Abstract
Stroke is the leading cause of motor impairments and generates distortion of body representation. Hence, stroke can modulate the sense of embodiment, namely the feeling of being inside the body (ownership), in the place where the body is located (location), and moving the body according to its own intentions (agency). A growing number of studies have adopted virtual reality (VR) to train motor abilities. However, the impact of the body illusion on the rehabilitation outcome is not fully understood. The present systematic review investigates the modulating role of the body illusion elicited by VR on motor rehabilitation in post-stroke patients after embodying a virtual avatar. The research was led in the main databases—PubMed, Scopus, PsychINFO, and Web of Science—and four studies matched the inclusion criteria (e.g., to have a sample of adult post-stroke patients, to use VR as an instrument for motor rehabilitation, to adopt the paradigm of the body illusion as a modulator for motor rehabilitation, to test the sense of body illusion outcome). Research outcomes demonstrated that two studies adopted the immersive and two the non-immersive embodied VR; three studies focused on the upper limb, and one on lower limb rehabilitation. Two studies compare VR training with traditional therapy, and two are pilot studies with only one experimental group. The studies demonstrated the feasibility of the body illusion as an accelerator for motor rehabilitation compared to the non-embodied condition, and as a positive correlator of the rehabilitation outcome. The finding should be taken with caution due to the limited studies included; however, they are encouraging to justify further research efforts in this area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Stroke is the leading cause of disability worldwide. It is estimated that around 650 million people around the globe, with an average of 60 years, are affected by stroke, and this number is expected to increase to 2 billion by 2050 (Tsao et al. 2022). In stroke survivors, the principal neurological consequence is hemiplegia or hemiparesis, which presents constrained mobility on one side of the body involving the paresis of the upper and/or lower limbs (Maenza et al. 2020). After discharge from the hospital, patients must undergo rehabilitation to restore their motor functions. However, only 25% of them can recover completely, and the remaining 75% of patients need constant and profound rehabilitation varying from weeks to several months or years (Langhorne et al. 2009).
1.1 The consequences of stroke on the sense of embodiment
A severe brain injury after a stroke affects neural plasticity and changes the survivors’ embodied experiences, which means the experiences of how post-stroke patients perceive the world through their bodies (Chen et al. 2010; Hosp and Luft 2011; Lo et al. 2023). Hence, brain damages distort the body representations that control proprioceptive and kinesthetic signals and the perception of peripersonal space, thus preventing the correct limbs' planning, preparation, and execution (Connell et al. 2008; Corredi Dell’Acqua and Tessari, 2010; Wallwork et al. 2016). In this perspective, stroke modulates the sense of embodiment referred to the feeling of being inside the body (ownership), in the place where the body is located (location), and moving the body according to own intentions (agency) (Kilteni et al. 2012). Furthermore, the sense of embodiment contributes to assimilating various aspects of self-consciousness, including sensation, emotions, and perception, into the physical body (Bloom 2018). These bodily alienations improve how the body is perceived consciously and may also cause disruptions in day-to-day activities, as healthy individuals usually perform bodily actions naturally and spontaneously without conscious efforts (Lo et al. 2023).
Considering the role of neural plasticity—the brain’s ability to adapt in order to foster functional activities (Murphy and Corbett 2009)—a growing number of studies in the field of multisensory integration techniques are adopting the body ownership illusions to modulate the distorted body representations after brain damage (Matamala-Gomez et al. 2020). One example is the mirror box, an instrument that permits the patient to embody a healthy arm reflected in the mirror. When the arm ownership illusion is achieved, the mirror box allows the patient to perceive the reflected arm as her own, positioned in place of the injured arm (Tosi et al. 2018; Yang et al. 2018). This technique has been recommended to restore the sensorimotor function of chronic stroke patients (Hatem et al. 2016). Furthermore, previous literature also demonstrated that practicing a physical task mentally can enhance performance and could be a promising technique for motor rehabilitation (Mulder 2007), besides reducing chronic pain, suffered by the majority of stroke patients, by activating the cortical areas related to the affected limb (Moseley 2004).
1.2 Embodiment manipulation through virtual reality
In recent years, virtual reality (VR) has been adopted to induce the body illusion for motor rehabilitation for both the upper (Weber et al. 2019) and lower limbs (In et al. 2016). VR is an advanced form of human–computer interface that allows participants to interact and become present in an immersive computer-generated virtual environment (Riva et al. 2016), besides inducing the body-swap-body illusion (Kilteni et al. 2012; Ventura et al. 2022a). So far, various meta-analyses and literature reviews have provided evidence for improved motor function and daily-life activity after VR-based training compared with standard intervention (Saposnik et al. 2011; Howard 2017; Lee et al. 2019). Patients generally accept the treatment through VR because it offers an engaging environment based on gamification, the personalization of the therapy depending on patients' clinical status, and the real-time feedback of cognitive and motor improvements (Shin et al. 2014). A recent approach to VR in rehabilitation implies embodied sensorimotor feedback where the patient’s movements in the real world are reproduced as an avatar’s movements in the virtual environment (Perez-Marcos et al. 2017). This embodied technology can be achieved by using motion capture technology that interprets the patient’s movements and provides multisensory feedback to the user about the movement’s performance (Adamovich et al. 2009). Moreover, the appropriate sensorimotor correlations received on a virtual body from a first-person perspective and colocated with the real body induce an illusion of ownership over that body (Maselli et al. 2013; Kokkinara and Slater 2014). The illusion induces changes in the patients' internal body representation and may strengthen the neural network involved in motor execution and consequently accelerate the rehabilitation process (Hsu et al. 2022). A previous narrative review discussed the advantages and potential of using body ownership illusions in VR to improve motor abilities (Matamala-Gomez et al. 2021). The same author proposed a novel post-stroke rehabilitation protocol aimed at modifying the internal representation of the upper limb through the 360-degree immersive video-based VR as a facilitator of motor rehabilitation (Matamala-Gomez et al. 2020).
1.3 The present work
The induction of body ownership illusion to elicit the patients to perceive their own body with an artificial one is increasingly adopted in motor rehabilitation after stroke. The present systematic review explores the potentiality of the body illusion through virtual reality to elicit and accelerate motor rehabilitation after stroke. The benefits of virtual reality on post-stroke rehabilitation are already well known (e.g., Gervasi et al. 2010; Zahabi et al. 2020; Augenstein et al. 2022; Juan et al. 2022); however, we intended to go one step further than reviews on this traditional virtual motor approach to rehabilitation after stroke and explore whether the body illusion paradigm could benefit sensorimotor rehabilitation even more. In particular, the research questions (RQ) of this study are:
-
RQ1: Does the body ownership illusion through VR improves the motor rehabilitation outcome after a stroke?
-
RQ2: What measures are used to assess the body illusion with stroke patients?
-
RQ3: What design and embodied virtual environments are adopted for motor rehabilitation with stroke patients?
2 Methods
The current systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al. 2009).
2.1 Study selection criteria
To be included in the systematic review, studies had to fulfil the following criteria: (a) to have a sample of post-stroke participants aged ≥ 18 years, (b) to use virtual reality as an instrument for motor rehabilitation, (c) to adopt the paradigm of the body ownership illusion as a modulator for motor rehabilitation, (d) to test the sense of body illusion outcome, (e) to be written in English, and (f) to have the full text available.
2.2 Search strategy
The systematic literature search was conducted on the PubMed, Scopus, PsychINFO, and Web of Science databases up to February 2023. The keywords were used in combinations as follows: {[(title-abs-key (embodiment) or title-abs-key ("body ownership")] and title-abs-key (stroke) and title-abs-key ("virtual reality")}.
2.3 Search outcome
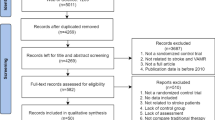
The initial search procedure led to 990 potentially relevant studies. After removing 35 duplicates, 948 titles and abstracts were read. Of those, 955 were removed because they did not match the focus of our research; in particular, they did not examine an adult sample (n = 19) with post-stroke injury (n = 560), and they did not assess the sense of body illusion (n = 358). The resulting 16 items were read, and 18 more studies were excluded because they did not match the following inclusion criteria: they did not examine post-stroke patients (n = 2), they did not adopt virtual reality as an instrument for motor rehabilitation (n = 10), and they did not assess the sense of body illusion (n = 2). Four studies were included in the analysis at the end of the literature search process (Fig. 1). The studies were selected individually by two researchers (S.V. and P.M.), and disagreements between researchers were resolved through discussion until a consensus was reached.
3 Results
The following sections organize the results. First, we synthesized the aim of the studies included in the review and described the sample. Then, we answered our second and third research questions (RQ2, RQ3), namely the study design focusing on the measures assessed, the VR apparatus and the virtual environment adopted, and the experimental procedure. Finally, we addressed the first research question (RQ1), and we summarized the main outcomes of the rehabilitation and the role of the embodiment as a modulator outcome (Table 1).
3.1 Aim of the studies
The study by Cha et al. (2021) aimed to investigate the feasibility of a tracking VR system that permits to control avatars' arms and fingers for the upper limbs post-stroke rehabilitation (Cha et al. 2021). The authors hypothesized that the virtual reality rehabilitation system (VRRS) could provide an effective rehabilitation training outcome for the upper limb's motor functions by enhancing the sense of body ownership of the patients through VR. The study by Tambone et al. (2021) investigated whether inducing a strong sense of body ownership illusion of a virtual body that performs walking movements might contribute to restoring motor functions in stroke patients in the absence of actual patients' movements. The authors compare two conditions—first- and third-person perspective—with the hypothesis that simply observing the virtual avatar moving in first-person perspective while sitting on a chair improves their motor ability more than in the third-person perspective. Fregna et al. (2022) intended to investigate the feasibility of an innovative immersive VR system for upper limb rehabilitation after stroke by adopting the paradigm of the arm illusion. Through a single group pilot study, the authors explored the patients’ body illusion score with the virtual upper limb, and if the rehabilitation system based on exergames improves the injury arm’s motor ability. Similarly, Perez-Marcos et al. (2017) studied the feasibility of a non-immersive VR embodied system for upper limb motor rehabilitation through exergames by embodying a virtual arm.
3.2 Sample characteristics
A total of 58 post-stroke patients were included in the systematic review. The study of Cha et al. (2021) consists of 27 patients, 15 male and 12 female, with an average age of 46 years old (SD = 21.6). These patients had undergone occupational and physical therapy and had a different levels of disability, with Fugl-Meyer (Fugl-Meyer et al. 1975) scores ranging from 4 to 58 (M = 24.0; SD = 17.8). The second study by Tambone et al. (2021) includes 12 patients with left-hemisphere damage, 8 male and 4 female, with an average age of 58.67 years old (SD = 2.89) recruited from the hospital where they were being treated for chronic non-fluent aphasia with no comprehension deficits. Fregna et al. (2022) study included 16 subacute and chronic post-stroke patients, 4 female and 12 men, with an average age of 62 years old (SD = 9), 5 with hemorrhagic stroke. These patients had a wide range of motor impairments with the Fugl-Meyer score ranging from 30 to 60 (M = 36.2; SD = 15). However, only 9 patients completed all the training sessions. The study of Perez-Marcos et al. (2017) involved 10 chronic stroke-survivors, 9 with ischemic stroke, 4 male and 6 female, with an average age of 55 years old (SD = 13.1). All participants reported a proper upper limb motor ability to lead the rehabilitation program tested by the Medical Research Council Scale for shoulder elevation and elbow flexion and extension.
3.3 Outcome measures
3.3.1 Motor abilities
The administered tests assess the motor abilities before and after the training. In particular, the study of Tambone et al. (2021) tested the patients' walking ability through the 10 Meter Walk Test (Bohannon 1997), the Wisconsin Gait Scale (Rodriquez et al. 1996), the Walking While Talking (Verghese et al. 2007), the 30 Seconds Sit-to-Stand Test (Jones et al. 1999), the Rivermead Mobility Index (Nair and Wade 2003), and the balance ability through the Berg Balance Scale (Berg 1992), the Dynamic Gait Index (Marchetti et al. 2008), and the Timed Up and Go test (Podsiadlo and Richardson 1991). To evaluate the upper limb motor ability was adopted the Fugl-Meyer scale (hereafter, FM; Fugl-Meyer et al. 1975). Cha et al. (2021) used the FM scale to evaluate the change on upper limb functionality comparing the patients’ score before to after the VR training. On the contrary, Fregna et al. (2022) used the FM scale only at baseline. Perez-Marcos et al. (2017) used the Medical Research Council Scale for shoulder elevation and elbow flexion and extension only at baseline, as a screening for the patients’ upper limb ability.
3.3.2 Embodiment measures
According to our second research question (RQ2), the studies included in the review have assessed two different types of embodiment questionnaires, adapted from Gonzalez-Franco et al. (2018) (Cha et al. 2021; Fregna et al. 2022), and ad-hoc questionnaires generated by the authors (Tambone et al. 2021; Perez-Marcos et al. 2017) and adapted from previous studies (Kokkinara et al. 2016; Burin et al. 2019) (Table 2).
3.4 Virtual reality apparatus and training tasks
The third research question (RQ3) of the present review showed that the studies included adopted both immersive and non-immersive technologies. The study by Cha et al. (2021) adopted a non-immersive VR system. The apparatus consists of two cameras (BFS-U3–13Y3C-C, FLIR Systems, Inc.) and two computers, one including Unity software (Windows 8, Intel Core i7–6700 at 3.40 GHz, and 8 GB RAM), and one working as a server (Linux, Intel Core i9–9900 k at 3.60 GHz and 32 GB RAM and RTX2080TI) that collects the data by tracking the patients' upper limb with fingers movements. The experimental group used a kinematic system for upper-limb tracking that captured the patients’ limb movements and reproduced them on the screen. The advantage of this system is the degree of freedom of the movements as the system can capture a large range around the camera and enhance the realism of an avatar’s upper-limb behavior. One control group used the Leap Motion controller, a tracker system with a small range of movements above the device with the consequence that only the participants’ hands, and not the entire arms, can be tracked. The training consists of three tasks: (1) normal motion on a plane in which the patients are invited to reach a virtual object on a plane in a fixed slot of time, (2) mirrored motion on a plane in which the avatar's left upper limb is controlled by the subjects opposite limb, (3) grasping motion in which patients are invited to reach and grasp random virtual objects that are on a plane.
The study of Tambone et al. (2021) adopted an immersive VR system with the Oculus Rift CV1 equipped with two PenTile organic light-emitting diode displays (1080 × 1200 pixels, refresh rate = 90 Hz, field of view = 110° with 6° of freedom). The scenario was written and implemented using the Unity software. The experiment consists of two phases: (1) embodiment induction, in which patients are invited to embody a virtual avatar gender-matched from a first-person perspective and a third-person perspective, and (2) training, in which patients observe the walking avatar at a different speed level, and perspective according to the conditions group.
The study of Fregna et al. (2022) implemented an immersive VR system with the Quest 2 head-mounted display (HMD), and the patient’s application running by Windows that wirelessly communicates with the HMD. During the task execution, the patient’s real hands are captured by the Oculus Quest and projected into the virtual environment in first-person perspective to elicit the body illusion. The single training session included four tasks based on exergames where patients are invited to play various games with a virtual ball.
Perez-Marcos et al. (2017) study used a non-immersive VR developed with the MindMotion™ PRO software (MindMaze SA, Switzerland), usually adopted for functional training of the upper limb after brain damage. The mobile platform comprises a 3D motion tracking camera and a touch screen with an embedded computer. The camera captures, tracks, and interprets the participant’s movements, which are then displayed by the virtual avatar in first-person or third-person perspective. These movements are integrated into functional tasks, including pointing, reaching, and grasping virtual objects to rehabilitate the upper limb while the patients sit on a chair.
3.5 Study design
Results show two randomized studies reporting a study with 5 days-session (Cha et al. 2021) and a study with 12 days-session (Tambone et al. 2021). Two studies reported a single-group protocol where a study adopted a single day-session (Fregna et al. 2022), and the second study a 5 weeks rehabilitation protocol, two days a week (Perez-Marcos et al. 2017). Table 3 illustrates the experimental design of the studies included.
3.6 The modulating role of embodiment
The first research question (RQ1) was also satisfied. Two studies (Cha et al. 2021; Tambone et al. 2021) reported a significant improvement in the outcome's measures of motor abilities from before to after the experiment for the embodied condition compared to the control group. Tambone et al. (2021) results demonstrated a significant effect on embodied condition to improve the speed walking ability compared to the control condition (η2 = 0.71) assessed by the 10 Meter Walk Test. Moreover, the body ownership illusion was a significant positive predictor of motor abilities change (effect on Wisconsin Gait scale, R2 = 0.66), demonstrating that the stronger the illusion, the greater the motor improvement (Tambone et al. 2021). Cha et al. (2021) found a significant difference in upper limb motor ability assessed by Fugl-Meyer from before to after the motor training sessions between the VRRS group and the traditional rehabilitation (p < 0.001). However, the study's effect size was small (η2.36). No regression analysis was reported in the study regarding the sense of embodiment score. However, the authors found a significant difference between the VRRS condition and the control group (Leap Motion) for the factors of agency (p = 0.049), and ownership (p = 0.044), demonstrating the efficacy of the immersive VR in inducing the body illusion. The Perez-Marcos et al. (2017) study reported a significant improvement in upper limb function and shoulder flexion from before to after the embodied VR rehabilitation program (p = 0.007). However, participants did not reach a significant level of agency with the virtual arm (p = 0.546). Finally, Fregna et al. (2022) found a significant negative correlation between the completion times and Fugl-Meyer score (correlation = − 0.69; p < 0.05), explaining that the baseline patients’ motor ability is important for task performance. Furthermore, the patients reach a significant level of embodiment for the factors of ownership (p < 0.001), and agency (p < 0.001).
Table 4 reports the mean and standard deviation on the embodiment scores for both the experimental and control groups.
4 Discussion
The present systematic review investigated the modulating role of the body illusion through VR to promote motor rehabilitation after a stroke. Motor impairments are the main consequence of stroke, together with alteration in body representation and the sense of embodiment that prevent limb movements. Our first research question (RQ1), exploring whether the body ownership illusion through VR improves the motor rehabilitation outcome after a stroke, was well addressed. The reviewed studies demonstrated that inducing a body ownership illusion through VR could facilitate motor rehabilitation both for the upper (Perez-Marcos et al. 2017; Cha et al. 2021, Fregna et al. 2022) and lower limbs (Tambone et al. 2021), compared to the control non-embodied condition. This may happen because visual feedback, in terms of synchronized stimulation between the patient’s real body and the artificial body provided by the virtual environment, can affect the patient's cognition and rehabilitation (Kilteni et al. 2013). The study by Tambone et al. (2021) well highlights the modulating role of the embodiment with significant results and great effect size on body illusion as a positive predictor of motor rehabilitation change. Along the same line, the studies of Cha et al. (2021) and Fregna et al. (2022) found a significant score for the factors of ownership and agency of the embodiment scale, demonstrating the feasibility of VR to elicit body illusion in stroke patients. On the contrary, Perez-Marcos et al. (2017) did not find a significant score on agency because the patients could not perceive the avatar upper limb movements as their own. The negative results on agency confirm previous work on embodiment after stroke, which demonstrated the feasibility of VR to induce the illusion of ownership and location, but not the illusion of agency (Borrego et al. 2019). This may be because it could be challenging for the patients’ injured limb, characterized by not-fluid movements, to synchronize their own movements with the virtual arm. Hence, the illusion of moving the avatar is not satisfied (Borrego et al. 2019).
The third research question (RQ3) regarding the design and the embodied virtual environment for motor rehabilitation after a stroke was strongly fulfilled. Two studies provided a weekly rehabilitation protocol (Cha et al. 2021; Tambone et al. 2021), and one study used a five weeks program (Perez-Marcos et al. 2017), usually adopted in the protocol for upper limb rehabilitation through VR (Henderson et al. 2007). Only one study included in the review adopted a single day-session (Fregna et al. 2022) as the aim was to investigate the feasibility of a novel VR embodied system to elicit the arm illusion for motor rehabilitation by practicing exergames. In this line, more standardized protocols are needed to clarify the proper timeline to restore the upper limb after a stroke through an embodied VR system. Furthermore, it is interesting to highlight the different types of training adopted by the authors. In three studies, the patients actively played various exergame with their limbs while immersed in the virtual environment, such as playing with a virtual ball or reaching some targets with the arm (Perez-Marcos et al. 2017; Cha et al. 2021, Fregan et al. 2022), whereas, in one study, the patients simply observe the avatar walking randomly in VR from a first-person perspective (experimental group) or a third-person perspective (control group) without making any active movement (Tambone et al. 2021). Future studies might be necessary to investigate whether there is a difference between active exergame or observation training while embodying a virtual avatar to improve the somatosensory integration of motor functions. Following this point, previous literature underlines that simply observing a motor action through the mirror increases attentional demands for integrating vision, proprioception and neural activity in multisensory areas associated with self-awareness and spatial attention (Chen et al. 2018). These effects may translate into an increased awareness of the affected limb; in fact, the action observation therapy (Ertelt et al. 2007; Mulder 2007) was developed to activate the motor system through vision by generating an internal representation of the observed action that can be targeted for motor learning. Observing an action with the intention of later imitating it is essential to prepare the motor system for execution (Rumiati et al. 2005; Sale and Franceschini 2012; Tessari et al. 2021) and also implies the activation of the corresponding body parts (Schwoebelet al 2004; Ottoboni et al. 2022). Similarly, the reviewed VR studies suggest that body ownership plays an essential role in repairing motor functioning, probably due to acting on the motor intentions, neurocognitive network and processes.
The key point of the review is the modulating role of the body ownership illusion experienced by the patients during the training. In the studies, patients reached a high sense of body illusion contributing to the outcome of the motor abilities, especially for the factor of ownership and location. In particular, the body illusion was a positive predictor of motor rehabilitation: patients who perceived the body avatar as their own body improved their gait and balance abilities better than those who did not reach the illusion (Tambone et al. 2021). The added value of the embodied VR system, compared to traditional rehabilitation programs such as the mirror box, is the capacity to stimulate motor imagery with computerized images, and the patient can receive remote feedback about the training; in this way, the patient knows if they are performing the rehabilitation tasks correctly. Moreover, the VR have a high-tracking system that facilitates a fidelity reproduction of the patient’s limb, promoting the illusion of ownership. However, the level at which body ownership activates the motor system and allows body recovery is still unclear. A recent study, excluded from the review because it focused on patients with a distal radius fracture, investigated the effects of embodied VR training on upper limb orthopedic rehabilitation. Results showed that patients who embodied a virtual body and combined motor imagery through action planning and action observation significantly improved the functional ability of the injured limb and accelerated the rehabilitation treatment, compared to the non-embodied control group. The authors found that functional recovery highly correlated with the feeling of ownership and agency over the virtual arm (Matamala-Gomez et al. 2022). Future studies should focus on understanding the potential of being immersed in a virtual body while performing immersive VR training based on action execution or action observation to improve and accelerate the motor rehabilitation process, besides understanding the variables that could elicit or inhibit the patients from reaching body illusion in VR.
Apart from the interesting insight received from the review, it is also important to underline its limits. First, the number of studies is insufficient to draw any final conclusions on the impact of body illusion on motor rehabilitation. The review only includes four studies, and most of the articles found on the databases were excluded as they did not assess the sense of body illusion, even if they adopt the avatar to simulate the patient's body, or the authors did not investigate the modulating role of the body ownership illusion for rehabilitation (e.g., Perez-Marcos 2018; Ferreira et al. 2019; Song and Kim 2019). The body illusion through VR is not a novel field of investigation; however, its modulating role in improving motor abilities is not investigated. The second limitation arose from the second research question (RQ2) regarding the measures used to assess the body illusion. The review figured out the lack of a standardized embodiment questionnaire adopted by the authors. The studies administered ad-hoc questionnaires, and the results' interpretation should be cautiously taken. Future protocols could introduce implicit measures such as heart rate variability or skin conductance to assess the body illusion even though they have been demonstrated to be not sensitive enough in some studies (e.g., Critchley et al. 2021). To overcome the limit of the heterogeneity of the embodiment questionnaires, Table 2 of the present work could serve as reference for future researchers to set the items for assessing the embodiment by self-report questionnaire. Moreover, it could be interesting to measure the interoception to evaluate the sensory-motor integration of the injured limb. The third limit of the review is the absence of the follow-up assessment after the training program, so it was impossible for the authors to check the stability of the changes and whether the motor abilities last over time. At last, there is a lack of correlational analysis between the patients’ experience with VR in terms of sense of presence and cybersickness and the rehabilitation outcome. In the present review, only one study assessed the participants’ feeling of immersion and comfort with the virtual environment (Perez-Marcos et al. 2017). However, the authors did not analyze how the experience modulates the rehabilitation program. Previous literature underlines that cybersickness could negatively compromise the positive outcome of the rehabilitation program (Veličković and Milovanović, 2021), and it depends on the type of the VR program and the degree of interaction (Impellizari et al. 2022). Moreover, it was demonstrated that the sense of presence is a positive predictor of the sense of body ownership illusion, so a lack of presence could compromise the body illusion that is essential for the study outcome (Ventura et al. 2022b). Future studies based on VR rehabilitation should consider the dependent variables in terms of patients’ motor ability change and the independent variable of cybersickness and presence and how they interact with the dependent variables as it may compromise the rehabilitation outcome. One possible solution could be to execute a pilot study first to investigate if the VR program may generate cybersickness and the sense of presence in the patients and then start with the clinical trial.
Apart from the limitation, we believe that the research topic of the review could be a promising area in motor rehabilitation after stroke and could lay the groundwork that the body illusion is a crucial aspect to consider when therapists decide to work with the paradigm. In fact, if the patient does not reach the body illusion, this could compromise the outcome of the rehabilitation program. Future direction should consider testing the patients' capacity to embody the virtual avatar and then continuing with the training program.
5 Conclusion
The review presents the emerging field of the modulating role of the body illusion through virtual reality for post-stroke rehabilitation. The higher is the sense of body illusion perceived by the patients toward a virtual avatar, the higher is the score on motor abilities outcome. Despite the limits, the results encourage further research efforts in this area.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Adamovich SV, Fluet GG, Tunik E, Merians AS (2009) Sensorimotor training in virtual reality: a review. NeuroRehabilitation 25(1):29–44
Augenstein TE, Kortemeyer D, Glista L, Krishnan C (2022) Enhancing mirror therapy via scaling and shared control: a novel open-source virtual reality platform for stroke rehabilitation. Virtual Real 1–14
Berg K (1992) Measuring balance in the elderly: development and validation of an instrument. McGill University
Bloom K (2018) The embodied self: movement and psychoanalysis. Routledge
Bohannon RW (1997) Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Age 26(1):15–19. https://doi.org/10.1093/ageing/26.1.15
Borrego A, Latorre J, Alcañiz M, Llorens R (2019) Embodiment and presence in virtual reality after stroke. A comparative study with healthy subjects. Front Neurol. https://doi.org/10.3389/fneur.2019.01061
Burin D, Kilteni K, Rabuffetti M, Slater M, Pia L (2019) Body ownership increases the interference between observed and executed movements. PLoS ONE. https://doi.org/10.1371/journal.pone.0209899
Cha K, Wang J, Li Y, Shen L, Chen Z, Long J (2021) A novel upper-limb tracking system in a virtual environment for stroke rehabilitation. J Neuroeng Rehabil 18:1–13
Chen H, Epstein J, Stern E (2010) Neural plasticity after acquired brain injury: evidence from functional neuroimaging. PM&R 2:S306–S312. https://doi.org/10.1016/j.pmrj.2010.10.006
Chen X, Liu F, Yan Z, Cheng S, Liu X, Li H, Li Z (2018) Therapeutic effects of sensory input training on motor function rehabilitation after stroke. Medicine 97:48
Connell LA, Lincoln NB, Radford KA (2008) Somatosensory impairment after stroke: frequency of different deficits and their recovery. Clin Rehabil 22(8):758–767
Corradi-Dell’Acqua C, Tessari A (2010) Is the body in the eye of the beholder? Visual processing of bodies in individuals with anomalous anatomical sensory and motor features. Neuropsychologia 48(3):689–702
Critchley HD, Botan V, Ward J (2021) Absence of reliable physiological signature of illusory body ownership revealed by fine-grained autonomic measurement during the rubber hand illusion. PLoS ONE 16(4):e0237282
Ertelt D, Small S, Solodkin A, Dettmers C, McNamara A, Binkofski F, Buccino G (2007) Action observation has a positive impact on rehabilitation of motor deficits after stroke. Neuroimage 36:164–173. https://doi.org/10.1016/j.neuroimage.2007.03.043
Ferreira B, Lourenco J, Menezes P (2019) A serious game for post-stroke motor rehabilitation. In: Proceedings of the 2019 5th experiment at international conference, Exp.at 2019, pp 383–387. https://doi.org/10.1109/expat.2019.8876493
Fregna G, Schincaglia N, Baroni A, Straudi S, Casile A (2022) A novel immersive virtual reality environment for the motor rehabilitation of stroke patients: A feasibility study. Frontiers in Robotics and AI, 225. https://doi.org/10.3389/frobt.2022.906424
Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S (1975) A method for evaluation of physical performance. Scand J Rehabil Med 7:13–31
Gervasi O, Magni R, Zampolini M (2010) Nu! RehaVR: virtual reality in neuro tele-rehabilitation of patients with traumatic brain injury and stroke. Virtual Real 14:131–141
Gonzalez-Franco M, Peck TC (2018) Avatar embodiment towards a standardized questionnaire. Front Robot AI 5:74. https://doi.org/10.3389/frobt.2018.00074
Hatem SM, Saussez G, Della Faille M, Prist V, Zhang X, Dispa D, Bleyenheuft Y (2016) Rehabilitation of motor function after stroke: a multiple systematic review focused on techniques to stimulate upper extremity recovery. Front Hum Neurosci 10:442. https://doi.org/10.3389/fnhum.2016.00442
Henderson A, Korner-Bitensky N, Levin M (2007) Virtual reality in stroke rehabilitation: a systematic review of its effectiveness for upper limb motor recovery. Top Stroke Rehabil 14(2):52–61. https://doi.org/10.1310/tsr1402-52
Hosp JA, Luft AR (2011) Cortical plasticity during motor learning and recovery after ischemic stroke. Neural Plast. https://doi.org/10.1155/2011/871296
Howard MC (2017) A meta-analysis and systematic literature review of virtual reality rehabilitation programs. Comput Hum Behav 70:317–327
Hsu HY, Kuo LC, Lin YC, Su FC, Yang TH, Lin CW (2022) Effects of a virtual reality–based mirror therapy program on improving sensorimotor function of hands in chronic stroke patients: a randomized controlled trial. Neurorehabil Neural Repair 36(6):335–345
Impellizzeri F, Naro A, Basile G, Bramanti A, Gazia F, Galletti F, Milardi D (2022) Does cybersickness affect virtual reality training using the Computer Assisted Rehabilitation Environment (CAREN)? Preliminary results from a case-control study in Parkinson’s disease. Physiother Theory Practic. https://doi.org/10.1080/09593985.2021.1964117
In T, Lee K, Song C (2016) Virtual reality reflection therapy improves balance and gait in patients with chronic stroke: randomized controlled trials. Med Sci Monit Int Med J Exp Clin Res 22:4046
Jones CJ, Rikli RE, Beam WC (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport 70(2):113–119
Juan M, et al. (2022). Immersive virtual reality for upper limb rehabilitation: comparing hand and controller interaction. Virtual Real 1–15
Kilteni K, Bergstrom I, Slater M (2013) Drumming in immersive virtual reality: the body shapes the way we play. In: IEEE transactions on visualization and computer graphics, 19 (20th IEEE Virtual Reality Conference (VR)), pp 597–605. https://doi.org/10.1109/TVCG.2013.29
Kilteni K, Groten R, Slater M (2012) The sense of embodiment in virtual reality. Presence-Teleoper Virtual Environ 21(4):373–387. https://doi.org/10.1162/PRES_a_00124
Kokkinara E, Kilteni K, Blom KJ, Slater M (2016) First person perspective of seated participants over a walking virtual body leads to illusory agency over the walking. Sci Rep 6(1):28879
Kokkinara E, Slater M (2014) Measuring the effects through time of the influence of visuomotor and visuotactile synchronous stimulation on a virtual body ownership illusion. Perception 43(1):43–58
Langhorne P, Coupar F, Pollock A (2009) Motor recovery after stroke: a systematic review. Lancet Neurol 8(8):741–754
Lee HS, Park YJ, Park SW (2019) The effects of virtual reality training on function in chronic stroke patients: a systematic review and meta-analysis. BioMed Res Int 2019
Lo TLT, Lee JLC, Ho RTH (2023) Recovery beyond functional restoration: a systematic review of qualitative studies of the embodied experiences of people who have survived a stroke. BMJ Open 13(2):e066597
Maenza C, Good DC, Winstein CJ, Wagstaff DA, Sainburg RL (2020) Functional deficits in the less-impaired arm of stroke survivors depend on hemisphere of damage and extent of paretic arm impairment. Neurorehabil Neural Repair 34(1):39–50
Marchetti GF, Whitney SL, Blatt PJ, Morris LO, Vance JM (2008) Temporal and spatial characteristics of gait during performance of the Dynamic Gait Index in people with and people without balance or vestibular disorders. Phys Ther 88(5):640–651
Maselli A, Slater M (2013) The building blocks of the full body ownership illusion. Front Hum Neurosci 7:83. https://doi.org/10.3389/fnhum.2013.00083
Matamala-Gomez M, Malighetti C, Cipresso P, Pedroli E, Realdon O, Mantovani F, Riva G (2020) Changing body representation through full body ownership illusions might foster motor rehabilitation outcome in patients with stroke. Front Psychol. https://doi.org/10.3389/fpsyg.2020.01962
Matamala-Gomez M, Maselli A, Malighetti C, Realdon O, Mantovani F, Riva G (2021) Virtual body ownership illusions for mental health: a narrative review. J Clin Med 10(1):139. https://doi.org/10.3390/jcm10010139
Matamala-Gomez M, Slater M, Sanchez-Vives MV (2022) Impact of virtual embodiment and exercises on functional ability and range of motion in orthopedic rehabilitation. Sci Rep 12(1):5046. https://doi.org/10.1038/s41598-022-08917-3
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Reprint—preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Phys Ther 89(9):873–880
Moseley GL (2004) Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain 108(1–2):192–198. https://doi.org/10.1016/j.pain.2004.01.006
Mulder T (2007) Motor imagery and action observation: cognitive tools for rehabilitation. J Neural Transm 114:1265–1278
Murphy TH, Corbett D (2009) Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci 10(12):861–872
Nair KPS, Wade DT (2003) Changes in life goals of people with neurological disabilities. Clin Rehabil 17(7):797–803
Ottoboni G, et al. (2022) Paradoxical decrease of imitation performance with age in children. bioRxiv, 2022–04.
Perez-Marcos D (2018) Virtual reality experiences, embodiment, videogames and their dimensions in neurorehabilitation. J Neuroeng Rehabil. https://doi.org/10.1186/s12984-018-0461-0
Perez-Marcos D, Chevalley O, Schmidlin T, Garipelli G, Serino A, Vuadens P, Millán JDR (2017) Increasing upper limb training intensity in chronic stroke using embodied virtual reality: a pilot study. J Neuroeng Rehabil 14:1–14. https://doi.org/10.1186/s12984-017-0328-9
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148
Riva G, Baños RM, Botella C, Mantovani F, Gaggioli A (2016) Transforming experience: the potential of augmented reality and virtual reality for enhancing personal and clinical change. Front Psych 7:164
Rodriquez AA, Black PO, Kile KA, Sherman J, Stellberg B, McCormick J, Roszkowski J, Swiggum E (1996) Gait training efficacy using a home-based practice model in chronic hemiplegia. Arch Phys Med Rehabil 77(8):801–805
Rumiati RI, Weiss PH, Tessari A, Assmus A, Zilles K, Herzog H, Fink GR (2005) Common and differential neural mechanisms supporting imitation of meaningful and meaningless actions. J Cogn Neurosci 17(9):1420–1431. https://doi.org/10.1162/0898929054985374
Sale P, Franceschini M (2012) Action observation and mirror neuron network: a tool for motor stroke rehabilitation. Eur J Phys Rehabil Med 48(2):313–318
Saposnik G, Levin M, Group, S. O. R. C. (SORCan) W (2011) Virtual reality in stroke rehabilitation: a meta-analysis and implications for clinicians. Stroke 42(5):1380–1386
Schwoebel J, Buxbaum LJ, Branch Coslett H (2004) Representations of the human body in the production and imitation of complex movements. Cogn Neuropsychol 21(2–4):285–298
Shin J-H, Ryu H, Jang SH (2014) A task-specific interactive game-based virtual reality rehabilitation system for patients with stroke: a usability test and two clinical experiments. J Neuroeng Rehabil 11(1):1–10
Song M, Kim J (2019) A paradigm to enhance motor imagery using rubber hand illusion induced by Visuo-Tactile Stimulus. IEEE Trans Neural Syst Rehabil Eng 27(3):477–486. https://doi.org/10.1109/TNSRE.2019.2895029
Tambone R, Giachero A, Calati M, Molo MT, Burin D, Pyasik M, Cabria F, Pia L (2021) Using body ownership to modulate the motor system in stroke patients. Psychol Sci 32(5):655–667. https://doi.org/10.1177/0956797620975774
Tessari A, Proietti R, Rumiati RI (2021) Bottom-up and top-down modulation of route selection in imitation. Cogn Neuropsychol 38(7–8):515–530. https://doi.org/10.1080/02643294.2022.2043264
Tosi G, Romano D, Maravita A (2018) Mirror box training in hemiplegic stroke patients affects body representation. Front Hum Neurosci 11:617
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y (2022) Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation 145(8):e153–e639
Veličković P, Milovanović M (2021) Improvement of the interaction model aimed to reduce the negative effects of cybersickness in VR rehab applications. Sensors 21(2):321. https://doi.org/10.3390/s21020321
Ventura S, Cebolla A, Latorre J, Escrivá-Martínez T, Llorens R, Baños R (2022a) The benchmark framework and exploratory study to investigate the feasibility of 360-degree video-based virtual reality to induce a full body illusion. Virtual Real. https://doi.org/10.1007/s10055-021-00567-6
Ventura S, Miragall M, Cardenas G, Baños RM (2022b) Predictors of the sense of embodiment of a female victim of sexual harassment in a male sample through 360-degree video-based virtual reality. Front Hum Neurosci 16:845508
Verghese J, Kuslansky G, Holtzer R, Katz M, Xue X, Buschke H, Pahor M (2007) Walking while talking: effect of task prioritization in the elderly. Arch Phys Med Rehabil 88(1):50–53
Wallwork SB, Bellan V, Catley MJ, Moseley GL (2016) Neural representations and the cortical body matrix: implications for sports medicine and future directions. Br J Sports Med 50(16):990–996. https://doi.org/10.1136/bjsports-2015-095356
Weber LM, Nilsen DM, Gillen G, Yoon J, Stein J (2019) Immersive virtual reality mirror therapy for upper limb recovery following stroke: A pilot study. Am J Phys Med Rehabil 98(9):783
Yang Y, Zhao Q, Zhang Y, Wu Q, Jiang X, Cheng G (2018) Effect of mirror therapy on recovery of stroke survivors: a systematic review and network meta-analysis. Neuroscience 390:318–336
Zahabi M, Abdul Razak AM (2020) Adaptive virtual reality-based training: a systematic literature review and framework. Virtual Reality 24:725–752
Acknowledgements
This work was supported by the Margarita Salas postdoctoral fellowship, Ministry of Universities of the Government of Spain (European Union NextGeneration EU, ref. UP2021-044).
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflict of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ventura, S., Marchetti, P., Baños, R. et al. Body ownership illusion through virtual reality as modulator variable for limbs rehabilitation after stroke: a systematic review. Virtual Reality 27, 2481–2492 (2023). https://doi.org/10.1007/s10055-023-00820-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10055-023-00820-0