted in the following conclusions for this vulnerable population;
The results presented thematically are:
-
(1)
Virtual Therapy
virtual therapy was not only feasible but provided opportunities to improve balance, gait, fall, strength and/or symmetry while increasing engagement for the physical therapy with meaningful exercise.
-
(2)
HDM
Positive feedback provided during the training helps to motivate participants to train more.
-
(3)
Balance board:
-
(4)
Improvement in FRT score, overall balance, no change in the TUG score.
-
(5)
Better improvements in SOT-5 and SOT-6 compared to traditional training.
-
(6)
Significant improvement in Gait analysis.
-
(7)
Body tracking camera:
-
(8)
Improvements in the BBS score and the TUG test.
-
(9)
Significant increase of the overall loss of stability (LOS) score.
-
(10)
A significant increase of the PRPS score to the maximum.
-
(11)
This technology enhanced the participants’ motivation for the therapy.
-
(12)
Overall design
-
(13)
Need for activity specificity (i.e. turn, sit-to-stand) within the training to improve mobility.
-
(14)
Need to include task-oriented training as this significantly improves dynamic balance.
-
(15)
The inclusion of coupled graded dynamic balance exercises on different surfaces with video-game tasks enhances engagement and improves performance.
-
(16)
The use of games embedded within the virtual training supports the users in learning the movements and repeating them correctly.
Therefore, in conclusion, when deciding to use virtual training for older adults with osteoporosis, the main recommendations (based on the above) include:
-
The technology choice (i.e. HMD, body tracking camera, specific devices, balance board) must be related to the care need (i.e. improvement required, patient’s needs).
-
While balance boards can be used for overall body improvement, they do not significantly improve mobility factors such as gait.
-
When using the balance board, it is necessary to design games/exercises which train balance in multiple directions.
-
The use of HMDs, a body tracking camera or the YouKicker can support balance improvement.
-
HMDs support gait improvement more so than the use of a camera or YouKicker.
-
The use of a Dataglove, Youkicker and/or HMD has the potential to significantly improve muscle strength. The Dataglove has the greatest impact on muscle strength, followed by the Youkicker and an HMD.
-
The use of an HMD or body tracking camera can positively impact overall body movement.
-
Datagloves can lead to improvements in manual dexterity and hand functioning.
-
An HMD or a body tracking camera can result in positive impacts on full body training.
-
An HMD or a body tracking camera cannot be used to track specific areas e.g. hand mobility.
-
The type of training and its design are more important than the technology selected.
-
The training schedule should be personalised to support/enhance engagement.
-
Short (i.e. between 15 and 30 min) and frequent (i.e. 2–3 times per week) training programmes can mitigate against boredom and pain.
-
When using an HMD, provide protective padding between the nose and headset.
-
Cameras, balance boards and specific device are often more comfortable for use during the training programme.
-
Provide clear instructions on what is required in the exergames whilst also stating the expected learning outcomes.
-
Design the exergames so that the patients can also train in a seated position.
-
The design characteristics preferred by patients include: user-friendly interaction, clear instructions and feedback, a comfortable interface and the opportunity for personalization.
-
The comfort and immersion of the patient has an impact on the outcome of the training sessions. Note: HMDs are the most immersive technology.
In conclusion, the choice of the technology and the design of the exergames are key items to improving virtual rehabilitation.
5 Limitations
Despite the physical improvements wrought by virtual rehabilitation as reported in the 23 studies, there are several limitations which impact generalizability:
-
The absence of a control group for nine studies (i.e. (Blomqvist et al. 2021; Yoo et al. 2013; Van den Heuvel et al. 2014; An and Park 2018; Khurana et al. 2017; Aung and Al-Jumaily 2011; Gianola et al. 2020; Andreikanich et al. 2019; Villiger et al. 2017)).
-
A small sample size for the experimental group (ranging from 1 to 74) (Aung and Al-Jumaily 2011; Andreikanich et al. 2019; Wall et al. 2015).
-
Two studies focussed on healthy patients (Yen et al. 2011; Szturm et al. 2011).
-
A broad age range within the groups (from 18 to 85 years).
-
The lack of standard exercises in the training (Kaharan et al. 2016).
-
The lack of objective muscle power and balance measurements (Gianola et al. 2020).
-
The short duration of three studies (Jung et al. 2012).
-
The lack of follow up (Da Gama et al. 2016).
A number of the studies were also limited by: their dependence on a hospital setting (Kaharan et al. 2016) (this made it impossible to transfer the training to a home-setting post the study); the double blinded nature of the intervention (Trombetta et al. 2017) (related to the care needs) and the focus of the study on technology cost effectiveness instead of physical improvement (Trombetta et al. 2017).
This systematic review also includes a language bias, as only studies in English or French were reviewed; thus not every study could be included in the systematic review. Additionally, the search on only three databases (PubMed, ACM and Google Scholar) limited the choice of articles included in the study. Moreover, due to the paucity of studies on osteoporosis, experts in Rheumatology (JJC and BW) advised the inclusion of other care needs i.e., Ankylosing spondylitis, spinal cord injury, motor rehabilitation, post-stroke rehabilitation, shoulder abduction. As a result, virtual rehabilitation for these care needs was investigated. Related to this limitation, not every study focussed on older adults due to the wide range of care needs selected, (i.e. some studies related to younger people).
It would also have been interesting to include an analysis of studies regarding cybersickness in this review.
6 Conclusion
In this study, a systematic review was conducted to identify effective ways to design virtual rehabilitation to obtain physical improvement (e.g. balance and gait) and support engagement (i.e., motivation) for people with musculoskeletal disorders. A detailed presentation of the technologies has been made, in addition to outlining the training programmes, exergames and respective outcomes achieved.
Four distinct categories of device, enabling different degrees of immersion in a virtual environment for virtual rehabilitation were used in these studies: head-mounted display (HMD), balance board, body recognition camera and more specific devices (e.g. Datagloves, Youkicker). This paper contributes to the body of knowledge on virtual rehabilitation through its set of recommendations on technology choice and exercise training programme design. This knowledge should benefit both clinicians and researchers in the design and implementation of virtual rehabilitation solutions specific to the care needs of patients with musculoskeletal disorders including osteoporosis.
This study enabled us to define a list of recommendations to design virtual rehabilitation for older adults. In summary,
-
(1)
The exergames should be user-friendly and provide clear instruction and feedback. Additionally, a personalized experience is usually appreciated by patients and tends to increase their motivation and engagement.
-
(2)
The choice of device is dependent on the care need. For global body training, an HMD, camera or balance board is preferred.
-
(3)
The comfort and immersion of the patients will have an impact on the results of the training sessions, with HMDs being the most immersive.
-
(4)
Training programmes should be frequent but short in duration (e.g. 15–30 min and 2–3 times per week).
This review is important as osteoporosis affects 200 million people worldwide. The use of virtual rehabilitation has been shown to improve a patient’s physical abilities (e.g. balance, gait, muscle strength, body joint) and their motivation. Virtual rehabilitation can be used for patients with osteoporosis or other comparable musculoskeletal disorders with the goal of enhancing rehabilitation. Our review also shows that as there is a paucity of research regarding virtual rehabilitation for older adults with osteoporosis, this is a confirmation that this audience also requires similar HCI considerations.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
An C, Park Y (2018) The effects of semi-immersive virtual reality therapy on standing balance and upright mobility function in individuals with chronic incomplete spinal cord injury: a preliminary study. J Spinal Cord Med 41(2):223–229. https://doi.org/10.1080/10790268.2017.1369217
Andreikanich A, Santos B S, Amorim P, Zagalo H, Marques B, Margalho P, Laíns J, Faim F, Coelho M, Cardoso T, Dias P (2019) An exploratory study on the use of virtual reality in balance rehabilitation. 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 3416–3419. https://doi.org/10.1109/EMBC.2019.8857469
Aung YM, Al-Jumaily A (2011) Augmented reality based reaching exercise for shoulder rehabilitation. i-CREATE ’11: Proceedings of the 5th International Conference on Rehabilitation Engineering Assistive Technology, (50):1–4
Australian Commission on Safety and Quality in Health Care (2009) Preventing falls and harm from falls in older people. https://www.safetyandquality.gov.au/publications-and-resources/resource-library/preventing-falls-and-harm-falls-older-people-best-practice-guidelines-australian-hospitals. Accessed 21 August 2023
Bartlett HL, Ting LH, Bingham JT (2014) Accuracy of force and center of pressure measure of the Wii Balance Board. Gait Posture 39(1):224–228. https://doi.org/10.1016/j.gaitpost.2013.07.010
Baus O, Bouchard S (2014) Moving from virtual reality exposure-based therapy to augmented reality exposure-based therapy: a review. Front Hum Neurosci. https://doi.org/10.3389/fnhum.2014.00112
Berg K, Wood-Dauphine S, Williams JI, Gayton D (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 41(6):304–311. https://doi.org/10.3138/ptc.41.6.304
Blomqvist S, Seipel S, Engström M (2021) Using augmented reality technology for balance training in the older adults: a feasibility pilot study. BMC Geriatr 21(1):144. https://doi.org/10.1186/s12877-021-02061-9
Boettcher CE, Cathers I, Ginn KA (2008) Standard maximum isometric voluntary contraction tests for normalizing shoulder muscle EMG. J Ortho Res off Publ Ortho Res Soc 26(12):1591–1597. https://doi.org/10.1002/jor.20675
Boswell-Ruys CL, Sturnieks DL, Harvey LA, Sherrington C, Middleton JW, Lord SR (2009) Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil 90(9):1571–1577. https://doi.org/10.1016/j.apmr.2009.02.016
Browne J, O’Hare N (2000) Physiological measurement a quality control procedure for force platforms. Physiol Meas 21(4):515–524. https://doi.org/10.1088/0967-3334/21/4/308
Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, Jenkinson T (1994) A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 21(12):2281–2285
Chan WLS, Pin TW (2019) Reliability, validity and minimal detectable change of 2-min walk test and 10-m walk test in frail older adults receiving day care and residential care. Aging Clin Exp Res 32:597–604. https://doi.org/10.1007/s40520-019-01255-x
Cho GH, Hwangbo G, Shin HS (2014) The effects of virtual reality-based balance training on balance of the elderly. J Phys Ther Sci 26(4):615–617. https://doi.org/10.1589/jpts.26.615
Da Gama AEF, Chaves TM, Figueiredo LS, Baltar A, Meng M, Navab N, Teichrieb V, Fallavollita P (2016) MirrARbilitation: a clinically-related gesture recognition interactive tool for an AR rehabilitation system. Comput Meth Programs Biomed 135:105–114. https://doi.org/10.1016/j.cmpb.2016.07.014
Delbaere K, Close JCT, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR (2010) The Falls Efficacy Scale International (FES-I) A comprehensive longitudinal validation study. Age Age 39(2):210–216. https://doi.org/10.1093/ageing/afp225
Dencker A, Sunnerhagen KS, Taft C, Lundgren-Nilsson Å (2015) Multidimensional fatigue inventory and post-polio syndrome a Rasch analysis. Health Qual Life Outcomes. https://doi.org/10.1186/s12955-015-0213-9
Dimbwadyo-Terrer I, Trincado-Alonso F, De Los R-G, Aznar MA, Alcubilla C, Pérez-Nombela S, Del Ama-Espinosa A, Polonio-López B, Gil-Agudo A (2016) Upper limb rehabilitation after spinal cord injury: a treatment based on a data glove and an immersive virtual reality environment. Disabil Rehabil Assist Technol 11(6):462–467. https://doi.org/10.3109/17483107.2015.1027293
Dionyssiotis Y, Skarantavos G, Papagelopoulos P (2014) Modern rehabilitation in osteoporosis, falls, and fractures. Clin Med Insights Arthritis Musculoskelet Disord 7:33–40. https://doi.org/10.4137/CMAMD.S14077
Dittuno P, Dittuno J Jr (2001) Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord 39:654–656. https://doi.org/10.1038/sj.sc.3101223
Doward LC, McKenna SP, Meads DM, Twiss J, Revicki D, Wong RL, Luo MP (2007) Translation and validation of non-English versions of the Ankylosing Spondylitis Quality of Life (ASQOL) questionnaire. Health Qual Life Outcomes. https://doi.org/10.1186/1477-7525-5-7
Duncan PW, Weiner DK, Chandler J, Studenski S (1990) Functional reach: a new clinical measure of balance. J Gerontol 45(6):192–197. https://doi.org/10.1093/geronj/45.6.m192
Enright PL (2003) The six-minute walk test. Respir Care 48(8):783–785
Erjiang E, Wang T, Yang L, Dempsey M, Brennan A, Yu M, Chan WP, Whelan B, Silke C, O’Sullivan M, Rooney B, McPartland A, O’Malley G, Carey JJ (2020) The Irish dual-energy X-ray absorptiometry (DXA) health informatics prediction (HIP) for osteoporosis project. BMJ Open 10(12):e040488. https://doi.org/10.1136/bmjopen-2020-040488
Fabbri B, Berardi A, Tofani M, Panuccio F, Ruotolo I, Sellitto G, Galeoto G (2021) A systematic review of the psychometric properties of the Jebsen-Taylor Hand Function Test (JTHFT). Hand Surg Rehab 40(5):560–567. https://doi.org/10.1016/j.hansur.2021.05.004
Gardner MM, Buchner DN, Roberton MC, Campbell AJ (2001) Practical implementation of an exercise-based falls prevention programme. Age Ageing 30(1):77–83. https://doi.org/10.1093/ageing/30.1.77
Gianola S, Stucovitz E, Castellini G, Mascali M, Vanni F, Tramacere I, Banfi G, Tornese D (2020) Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: a randomized controlled trial. Medicine. https://doi.org/10.1097/MD.0000000000019136
Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, Giladi N, Holloway RG, Moore CG, Wenning GT, Yahr MD, Seild L (2004) Movement disorder society task force report on the Hoehn and Yahr staging scale: status and recommendation. Mov Disord 19(9):1020–1028. https://doi.org/10.1002/mds.20213
Gómez JF, Curcio C, Alvarado B, Zunzunegui V, Guralnik J (2013) Validity and reliability of the short physical performance battery (SPPB): a pilot study on mobility in the Colombian Andes. Colomb Med 44(3):165–171
Hagell P, Nygren C (2007) The 39 item Parkinson’s disease questionnaire (PDQ-39) revisited: implications for evidence-based medicine. J Neurol 78:1191–1198
Han J, Shao L, Xu D, Shotton J (2013) Enhanced computer vision with Microsoft Kinect sensor: a review. IEEE Trans Cybern 43(5):1318–1334. https://doi.org/10.1109/TCYB.2013.2265378
Hauser AR, Lyons KE, Pahwa R (2012) The UPDRS-8: a brief clinical assessment scale for Parkinson’s disease. Int J Neurosci 122(7):333–337. https://doi.org/10.3109/00207454.2012.657381
Hays RD, Morales LS (2009) The RAND-36 measure of health-related quality of life. Ann Med 33(5):350–357. https://doi.org/10.3109/07853890109002089
Ho PWT, Ma CC (2021) Musculoskeletal health in the community. In: Routledge (ed) The Routledge Handbook of Public Health and the Community., 1st edn. Taylor & Francis Group, London, pp 138–146
Im DJI, Ku J, Kim YJ, Cho S, Cho YK, Lim T, Lee HS, Kim HJ, Kang YJ (2015) Utility of a three-dimensional interactive augmented reality program for balance and mobility rehabilitation in the elderly: a feasibility study. Ann Rehabil Med 39(3):462–472. https://doi.org/10.5535/arm.2015.39.3.462
Itzkovich M, Shefler H, Front L, Gur-Pollack R, Elkayam K, Bluvshtein V, Gelernter I, Catz A (2018) SCIM III (Spinal Cord Independence Measure version III): reliability of assessment by interview and comparison with assessment by observation. Spinal Cord 56(1):46–51. https://doi.org/10.1038/sc.2017.97
Jerald J (2015) The VR Book: human-centered design for virtual reality. Assoc Comput Mach Morgan Claypool. https://doi.org/10.1145/2792790
Jung J, Yu J, Kang H (2012) Effects of virtual reality treadmill training on balance and balance self-efficacy in stroke patients with a history of falling. J Phys Ther Sci 24(11):1133–1136. https://doi.org/10.1589/jpts.24.1133
Kaharan AY, Tok F, Yildirim P, Ordahan B, Turkoglu G, Sahin N (2016) The effectiveness of exergames in patients with ankylosing spondylitis: a randomized controlled trial. Adv Clin Exp Med. 25(5):931–936. https://doi.org/10.17219/acem/32590
Kamper SJ, Ostelo RWJG, Knol DL, Maher CG, De Vet HCW, Hancock MJ (2010) Global Perceived Effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol 63(7):760–766. https://doi.org/10.1016/j.jclinepi.2009.09.009
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon : McCloskey E V, Willers C, Borgström F, (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16:82. https://doi.org/10.1007/s11657-020-00871-9
Kear BM, Guck TP, McGaha AL (2017) Timed up and go (TUG) test: normative reference values for ages 20 to 59 years and relationships with physical and mental health risk factors. J Prim Care Community Health 8(1):9–13. https://doi.org/10.1177/2150131916659282
Khasnis A, Gokula R M (2003) Romberg's test. J Postgrad Med. 49:169. Available from: https://www.jpgmonline.com/text.asp?2003/49/2/169/894. Accessed the 22 August 2023.
Khurana M, Walia S, Noohu MM (2017) Study on the effectiveness of virtual reality game-based training on balance and functional performance in individuals with paraplegia. Top Spinal Cord Inj Rehabil 23(3):263–270. https://doi.org/10.1310/sci16-00003
Kizony R, Raz L, Katz N, Weingarden H, Weiss PLT (2005) Video-capture virtual reality system for patients with paraplegic spinal cord injury. J Rehabil Res Dev 42(5):595–609. https://doi.org/10.1682/jrrd.2005.01.0023
Lavernia C, D’Apuzzo M, Rossi MD, Lee D (2008) Accuracy of knee range of motion assessment after total knee arthroplasty. J Arthroplasty 23(5):85–91. https://doi.org/10.1016/j.arth.2008.05.019
Lee HY, Kim YL, Lee SM (2015) Effects of virtual reality-based training and task-oriented training on balance performance in stroke patients. J Phys Ther Sci 27(6):1883–1888. https://doi.org/10.1589/jpts.27.1883
Lee J, Yoo H, Lee B (2017) Effects of augmented reality-based Otago exercise on balance, gait, and physical factors in elderly women to prevent falls: a randomized controlled trial. J Phys Ther Sci 29(9):1586–1589. https://doi.org/10.1589/jpts.29.1586
Lenze EJ, Munin MC, Quear T, Dew MA, Rogers JC, Begley AE, Reynolds CF (2004) The pittsburgh rehabilitation participation scale: reliability and validity of a clinician-rated measure f participation in acute rehabilitation. Arch Phys Med Rehabil 85(3):380–384. https://doi.org/10.1016/j.apmr.2003.06.001
Losilla F, Rosique F (2019) An augmented reality mirror exergame using 2d pose estimation. Proceedings of the 14th International Conference on Software Technologies, 643–648, https://doi.org/10.5220/0007798906430648
Mahoney FI, Barthel DW (1965) Barthel Index [Database record]. APA PsycTests. https://doi.org/10.1037/t02366-000
Maples-Keller J, Brunnell B, Sae-Jin RB (2017) The Use of Virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psych 25(3):103–113. https://doi.org/10.1097/HRP.0000000000000138
McCabe E, Ibrahim A, Singh R, Kelly M, Armstrong C, Heaney F, Bergin D, McCabe JP, Carey JJ (2020) A systematic review of the Irish osteoporotic vertebral fracture literature. Arch Osteoporos 15:34. https://doi.org/10.1007/s11657-020-0704-0
McDonough AL, Batavia M, Chen FC, Kwon S, Ziai J (2001) The validity and reliability of the GAITRite system’s measurements: a preliminary evaluation. Arch Phys Med Rehabil 82(3):419–425. https://doi.org/10.1053/apmr.2001.19778
Morse JM, Morse MR, Tylko SJ (1989) Development of a scale to identify the fall-prone patient. Can J Aging 8(4):366–377. https://doi.org/10.1017/S0714980800008576
Mubin O, Alnajjar F, Jishtu N, Alsinglawi B, Al Mahmud A (2019) Exoskeletons with virtual reality, augmented reality, and gamification for stroke patients’ rehabilitation: systematic review. JMIR Rehabil Assist Technol 6:2. https://doi.org/10.2196/12010
Omaña H, Bezaire K, Brady K, Davies J, Louwagie N, Power S, Santin S, Hunder SW (2021) Functional reach test, single-leg stance test and tinetti performance-oriented mobility assessment for the prediction of falls in older adult: a systematic review. Phys Therapy Hournal 101(10):1–18. https://doi.org/10.1093/ptj/pzab173
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw J M, Hróbjartsson A, Lalu M M, Li T, Loder E W, Mayo-Wilson E, McDonald S, McGuinness L. A, Steward L A, Thomas J, Tricco A C, Welch V A, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed.), 372(71) https://doi.org/10.1136/bmj.n71
Pandian S, Arya KN, Davidson EWR (2012) Comparison of Brunnstrom movement therapy and Motor Relearning Program in rehabilitation of post-stroke hemiparetic hand: a randomized trial. J Bodywork Movement Therap 16(3):330–337. https://doi.org/10.1016/j.jbmt.2011.11.002
Perlmutter JS (2009) Assessment of parkinson disease manifestations. Current Protocols Neurosci. https://doi.org/10.1002/0471142301.ns1001s49
Rabin R, De Charro F (2009) EQ-SD: a measure of health status from the EuroQol Group. An Med 33(5):337–343. https://doi.org/10.3109/07853890109002087
Rand D, Kizony R, Weiss P (2008) The sony playstation II EyeToy: low-cost virtual reality for use in rehabilitation. J Neurol Phys Therapy: JNPT 32(4):155–163. https://doi.org/10.1097/NPT.0b013e31818ee779
Roberts MH, Fletcher RB, Merrick PL (2014) The validity and clinical utility of the Hospital Anxiety and Depression Scale (HADS) with older adult New Zealanders. Int Psychogeriatr 26(2):325–333. https://doi.org/10.1017/S104161021300197X
Robertson JA, Kendall FP, McCreary EK (1984) Muscles testing and function (third edition). Br J Sports Med. 18(1):25
Roetenberg D, Luinge H, Slycke P (2009) Xsens MVN: Full 6DOF human motion tracking using miniature inertial sensors
Roos EM, Klässbo M, Lohmander LS (2009) WOMAC osteoarthritis Index: reliability, validity, and responsiveness in patients in arthroscopically assessed osteoarthritis. Scand J Rheumatol 28(4):210–215. https://doi.org/10.1080/03009749950155562
Scheman J, Ferguson L (2009) Patient global impression of change scores within the context of a chronic pain rehabilitation program. J Pain. https://doi.org/10.1016/j.jpain.2009.01.258
Shahid A, Wilkinson K, Marcu S, Shapiro C M (2012) STOP, THAT and one hundred other sleep scales. Springer New York, NY. https://doi.org/10.1007/978-1-4419-9893-4
Sharma S, Ghrouz AK, Hussain ME, Sharma S, Alsabbas M, Ansari S (2021) Progressive resistance exercises plus manual therapy is effective in improving isometric strength in overhead athletes with shoulder impingement syndrome: a randomized controlled trial. BioMed Res Int. https://doi.org/10.1155/2021/9945775
Singh S, Bajorek B (2014) Defining ’elderly’ in clinical practice guidelines for pharmacotherapy. Pharm Pract 12(4):489. https://doi.org/10.4321/s1886-36552014000400007
Song H, Peng W, Lee KM (2011) Promoting exercise self-efficacy with an exergame. J Health Commun 16:148–162. https://doi.org/10.1080/10810730.2010.535107
Sözen T, Özışık L, Başaran NÇ (2017) An overview and management of osteoporosis. Eur J Rheumatol 4(1):46–56. https://doi.org/10.5152/eurjrheum.2016.048
Staiano AE, Flynn R (2014) Therapeutic uses of active videogames: a systematic review. Games Health J 3:351–365. https://doi.org/10.1089/g4h.2013.0100
Szturm T, Betker AL, Moussavi Z, Desai A, Goodman V (2011) Effects of an interactive computer game exercise regimen on balance impairment in frail community-dwelling older adults: a randomized controlled trial. Phys Ther 91(10):1449–1462. https://doi.org/10.2522/ptj.20090205
Topley M, Richards JG (2020) A comparison of currently available optoelectronic motion capture systems. J Biomech. https://doi.org/10.1016/j.jbiomech.2020.109820
Trombetta M, Bazzanello Henrique PP, Brum MR, Colussi EL, De Marchi ACB, Rieder R (2017) Motion Rehab AVE 3D: A VR-based exergame for post-stroke rehabilitation. Comput Methods Programs Biomed 151:15–20. https://doi.org/10.1016/j.cmpb.2017.08.008
Valenzuela T, Okubo Y, Woodbury A, Lord SR, Delbaere K (2018) Adherence to technology-based exercise programs in older adults: a systematic review. J Geriatr Phys Ther 41:49–61. https://doi.org/10.1519/JPT.0000000000000095
Van den Heuvel MRC, Kwakkel G, Beek PJ, Berendse HW, Daffertshofer A (2014) Effects of augmented visual feedback during balance training in Parkinson’s disease: a pilot randomized clinical trial. Parkinsonism Related Disorders 20(12):1352–1358. https://doi.org/10.1016/j.parkreldis.2014.09.022
Villiger M, Liviero J, Awai L, Stoop R, Pyk P, Clijsen R, Curt A, Eng K, Bolliger M (2017) Home-based virtual reality-augmented training improves lower limb muscle strength, balance, and functional mobility following chronic incomplete spinal cord injury. Front Neurol 8:635. https://doi.org/10.3389/fneur.2017.00635
Wall T, Feinn R, Chui K, Cheng MS (2015) The effects of the Nintendo™ Wii Fit on gait, balance, and quality of life in individuals with incomplete spinal cord injury. J Spinal Cord Med 38(6):777–783. https://doi.org/10.1179/2045772314Y.0000000296
Wang Y, Bohannon RW, Kapellusch J, Garg A, Gershon RC (2015) Dexterity as measure with the 9-Hole Peg Test (9-HPT) across the age span. J Hand Ther 28(1):53–60. https://doi.org/10.1016/j.jht.2014.09.002
Weigl K, Forstner T (2020) Design of paper-based visual analogue scale items. Educ Psychol Measur 81(3):595–611. https://doi.org/10.1177/0013164420952118
Wildschut A, Rochette A, Filiatrault J, Plumier G (2020) Activities-specific balance confidence scale (abc scale). Stroke Engine 2023. https://strokengine.ca/en/assessments/activities-specific-balance-confidence-scale-abc-scale/. Accessed 22 August 2023
Willers C, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, McCloskey EU, Borgström F, Kanis JA (2022) Osteoporosis in Europe: a compendium of country-specific reports. Arch of Osteoporos 17:23. https://doi.org/10.1007/s11657-021-00969-8
Yen C, Lin K, Hu M, Wu R, Lu T, Lin C (2011) Effects of virtual reality-augmented balance training on sensory organization and attentional demand for postural control in people with Parkinson disease: a randomized controlled trial. Phys Ther 91(6):862–874. https://doi.org/10.2522/ptj.20100050
Yoo H, Chung E, Lee B (2013) The effects of augmented reality-based otago exercise on balance, gait, and falls efficacy of elderly women. J Phys Ther Sci 25(7):797–801. https://doi.org/10.1589/jpts.25.797
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Acknowledgements
This work was conducted with the financial support of the Science Foundation Ireland Centre for Research Training in Digitally-Enhanced Reality (d-real) under Grant No. 18/CRT/6224. For the purpose of Open Access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Funding
Open Access funding provided by the IReL Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest of declarations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thuilier, E., Carey, J., Dempsey, M. et al. Virtual rehabilitation for patients with osteoporosis or other musculoskeletal disorders: a systematic review. Virtual Reality 28, 93 (2024). https://doi.org/10.1007/s10055-024-00980-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10055-024-00980-7