Abstract
Invasive techniques such as venipuncture are painful procedures causing stress and anxiety, both in pediatric patients and in their carers. For this reason, efforts are being made to develop mitigating strategies for the patient’s pain and anxiety during the performance. To analyze and evaluate the effectiveness of the use of Virtual Reality distraction techniques as a measure of pain and anxiety reduction in pediatric patients and their parents. In addition, the effects of two modes of Virtual Reality (passive vs. interactive) were compared. A quasi-experimental study was carried out in the pediatric emergency department of a tertiary referral hospital in north Spain. The participants were children who underwent venipuncture for blood extraction and vascular cannulation. From the 124 patients, 51.6% (n = 64) were girls and 48.4% (n = 60) were boys (p = 0.574). The mean age was 8.4 years (SD: 4.1). The mean level of pain experienced was 2.33 (SD: 0.76) in the interactive VR group (n = 88) versus 2.67 (SD: 1.35) in patients with passive VR (n = 36) (p = 0.008); being the presence of anxiety in 27.3% (n = 24) of the cases treated with interactive Virtual Reality and in 88.9% (n = 32) of the patients with passive Virtual Reality (p = 0.000). The virtual reality is an effective method to reduce pain and anxiety levels in pediatric patients, with the effectiveness of interactive virtual reality and its use in the population aged 7–15 years being greater.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The performance of invasive procedures, both diagnostic and therapeutic in pediatric patients in the hospital environment is very frequent—with venipuncture and intravascular cannulation techniques being predominant (Cardozo Rodrígez and Escobar Valdivia 2020). These techniques cause pain in children (Krauss et al. 2016; Toledo del Castillo et al. 2019) and even generate situations of stress and anxiety, both in the patient and their carers (Ali et al. 2015; Bradford et al. 2019; Eijlers et al. 2019).
Both pain and anxiety are biological phenomena conditioned by psychological and environmental factors. Some of these factors are: age (Figueroa Jaramillo 2015; Hedén et al. 2020), gender and the patient's personal circumstances and surroundings (Berke et al. 2017; Filingim 2017; Sorge and Totsch 2017). Other clearly linked factors are the behavior of parents or guardians (Casanovas 2017; Harding et al. 2019; Krauss et al. 2016), and the behavior of the professionals who assist them (Ferraz-Torres et al. 2021; Krauss et al. 2016; Svendsen et al. 2016). Accordingly, the level of anxiety experienced by both children and parents during the procedure can also cause stress and / or anguish in health professionals (Ali et al. 2015), constraining their performance and the development of the technique or procedure (Santos et al. 2020).
Therefore, in recent decades, efforts have been made to evaluate and develop mitigating strategies for both pain and anxiety of patients during the performance of frequently used techniques, such as venipuncture and intravascular cannulation techniques. These measures include different types of interventions, such as pharmacological (Krauss et al. 2016), physical such as cold or vibration (Ballard et al. 2019) and psychological such as distraction, cognitive-behavioral therapy or hypnosis (Birnie et al. 2018; Taddio et al. 2010). Several studies focused on the assessment of its implementation as a distraction technique have demonstrated their effectiveness (Díaz-Rodríguez et al. 2021; Özalp Gerçeker et al. 2020; Piskorz and Czub 2018).
Drug administration for the control of acute and short lasted pain, produced by the venipuncture technique, can be effective regardless of the administration route (topical or intravenous). Although it can be an interesting resource, its impact on anxiety control is limited (Krauss et al. 2016). The use of physical measures such as cold application or the Buzzy® device (vibrating box with optional cold feeling) has shown uncertain results. Although it seems to be an optimal alternative for reducing the level of pain experienced during the technique, physical measures do not have effects on stress and anxiety experienced before and during the procedure (Ballard et al. 2019).
Distraction techniques such as hypnosis, combined Cognitive Behavioral Therapy (CBT), or respiratory therapies have demonstrated benefits in reducing pain and anxiety levels for invasive procedures (Birnie et al. 2018). However, they have not proven to be effective on stress and anxiety levels experienced by both the patient and the family members in the moments prior to performing the invasive technique (Birnie et al. 2018). Therefore, these studies show that pediatric patients undergoing venipuncture and catheterization perceive a reduction in pain levels but effectiveness in anxiety levels is limited (Álvarez García et al. 2017; Martín Valbuena et al. 2019; Toledo del Castillo et al. 2019).
More recently, other distraction measures such as the use of virtual reality devices have been shown their effectiveness and safety for this type of invasive procedures (Ahmadpour et al. 2019; Atzori et al. 2018; Eijlers et al. 2019; Lier et al. 2020), as well as for the reduction in anxiety levels both during the procedure (Toledo del Castillo et al. 2019) and prior to it. They are an appealing alternative thanks to their immersive features (Gold and Mahrer 2018). This technology can be applied in two different modes: passive (no user interaction through games) or interactive (combination of virtual reality games with user participation). However, the existing evidence has not assessed the variation in anxiety levels according to the type. Furthermore, few studies analyze the global impact on the level of satisfaction and anxiety experienced by parents and children during these techniques with the use of virtual reality (Han et al. 2019).
Regarding the use of measures to reduce pain and anxiety in pediatric children during invasive techniques, it should be noted that emergency and primary care services do not routinely implement or evaluate any of the existing measures (Benini et al. 2020; Rodríguez et al. 2016), being areas where this type of procedures are performed frequently. Some of the possible causes may be the uncertainty about the effectiveness of the measures to be implemented, as well as the time constraints, the difficulty of the technique, their potential cost and the absence of protocols that allow professionals to implement and evaluate these measures (Rodríguez et al. 2016).
Another aspect linked to anxiety levels experienced during the procedure is the time required to perform the technique. It is worth mentioning that the profile of the pediatric and preschool patient can be considered as a patient typology with difficult vascular access. Thus, the characteristics of these patients are related to the increase in the number of puncture attempts (18.1%) (Gerçeker et al. 2018) and the duration of the procedure. This aspect also conditions pain and anxiety levels experienced by pediatric patients (Ferraz-Torres et al. 2021; Gerçeker et al. 2018). Therefore, in order to reduce the number of punctures and the length of time, the following resources have been identified to be effective: the use of vascular access visualization devices such as infrared devices (Galván Guzmán and Chacon Yance 2019) the ultrasound-guided approach or via ultrasound (Attie et al. 2019; Mayordomo-Colunga et al. 2019; Oulego-Erroz et al. 2021; Sallam et al. 2018). However, this kind of resources are underused at times (Elkhunovich et al. 2017).
Against this background, an intervention protocol was developed, called the ReVi Technique, which allows the standardization of the combined use of ultrasound devices/infrared devices and Virtual Reality when performing phlebotomy procedures (including venipuncture and intravascular cannulation) in pediatric patients. The main objective of this study was to compare the effectiveness of the use of passive and interactive Virtual Reality through the implementation of the ReVi technique protocol (combination of virtual reality and the use of blood vessels viewer device) on reducing patients’ pain anxiety as well as its influence on the experience of the accompanying father or mother and the health care professional involved.
2 Methods
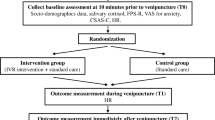
2.1 Study design
A quasi-experimental study was designed with two groups of pediatric patients undergoing venipuncture for blood extraction or venous cannulation who attended the pediatric hospital emergency service of the Hospital Universitario de Navarra (HUN), the reference hospital center of the Autonomous Community of Navarra, in the north of Spain.
We followed the TREND statement specifically developed to guide standardized reporting of nonrandomized controlled trials (Guidelines for Transparent Reporting of Evaluations with Nonrandomized Designs.
2.2 Sample and recruitment
Sample size calculation was carried out with the help of the Epitable software, establishing as analysis criteria a type I error (α) of 0.10 and a power of 99% (error β = 0.01); accounting for an estimated population of 500 patients. A representative sample of 126 patients was calculated; of which two were eliminated for the analysis of the data due to their subsequent rejection to participate.
Distribution of sample participants for both groups was made in a randomized way, marked by the patient's own choice according to the ability to handle the stick or command for the dynamics of the game.
Finally, the sample comprised 124 participants, from which 88 were part of the ReVi Technique program through the use of interactive VR and 36 with passive VR. Data collection was carried out from December 1, 2019 to March 1, 2020.
The inclusion criteria in the study were: pediatric patients with an age range between 2 and 15 years inclusive, subjected to venipuncture (blood extraction or vascular cannulation) not in a vital emergency situation (inclusion of severity in MAT-SET triage with categorization 2–5) and whose parents or guardians agreed to participate in the study. The exclusion criteria were: facial impairment and limited visual acuity.
2.3 Intervention
In both groups, the procedure was performed following the ReVi Technique protocol, which indicated the use of a vein visualizer using ultrasound or infrared detector (at the choice of the nurse performing the procedure), in combination with the use of virtual reality glasses as a distraction mechanism for the children.
The visual distraction system chosen was virtual reality as the more immersive element compared to augmented reality since it allows eliminating the child's real visual field where the anxiety and pain-generating stimulus (the needle or catheter) is found.
Within the use of virtual reality (with the Oculus Go device), two intervention groups were developed. In one of them participants used passive VR, with a designed VR presentation showing a sequence of four short scenes (80 second per scene) with various nature landscape environments, animals and with audio stimulation with different animals sound, with total of 3.20 minutes long and sequential repetitions (Figs. 1, 2, 3, 4).
These videos are made with dynamic scenes and clear images with the incorporation of environmental sounds and animals visualized in the environment to improve immersion in both groups.
Participants in the other group used interactive VR, based on the same visual resource but including four simple interactive games (creating a constellation by joining stars with a laser arrow, building a dolmen by joining rocks, developing a puzzle in the desert and hunting for moles in the forest) to be played by the user with a stick or controller (Figs. 5, 6). The allocation of the participants in the two groups was random marked sometimes conditioned by the young age of the patient and the ability to use the stick and follow-up in the game.
2.4 Measures
Data were collected on the children's age, gender, presence of a companion, the type of vein viewer device (infrared or ultrasound-guided) and the type of venous approach (blood extraction or vascular cannulation). Pain was measured using the visual analogical scale with facial drawings, the Wong-Baker Faces Pain Scale (Miró et al. 2005; Naegeli et al. 2018). It consists of six drawn faces with a score of 0, 2, 4, 6, 8, 10, ranging from a smiling face for no pain (0 points) to a crying face for the worst possible pain (10 points). The standardized FLACC scale: Face, Leg, Activity, Cry and Consolability (Hummel et al. 2010; Manworren and Hyan 2003) was used to measure pain in minor or non-cooperative patients. On this scale, five aspects are measured; facial expression, legs mobility, the activity, crying and the capacity of comforting the child. Each of these criteria is valued between 0, 1 and 2, so the total score of the scale varies between 0 and 10. These scores were interpreted as: 0 = relaxed and comfortable, 1–3 = mild discomfort, 4–6 = moderate pain, 7–10 = severe discomfort/pain. Cronbach's alpha coefficient (α) to measure the reliability of the scale was α = 0.882 (Voepel-Lewis et al. 2010).
To measure anxiety levels of pediatric patients and their parents, the PACBIS (Perioperative Adult and Child Behavioral Interaction Scale) was used, a method selected for its great validity and high level of specificity for detecting stress in pediatric patients (Sadhasivam et al. 2010). This scale offers four dimensions referring to the most characteristic observable behaviors in the child or in the parents: the child's anxiety, evaluated with the child stress subscale (Child distress); and how the child copes, evaluated with the child coping subscale (Child coping).Parental attitudes that promote child stress are assessed with the parent's behavior subscale, defined as reactive or blocking (Negative Parent), and parental attitudes that promote the child coping are assessed with the parent's behavior subscale: defined as proactive or collaborative (Positive Parent). Each dimension scores 0, 1 or 2, with higher scores suggesting maladaptive psychological states or behaviors (Sadhasivam et al. 2010).
The level of anxiety experienced by the professional during the performance of the technique was assessed with an ad hoc question, using a numerical record from zero, indicative of the absence of anxiety, and 10, interpreted as an extreme anxiety level. Likewise, the main advantages and disadvantages detected by health professionals during the use of the ReVi technique were included as a free text field.
To conclude, the number of canalization attempts was determined, collecting this data at the time of the procedure by the nurse. As well as the duration of the procedure, also evaluated by the nurse performing the procedure with the help of a chronometer, starting the measurement when the compressor was placed on the child's arm and ending when the PVC fixation dressing or an adhesive dressing after blood collection was placed. Time was recorded in seconds.
2.5 Data collection
Patient assessment-related data were collected by two nursing professionals trained in the ReVi technique implementation protocol over a period of six months; after completing the first phase of the project (Ferraz-Torres et al. 2021).
Four nurses trained were responsible for carrying out the procedure with the ReVi technique and simultaneously recording the variables. This recording did not interfere during the procedure to ensure an impartial and systematic data collection.
2.6 Statistical analyses
In the first instance, a descriptive analysis of the variables under study was conducted, using the mean and standard deviation (SD) in the case of variables of a quantitative nature and the frequency and percentage in the case of variables of a qualitative nature. Subsequently, the inferential analysis was carried out. First, the homogeneity of the groups was verified by applying the Student's t test to compare two means, in the case of age, time and pain, and the Chi-square test to compare gender, the presence of a carer and the type of venipuncture approach. Second, the outcome variables between the two groups were compared, using multiple linear regression in the case of quantitative variables (time spent and pain) and multiple logistic regression in the case of dichotomous variables (children and parents’ anxiety and health worker’s anxiety). In both cases, the dependent variable was the outcome variable, the group (interactive VR/passive VR) was the independent variable, and age was the control variable. The age was the only variable that did not demonstrate homogeneity between the two groups. In all regressions, the “intro” method was used to introduce the variables to the model. Statistical significance has been set at 0.05. All the analysis was conducted with the statistical software program SPSS v. 25.
2.7 Ethical considerations
The study was approved by the Navarra Clinical Research Ethics Committee (Pyto 2018/52). Legal guardians and school-age pediatric patients were informed verbally and in writing; accepting their free participation in the study and signing the corresponding informed consent.
3 Results
Out of the 124 pediatric patients participating in the study, 51.6% (n = 64) were girls and 48.4% (n = 60) were boys (p = 0.574). The average age of the pediatric patients was 8.4 years (SD: 4.1). In all cases (100%) the patients were accompanied (father or mother) during the procedure.
Among the total number of phlebotomies, 87.1% (n = 108) were performed for venous access cannulation, the rest for venipuncture. The access approach was visualized through the use of ultrasound in 77.4% (n = 96) of the cases and in the remaining 22.6% (n = 28) the infrared external path visualization system was used.
Table 1 shows these characteristics in the interactive VR group and in the passive VR group, with the corresponding p value of the comparison test for both groups.
Regarding the variables of interest, 100% of the punctures were performed in a single attempt. The average duration of the procedure was 5 minutes and 16 seconds. Table 2 shows the results of both groups for these two variables and for the rest of the outcome variables: pain and the level of anxiety experienced by the users and staff involved.
The average level of pain experienced by users and measured with the Wong-Backer/FLACC scale was 2.33 (SD: 0.76) in the interactive VR group (n = 88) compared to 2.67 (SD: 1.35) in patients with passive VR (n = 36) (p = 0.008).
The level of pain experienced by the pediatric patient was similar for both procedures (venipuncture or vascular cannulation); the maximum level of pain expressed and measured using the FLACC or Wong-Backer scale being 4/10 in 18.5% (20) of the canalizations and 2/10 in 16.5% (3) (p = 0.000)
Likewise, the presence of anxiety in pediatric patients, that is, those rated 1 or 2 in the Child distress dimension, took place in 27.3% (n = 24) of the cases treated with interactive VR and in 88.9% (n = 32) of patients with passive VR (p = 0.00) (Table 2).
Depending on the type of procedure performed, a variation is observed in the level of anxiety experienced. Venipuncture did not register the presence of anxiety for items 1 and 2 of the PACBIS scale (0/2), with the presence of a mean level of anxiety 1/2 in 51.9% (56) of patients the cases (p = 0.000).
The study of the paternal and maternal response using the PACBIS scale identified that 22.7% n = (20) of the parents in the interactive VR group and 88.9% (n = 32) of the passive VR group presented a blocking response to the situation (with scores of 1 or 2 in the Negative Parent dimension).
Correspondingly, the analysis of stress or anxiety experienced by the health care professionals responsible for the procedure revealed its presence, that is, with a score equal to 1 or higher, in 22.7% (n = 20) of the cases with Interactive VR and 77.8% (n = 28) with passive VR (Table 2).
The collection of information in the free text field identified key elements such as: the facilitating response of the parents and the calm and passive attitude of the patients as optimal points of the use of virtual reality allowing reducing their anxiety and stress levels during the performance of the technique.
The results of the regressions carried out to compare both groups, in relation to the variables of interest and taking into account the control of the variable “age” are shown in Table 3. As seen in Table 3, there is only a difference between both groups in relation to the variable “time used,” meaning that for the children using interactive virtual reality, the nurses have spent 20 seconds less (0.326 minutes) in performing the blood extraction or cannulation technique vascular (p < 0.01).
Finally, regarding the duration of the technique according to the type of virtual reality used, a significant reduction in the time used in the ReVi technique with interactive virtual reality was detected (mode of 4 minutes, p = 0.00); depending this value on the age of the user (p = 0.00) and the type of venipuncture (blood extraction and / or vascular cannulation; p = 0.00).
4 Discussion
In this clinical study, the protocol called ReVi Technique was designed, which consisted of the combined use of vein visualization devices (infrared or ultrasound) to facilitate and ensure the correct vascular approach in the pediatric patient through direct visualization of the vascular path and the use of virtual reality (interactive or passive) for user distraction.
The development of the ReVi Technique aimed to improve the quality of the technique performed by reducing pain and anxiety experienced by the pediatric patient. In addition, in the study the effectiveness of this technique on improving the experience of the child's companions and the healthcare professionals involved was assessed. Likewise, the implementation of the ReVi Technique through the use of two types of Virtual Reality interactive and passive, allowed evaluating their effectiveness, according to the results in relation to the levels of pain and anxiety experienced by the participants during the performance of these techniques.
Based on the results presented, it is observed that of the vein visualization devices proposed by the ReVi Technique, most of the nurses 77.4% (n = 96) preferred the use of ultrasound. Literature suggests that the use of this technology for the venous approach is beneficial for nurses, highlighting the reduction in the number of attempts, the duration of the technique and patient discomfort as main advantages (Smith 2018).
In the present study, we observed a clear improvement with respect to the levels described by other studies that analyze the pain and the anxiety experienced by the patient during the venipuncture technique (Kleidon et al. 2020; Lee et al. 2020) thanks to the use of virtual reality as distraction techniques; as well as a clear variation of the results according to the type of distraction technique used.
Likewise, we have observed a clearer benefit in the use of VR over the venous cannulation procedure, a technique that presents a greater degree of pain and anxiety experienced by pediatric patients.
According to studies using physical measures (Ballard et al. 2019) and psychological resources (Birnie et al. 2018; Taddio et al. 2010) as a means of distraction and in order to reduce the levels of pain experienced during invasive techniques such as venipuncture in pediatric patients, an improvement in the results was detected, reducing the user's pain levels (Piskorz and Czub 2018). In our study, the comparative analysis regarding the type of VR used shows low levels of pain, recognized as mild for both study groups, and with significant differences according to the group to which they belong; detecting a lower level of pain in the use of interactive VR compared to passive VR.
In the study of anxiety levels expressed by pediatric patients who used the ReVi Technique procedure for blood collection, a clear reduction in their level was shown, compared to other studies (Gold et al. 2021; Han et al. 2019). According to the type of the technique used, the level of anxiety experienced by the child and measured by the PACBIS scale through the use of interactive virtual reality was significantly lower compared to passive VR (Figueroa Jaramillo, 2015; Hedén et al. 2020).
The analysis of the response of the family member accompanying the child during the invasive procedure, clear improvements were observed in the reactivity of the parent through the use of these techniques as a distraction method, allowing to reduce both the levels of blocking and negative response of the family members during the procedure; results similar to other studies showing the effectiveness of the use of distraction techniques as a mechanism to reduce the stress of accompanying family members (Casanovas 2017; Ferraz-Torres et al. 2021; Harding et al. 2019; Krauss et al. 2016).
Concerning the level of anxiety or stress experienced by the health care professionals responsible for performing venipuncture using the ReVi Technique, minimal levels of anxiety were observed. Furthermore, the health care professionals involved in the use of this new procedure showed a high level of satisfaction during the puncture thanks to the implementation of distraction techniques in the pediatric patient.
Our study complements these results by providing information on the key points detected for this improvement, which were the calm attitude of the patient and the positive response of the parents during the technique.
The level of anxiety experienced by the healthcare professionals during the procedure was lower in the intervention group with the interactive technique, which would allow us to conclude that it is the most effective technique for reducing the level of anxiety and pain of the pediatric patient and the most satisfactory and comfortable for the professionals and its use in this type of unit.
The present study provides new knowledge about the experience of healthcare professionals, an aspect that has been little researched but which is nevertheless of great interest since knowledge of the effect of its use allows favoring an effective and permanent implementation of the procedure; improving the quality of the intervention (Ali et al. 2015; Santos et al. 2020).
Another interesting outcome of this study focuses on the correlational analysis performed using the age covariate as a possible determining factor and marker of the type of virtual reality used. Thus, it was detected that both the level of anxiety experienced by the pediatric patient (p = 0.719), the negative reactivity of the parents (p = 0.216) and the anxiety of the healthcare professional involved in performing the technique (p = 0.586) are directly related to the age of the user (p < 0.01).
Our study detects a better adaptation to VR in older patients; allowing a better response in reducing the level of pain and anxiety in patients over 6 years of age; an aspect possibly conditioned by the greater psycho emotional maturity of the patient or which may be conditioned by the greater level of distraction generated by the interactive technique, allowing a greater immersion situation in the user and therefore greater distraction. However, this age factor should be analyzed in greater depth in other studies in which the sample of the pediatric population allows to group its results by ratios of young and advanced age; allowing to deduce what is the optimal age from which interactive VR can be used and thus be able to compare its effectiveness against passive VR without the age cofactor being determinant.
5 Conclusions
There is a clear benefit in the use of VR as a distraction method, being effective the use of two modes of Virtual Reality (passive vs. interactive) as a measure of pain and anxiety reduction in pediatric patients and their parents.
Our study detected a majority use of passive VR in children aged 2 to 6 years; with the conclusion that age this is a conditioning factor for the use of interactive VR. This point should be analyzed in greater depth, allowing to know the adaptation of children of younger age on the use of interactive VR. The implementation of visual resources such as ultrasound or infrared in the vascular access of the pediatric patient is appropriate to reduce the number of punctures, being more comfortable and effective for health professionals the use of ultrasound.
A greater reduction in the level of pain and anxiety in the pediatric patient is detected with the use of interactive VR; an aspect that may indicate a higher level of distraction thanks to the interaction with the game. This benefit should be further studied allowing the comparison of both techniques in the oldest age group.
The use of virtual reality devices as a distraction method generates a reduction in the negative response of the accompanying parents, improving the experience of the procedure for the pediatric patient, especially in patients undergoing venous cannulation.
The level of stress and anxiety expressed by the health care professional responsible for the technique is minimal, expressing a high degree of satisfaction.
References
Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P (2019) Virtual reality interventions for acute and chronic pain management. Int J Biochem Cell Biol 114:105568. https://doi.org/10.1016/j.biocel.2019.105568
Ali S, Mcgrath T, Drendel AL (2015) an evidence-based approach to minimizing acute procedural pain in the emergency department and beyond. Pediatr Emerg Care 32(1):36–42. https://doi.org/10.1097/PEC.0000000000000669
Álvarez García N, Gómez Palacio V, Siles Hinojosa A, Gracia Romero J (2017) Psicoprofilaxis quirurgica audiovisual en cirugía general pediátrica: ¿podemos disminuir la ansiedad del niño y de su familia? Cirugia Pediatrica : Organo Oficial de La Sociedad Espanola de Cirugia Pediatrica 30(4):216–220
Attie GA, Flumignan CDQ, Silva MADM, Barros EDM, Daolio RM, Guedes HJ, Baptista-Silva JCC, Amorim JED, Nakano LCU, Flumignan RLG (2019) What do cochrane systematic reviews say about ultrasound-guided vascular access? Sao Paulo Med J 137:284–291. https://doi.org/10.1590/1516-3180.2019.0113070519
Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, Grotto RL (2018) Virtual reality analgesia during venipuncture in pediatric patients with onco-hematological diseases. Front Psychol 9:1–7. https://doi.org/10.3389/fpsyg.2018.02508
Ballard A, Khadra C, Adler S, Trottier ED, Le May S (2019) Efficacy of the buzzy device for pain management during needle-related procedures: a systematic review and meta-analysis. Clin J Pain 35(6):532–543. https://doi.org/10.1097/AJP.0000000000000690
Benini F, Castagno E, Urbino AF, Fossali E, Mancusi RL, Milani GP (2020) Pain management in children has significantly improved in the Italian emergency departments. Acta Paediatr Int J Paediatr 109(7):1445–1449. https://doi.org/10.1111/apa.15137
Berke DS, Reidy DE, Miller JD, Zeichner A (2017) Take it like a man: Gender-threatened men’s experience of gender role discrepancy, emotion activation, and pain tolerance. Psychol Men Mascul 18(1):62–69. https://doi.org/10.1037/men0000036
Birnie K, Noel M, Chambers C, Uman L, Parker J (2018) Psychological interventions for needle-related procedural pain and distress in children and adolescents: summary of a cochrane review. Cochrane Datab Syst Rev 15(10):75. https://doi.org/10.1016/j.explore.2018.10.014
Bradford JY, Stapleton SJ, Horigan A, Barnason S, Foley A, Johnson M, Kaiser J, Killian M, MacPherson-Dias R, Proehl JA, Reeve NE, Slivinski A, Vanhoy MA, Zaleski ME, Gillespie G, Bishop-Royse J, Wolf L, Delao A, Gates L (2019) Clinical practice guideline: needle-related or minor procedural pain in pediatric patients. J Emerg Nurs 45(4):437.e1-437.e32. https://doi.org/10.1016/j.jen.2019.05.015
Cardozo Rodrígez J, Escobar Valdivia J (2020) Eficacia del uso de la ultrasonografía para el éxtiso del cateterismo periférico en pacientes con acceso venoso difícil. Osteoarthrit Cartil 28(2):1–43
Casanovas JO (2017) Originales 20(5):15–20
Díaz-Rodríguez M, Alcántara-Rubio L, Aguilar-García D, Pérez-Muñoz C, Carretero-Bravo J, Puertas-Cristóbal E (2021) The effect of play on pain and anxiety in children in the field of nursing: a systematic review. J Pediatr Nurs 61:15–22. https://doi.org/10.1016/j.pedn.2021.02.022
Eijlers R, Utens EMWJ, Staals LM, de Nijs PFA, Berghmans JM, Wijnen RMH, Hillegers MHJ, Dierckx B, Legerstee JS (2019) Systematic review and meta-analysis of virtual reality in pediatrics. Anesth Anal 129(5):1. https://doi.org/10.1213/ane.0000000000004165
Elkhunovich M, Barreras J, Pinero VB, Ziv N, Vaiyani A, Mailhot T (2017) The use of ultrasound for peripheral IV placement by vascular access team nurses at a tertiary children’s hospital. J Vasc Access 18(1):57–63. https://doi.org/10.5301/jva.5000615
Ferraz-Torres M, Escalada-Hernandez P, San Martín-Rodriguez L, Delarosa R, Saenz R, Soto-Ruiz M (2021) Predictive factors for anxiety during blood sampling and insertion of peripheral intravenous catheters in paediatric patients in Spain. J Pediatr Nurs. https://doi.org/10.1016/j.pedn.2021.04.009
Figueroa Jaramillo, M. de J. (2015). Modulación emocional con música clásica del dolor y ansiedad asociados a la venopunción en los niños entre 3 y 12 años que acuden al servicio de emergencias del Hospital Metropolitano de Quito de junio a diciembre de 2014 [Pontificia Universidad Católica del Ecuador]. http://repositorio.puce.edu.ec/handle/22000/9164
Filingim R (2017) Sex, gender and pain. In: Legato M (ed) Principles of gender-specific medicine. Academic Press, Cambridge, pp 481–496
Galván Guzmán, E., & Chacon Yance, Y. (2019). Efectividad del uso de dispositivos de imagen vascular infrarrojo y ultrasonido en la canalización de acceso venoso periférico comparado con la técnica tradicional para reducir el número de intentos de punción pacientes pediátricos [Universidad Norbert Wiener]. http://repositorio.uwiener.edu.pe/bitstream/handle/123456789/3496/T061_41686572-001329535_S.pdf?sequence=1&isAllowed=y
Gerçeker GÖ, Ayar D, Özdemir EZ, Bektaş M (2018) The impact of the difficult vascular access, fear, and anxiety level in children on the success of first-time phlebotomy. J Vasc Access 19(6):620–625. https://doi.org/10.1177/1129729818765598
Gold JI, Mahrer NE (2018) Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol 43(3):266–275. https://doi.org/10.1093/jpepsy/jsx129
Gold JI, Annick ET, Lane AS, Ho K, Marty RT, Espinoza JC (2021) “Doc McStuffins: Doctor for a Day” Virtual Reality (DocVR) for pediatric preoperative anxiety and satisfaction: pediatric medical technology feasibility study. J Med Int Res 23(4):1–14. https://doi.org/10.2196/25504
Han SH, Park JW, Choi S. Il, Kim JY, Lee H, Yoo HJ, Ryu JH (2019) Effect of immersive virtual reality education before chest radiography on anxiety and distress among pediatric patients: a randomized clinical trial. JAMA Pediatr 173(11):1026–1031. https://doi.org/10.1001/jamapediatrics.2019.3000
Harding M, Sorkin T, Mccaffery H, Pizzo M (2019) Parental acute stress due to invasive procedures in the pediatric intensive CPCCRN family network collaborative: engaging families in pediatric critical. Critical Care Med 48(1):396. https://doi.org/10.1097/01.ccm.0000631468.53581.17
Hedén L, von Essen L, Ljungman G (2020) Children’s self-reports of fear and pain levels during needle procedures. Nurs Open 7(1):376–382. https://doi.org/10.1002/nop2.399
Hummel P, Lawlor-Klean P, Weiss MG (2010) Validity and reliability of the N-PASS assessment tool with acute pain. J Perinatol 30(7):474–478. https://doi.org/10.1038/jp.2009.185
Kleidon TM, Rickard CM, Schults JA, Mihala G, McBride CA, Rudkin J, Chaseling B, Ullman AJ (2020) Development of a paediatric central venous access device database: a retrospective cohort study of practice evolution and risk factors for device failure. J Paediatr Child Health 56(2):289–297. https://doi.org/10.1111/jpc.14600
Krauss BS, Calligaris L, Green SM, Barbi E (2016) Current concepts in management of pain in children in the emergency department. Lancet 387(10013):83–92. https://doi.org/10.1016/S0140-6736(14)61686-X
Lee SU, Jung JY, Ham EM, Wang SW, Park JW, Hwang S, Kim DK, Kwak YH (2020) Factors associated with difficult intravenous access in the pediatric emergency department. J Vasc Access 21(2):180–185. https://doi.org/10.1177/1129729819865709
Lier EJ, Oosterman JM, Assmann R, de Vries M, van Goor H (2020) The effect of Virtual Reality on evoked potentials following painful electrical stimuli and subjective pain. Sci Rep 10(1):1–8. https://doi.org/10.1038/s41598-020-66035-4
Manworren R, Hyan L (2003) Clinical validation of FLACC: preverbal patient pain scale. Pediatr Nurs 29(2):140–146
Martín Valbuena S, Fernández Fernández I, Varela Robla M, Valcárcel Vega I, Gordo Ruiz T, Fernández Fernández J (2019) Eficacia de una intervención enfermera con realidad virtual en urgencias pediátricas: un ensayo clínico aleatorizado. Tiempos de Enfermería y Salud 1(5):32–37
Mayordomo-Colunga J, González-Cortés R, Bravo MC, Martínez-Mas R, Vázquez-Martínez JL, Renter-Valdovinos L, Conlon TW, Nishisaki A, Cabañas F, Bilbao-Sustacha JÁ, Oulego-Erroz I (2019) Point-of-care ultrasound: Is it time to include it in the paediatric specialist training program? Anales de Pediatria 91(3):206.e1-206.e13. https://doi.org/10.1016/j.anpedi.2019.06.012
Miró J, Huguet A, Nieto R, Paredes S, Baos J (2005) Valoración de la escala de dolor de caras-revisada (faces pain scale-revised) para evaluar la intensidad del dolor pediátrico en niños castellano parlantes. Revista de La Sociedad Espanola Del Dolor 12(7):407–416
Naegeli AN, Hanlon J, Gries KS, Safikhani S, Ryden A, Patel M, Crescioni M, Vernon M (2018) Literature review to characterize the empirical basis for response scale selection in pediatric populations. J Patient Rep Outcomes. https://doi.org/10.1186/s41687-018-0051-8
Oulego-Erroz I, Mayordomo-Colunga J, González-Cortés R, Sánchez-Porras M, Llorente-de la Fuente A, Fernández-de Miguel S, Balaguer-Gargallo M, Frías-Pérez M, Rodríguez-Nuñez A, Santos-Herraiz P, García-Soler P (2021) Ultrasound-guided arterial cannulation or by pulse palpation in the intensive care unit. Anales de Pediatría (English Edition) 94(3):144–152. https://doi.org/10.1016/j.anpedi.2019.12.022
Özalp Gerçeker G, Ayar D, Özdemir EZ, Bektaş M (2020) Effects of virtual reality on pain, fear and anxiety during blood draw in children aged 5–12 years old: a randomised controlled study. J Clin Nurs 29(7–8):1151–1161. https://doi.org/10.1111/jocn.15173
Piskorz J, Czub M (2018) Effectiveness of a virtual reality intervention to minimize pediatric stress and pain intensity during venipuncture. J Spec Pediatr Nurs 23(1):1–6. https://doi.org/10.1111/jspn.12201
Rodríguez MC, Villamor P, Castillo T (2016) Assessment and management of pain in pediatric otolaryngology. Int J Pediatr Otorhinolaryngol 90:138–149. https://doi.org/10.1016/j.ijporl.2016.09.015
Sadhasivam S, Cohen LL, Hosu L, Gorman KL, Wang Y, Nick TG, Jou JF, Samol N, Szabova A, Hagerman N, Hein E, Boat A, Varughese A, Kurth CD, Willging JP, Gunter JB (2010) Real-time assessment of perioperative behaviors in children and parents: development and validation of the perioperative adult child behavioral interaction scale. Anesth Anal 110(4):1109–1115. https://doi.org/10.1213/ANE.0b013e3181d2a509
Sallam K, Refaat A, Romeih M (2018) Ultrasound-guided venous access: “Wire-loaded puncture” technique for paediatric cancer patients. J Egypt Nal Cancer Inst 30(3):99–105. https://doi.org/10.1016/j.jnci.2018.07.001
Santos N, Pérez G, García S, Mintegi S (2020) Procedimientos de sedoanalgesia pediátricos: formación y práctica profesional de los enfermeros en los servicios de urgencias españoles. Emergencias 32(2):143–145
Smith C (2018) Should nurses be trained to use ultrasound for intravenous access to patients with difficult veins? Emerg Nurse 26(2):18–24. https://doi.org/10.7748/en.2018.e1733
Sorge RE, Totsch SK (2017) Sex differences in pain. J Neurosci Res 95(6):1271–1281. https://doi.org/10.1002/jnr.23841
Svendsen EJ, Moen A, Pedersen R, Bjørk IT (2016) Parent-healthcare provider interaction during peripheral vein cannulation with resistive preschool children. J Adv Nurs 72(3):620–630. https://doi.org/10.1111/jan.12852
Taddio A, Appleton M, Bortolussi R, Chambers C, Dubey V, Halperin S, Hanrahan A, Ipp M, Lockett D, MacDonald N, Midmer D, Mousmanis P, Palda V, Pielak K, Riddell RP, Rieder M, Scott J, Shah V (2010) Reducing the pain of childhood vaccination: An evidence-based clinical practice guideline (summary). Cmaj 182(18):1989–1995. https://doi.org/10.1503/cmaj.092048
Toledo del Castillo B, Pérez Torres JA, Morente Sánchez L, Escobar Castellanos M, Escobar Fernández L, González Sánchez MI, Rodríguez Fernández R (2019) Reducing the pain in invasive procedures during paediatric hospital admissions: fiction, reality or virtual reality? Anales de Pediatria 91(2):80–87. https://doi.org/10.1016/j.anpedi.2018.10.019
Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S (2010) Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care 19(1):55–61. https://doi.org/10.4037/ajcc2010624
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research is part of the ReVi project, funded by the “Precipita” crowdfunding platform, from the Spanish Foundation for Science and Technology (FECYT).
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to the preparation of this manuscript following the International Committee of Medical Journal Editors guidelines. Study design was contributed by MFT, LSM, PEH, NSR. Preparation of the manuscript was contributed by LSM, PEH, NSR, MFT, CGV. Editing and final revision of the manuscript were contributed by MFT, LSM, PEH, NSR, CGV. The manuscript has been read and approved by all named authors. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest disclose.
Ethical approval
The research was in accordance with the 1964 Helsinki Declaration and its later amendments ethical standards
Human and animal rights
We further confirm that any aspect of the work covered in this manuscript that has involved human participants has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Informed consent
Informed consent was obtained from all individual participants involved in the study, and their anonymity was preserved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferraz-Torres, M., San Martín-Rodríguez, L., García-Vivar, C. et al. “Passive or interactive virtual reality? The effectiveness for pain and anxiety reduction in pediatric patients”. Virtual Reality 26, 1307–1316 (2022). https://doi.org/10.1007/s10055-022-00633-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10055-022-00633-7