Abstract
The objective of this meta-analysis was to identify the correlation between arterial blood gas (ABG) and venous blood gas (VBG) analysis in patients with acute exacerbation chronic obstructive pulmonary disease (AECOPD). Seven relevant literature entries from PubMed, the Cochrane Library, Google Scholar, and China National Knowledge Infrastructure (CNKI) on 1234 patients were included in the analysis. Variables derived from the investigations, which were presented as mean ± standard deviation (SD) in both ABG and VBG, were converted into mean differences (MDs) (mean ± SD) by subtracting venous values from arterial values. For the purposes of pooling the MDs, 95% confidence intervals (CIs) were required. Stata version 13.0 software was used to perform the statistical analysis. As a result, the pooled MD for the potential of hydrogen (pH) was 0.02 pH units (ABG minus VBG) (95% CI, 0.02–0.03), for partial pressure of carbon dioxide (PCO2) −2.91 mm Hg (95% CI, −4.23 to −1.59), for partial pressure of oxygen (PO2) 13.13 mm Hg (95% CI, 9.13–17.12), and for bicarbonate (HCO3−) −0.22 mmol/l (95% CI, −0.62 to 0.18). In conclusion, VBG analysis compares well with ABG for pH, PCO2, and HCO3 estimations, but not for PO2 in patients with AECOPD.
Zusammenfassung
Ziel dieser Metaanalyse war es, die Korrelation zwischen arteriellen (ABG) und venösen (VBG) Blutgasanalysen bei Patienten mit akuter Exazerbation einer chronisch-obstruktiven Lungenerkrankung (AECOPD) zu bestimmen. Für diese Analyse wurden sieben relevante Berichte aus PubMed, Cochrane Library, Google Scholar und China National Knowledge Infrastructure (CNKI) mit 1234 Patienten herangezogen. Variablen, die aus den berücksichtigten Untersuchungen abgeleitet und als Mittelwert ± Standardabweichung (SD) sowohl in ABG als auch in VBG dargestellt wurden, wurden durch Subtraktion venöser Werte von arteriellen Werten in eine Mittelwertdifferenz (MD; Mittelwert ± SD) transformiert. Für die Zusammenlegung der MD wurden 95 %-Konfidenzintervalle (KI) benötigt. Für die statistische Analyse wurde die Software Stata Version 13.0 genutzt. Der zusammengelegte MD für den pH-Wert betrug 0,02 pH-Einheiten (ABG minus VBG; 95 %-KI 0,02 bis 0,03), für den Kohlendioxidpartialdruck (pCO2) −2,91 mm Hg (95 %-KI −4,23 bis −1,59 mm Hg), für den Sauerstoffpartialdruck (pO2) 13,13 mm Hg (95 %-KI 9,13 bis 17,12 mm Hg) und für HCO3− −0,22 mmol/l (95 %-KI −0,62 bis 0,18 mmol/l). Zusammenfassend lässt sich sagen, dass die VBG-Analyse bei Patienten mit AECOPD gut mit der ABG-Analyse für pH-, pCO2- und HCO3−-Schätzungen verglichen werden kann. Für pO2 gilt dies dagegen nicht.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the heaviest burdens placed on medical institutions, not to mention governments, all over the world [1]. Acute exacerbation of COPD (AECOPD) is defined as a progressive deterioration of ventilatory function in patients with COPD, leading to hypoxia and hypercarbia [2]. Arterial blood gas (ABG) is a gold standard to obtain information on the potential of hydrogen (pH), partial pressure of carbon dioxide (PCO2), partial pressure of oxygen (PO2), and bicarbonate (HCO3−) in order to measure the severity AECOPD according to the recommendations of National Institute for Health and Care Excellence (NICE) [3]. However, arterial sampling obtained by puncture biopsy is associated with significant disadvantages, including technical difficulty, pain, infection, thrombosis with distal ischemia, as well as severe subcutaneous hematoma, and repeated arterial puncture biopsy increases the incidence of complications. Alternative solutions for ABG need to be found to lower the cost of assessing and treating AECOPD.
Data from recent studies suggested good agreement between venous blood gas (VBG) and ABG when measuring pH, PCO2, PO2, and HCO3− in patients with diabetic keto-acidosis (DKA), tricyclic overdose, uremia, and emergency department (ED) trauma [4, 5]. Simultaneously, VBG has also been reported in recent studies as an alternative to ABG for monitoring during AECOPD treatment [3, 6,7,8,9,10,11,12,13].
The objective of this study was to perform a meta-analysis of the reported literature entries related to the agreement of parameters pH, PCO2, PO2, and HCO3− between VBG and ABG to determine whether they are comparable, in order to verify the feasibility of replacing ABG with VBG in patients with AECOPD.
Methods
Search strategy
A general search for English-language literature was performed in the following databases: PubMed, Cochrane Library, Google Scholar, and China National Knowledge Infrastructure (CNKI). The date of the last search was February 22 2017. The definite words applied during the search in English included: “venous blood gas,” “arterial blood gas,” “VBG,” “ABG,” “chronic obstructive pulmonary disease,” “chronic obstruction pulmonary disease,” “COPD,” “pH,” “PCO2,” “PO2,” “HCO3−” in the titles or abstracts. The references listed below the articles searched were scanned and selected for inclusion in the meta-analysis.
Inclusion and exclusion criteria
Case-control studies comparing ABG and VBG in patients with COPD in which sample size, study population, criteria for patient selection, and type of blood gas analyzer used for the analysis were included. Searches that reported mean and standard deviation (SD) of paired pH, PCO2, PO2, or HCO3− for peripheral venous and arterial blood samples were included. Case studies and research on animals were excluded. Studies in which venous samples were obtained via central venous access were also excluded.
Data extraction
The basic characteristics of searches, including first author names, publication year, patient cases, and paired variables, i.e., pH, PCO2, PO2, or HCO3− (mean ± SD), were extracted. Full texts and supplementary material from selected literature were reviewed for the extraction of available data. The meta-analysis was carried out according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses report (PRISMA). Data analysis, including study searches, article selection, and data extraction was performed by two independent researchers; any disagreements were discussed and solutions sought.
Statistical analysis
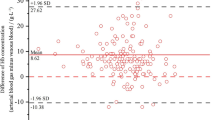
In the present study, the variables derived from the included investigations, which were presented as mean ± SD in both ABG and VBG, were converted into mean differences (mean ± SD) by subtracting venous values from arterial values. For the purposes of pooling the mean differences (MDs), 95% confidence intervals (CIs) were required. In cases in which 95% CIs were not provided in the selected studies, these were calculated from the given MDs. CIs for a mean are a function of the standard error of mean (SEM), which is the SD divided by the square root of the case sample; 95% limits of agreement (LOA) is the range of the mean plus or minus the SD multiplied by 2. Therefore, CIs are necessarily narrower than the LOA. The data obtained from texts directly or calculated with the given variable were combined for MDs.
Tests for ABG and VBG, including pH, PCO2, PO2, and HCO3−, were considered comparable if the average bias was less than the error defined by standard laboratory performance criteria: pH ±0.04, PCO2 ±5 mm Hg, and PO2 ±7 mm Hg [14].
The Higgins I2-test was used as a heterogeneity test to detect heterogeneity of the included data, whereby: I2 = 0 meant no heterogeneity; I2 < 50% meant mild heterogeneity; 50% < I2 < 75% meant moderate heterogeneity; I2 > 50% meant high heterogeneity [15]; and I2 reflects the proportion of the part of heterogeneity among the total variation of effect size. The formula is I2 = 100% × (Q −df) / Q, where Q means statistics and df means degrees of freedom. In the case of I2 < 50%, a fixed effects meta-analysis was used. In the case of I2 ≥ 50%, a random effects meta-analysis was performed. The meta-analysis was performed using the package Metan running in Stata software version 13.0.
Results
Search results
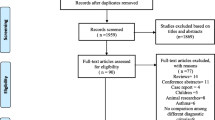
According to the PRISMA diagram shown in Fig. 1, 568 literature entries were obtained from PubMed (n = 447) and other sources (n = 121), including the Cochrane Library, Google Scholar, and CNKI. After the deletion of duplicates, there were 514 remaining results, of which 52 literature entries were selected according to titles. By limiting selection to studies on COPD, seven studies with 1234 patients were included in the final analysis (Ak et al. 2006, McCanny et al. 2012, McKeever et al. 2016, Novovic et al. 2012, Raoufy et al. 2011, Razi et al. 2007, Sadariya et al. 2014).
All studies included were on the comparison between ABG and VBG in patients with COPD. Study characteristics are listed in Table 1.
Comparisons
The pooled MD for pH was 0.02 pH units (ABG minus VBG) (95% CI, 0.02–0.03), for PCO2 −2.91 mm Hg (95% CI, −4.23 to −1.59), for PO2 13.13 mm Hg (95% CI, 9.13 to 17.12), and for HCO3− −0.22 mmol/l (95% CI, −0.62 to 0.18) (Figs. 2, 3, 4, and 5).
Discussion
As a result of the present study, the pooled MD for pH was 0.02 pH units (ABG minus VBG) (95% CI, 0.02−0.03), for PCO2 −2.91 mm Hg (95% CI, −4.23 to −1.59), for PO2 13.13 mm Hg (95% CI, 9.13−17.12), and for HCO3− −0.22 mmol/l (95% CI, −0.62 to 0.18). According to the error defined by standard laboratory performance criteria [14], whereby pH is ±0.04, PCO2 ±5 mm Hg, and PO2 ±7 mm Hg, the data above suggested that they might compare well between ABG and VBG for pH, PCO2, but not for PO2. In addition, HCO3− is a derived value of pH and PCO2 using the Henderson-Hasselbalch equation. Thus, HCO3− of VBG might also compare well to that of ABG.
Data from a prospective trial have revealed that there was a significant correlation between ABG and VBG values for pH, PCO2, and HCO3− (p < 0.001) with the Pearson correlation coefficients, respectively [6], which was further verified by other investigations [3, 8, 9, 12]. Although PO2 showed poor correlation between VBG and ABG in the present analysis [11], it has been reported that, when using VBG values, the designed artificial neural networks (ANN), a non-linear mode, was able to predict all ABG values (even PO2 and O2 saturation) by regression equations such as arterial PO2 = 26.651 + 0.694 × venous PO2; and arterial O2 saturation = 64.724 + 0.297 × venous O2 saturation in AECOPD patients [11]. In the authors’ view, ANNs have the added advantage that they can learn to predict arbitrarily complex nonlinear relationships between independent and dependent variables by including more processing elements in the hidden layer or more hidden layers, which make the ANN a more robust paradigm for application in a real-world setting [16]. In this way, ABG values could be calculated using specific formula from VBG by ANNs, thereby avoiding the puncture biopsy complications associated with ABG.
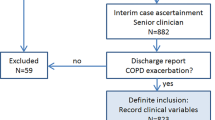
The ability to detect hypoxemia hypercapnia (arterial PCO2 > 50 mm Hg) in COPD patients is of crucial importance, since it provides the opportunity for earlier intervention to treat respiratory failure [17]. Given the associated relationship between pH and PCO2 and good agreement between VBG and ABG, a trend of peripheral venous pH and HCO3− could potentially be used to follow the trend of respiratory acidosis [18]. Clinically, an unanticipated HCO3− value with acidosis in patients with COPD should prompt the physician to search for other underlying diseases causing metabolic acidosis, such as lactic acidosis from septic shock or uremia [19]. Hence, the authors suggest an algorithm for the management of COPD exacerbations in clinical practice (Fig. 6). However, in terms of this meta-analysis, the majority of suggestions in Fig. 6 were based on data from the studies included, which might be less specific and intended merely as a guide for clinicians.
Suggested algorithm for blood gas analysis during chronic obstructive pulmonary disease (COPD) exacerbation. AECOPD acute exacerbation of chronic obstructive pulmonary disease, ABG arterial blood gas, VBG venous blood gas, pH potential of hydrogen, PCO2 partial pressure of carbon dioxide, HCO3 bicarbonate, SPO2 peripheral capillary oxygen saturation
Previous studies, including systematic reviews and meta-analyses, that compared peripheral VBG and ABG analysis in emergency department patients showed that venous and arterial pH agree reasonably well for all values, but the agreement is highest for normal values. In addition, arteriovenous agreement for PCO2 and HCO3− is poor [5]; no sub-group analysis was performed for cases involving patients with, e.g., diabetic keto-acidosis (DKA), tricyclic overdose, or uremia. Another study showed that VBG compares well with ABG analysis for pH estimations in adults, but not for PCO2 or PO2 in emergency department patients [4]. It was revealed that venous PCO2 cannot be used to predict arterial PCO2 by applying a ‘correction factor.’ Another investigation reported that the VBG might be useful in determining whether venous blood has a low amount of CO2 and high O2 to exclude hypercapnia and hypoxia [20]. Likewise, the systematic review of estimates of differences between VBG and ABG was subject to a high degree of heterogeneity, which might lead to a further bias. Whatever the case, pH was assumed to be comparable between VBG and ABG whether or not in AECOPD patients.
One of the most obvious limitations of the present meta-analysis is that all cases in the included literature entries presented with stable hemodynamics and normal blood pressure. According to earlier studies, there is poor agreement for pH, PCO2, and HCO3− in patients with shock or unstable hemoperfusion [21], which gave rise to uncertainties about the correlation in COPD patients with circulatory failure or shock. In addition, the authors tried but failed to specify the relevant coefficient of parameters, including pH, PCO2, or HCO3−, between ABG and VBG, which represents another limitation of this study.
In conclusion, VBG analysis compares well with ABG for pH, PCO2, and HCO3− estimations, but not for PO2 in patients with AECOPD.
References
Hurd S. The impact of COPD on lung health worldwide: epidemiology and incidence[J]. Chest, 2000, 117(2 Suppl): 1S–4S.
Agusti AG, Barbera JA (1994) Contribution of multiple inert gas elimination technique to pulmonary medicine. 2. Chronic pulmonary diseases: chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis[J. Thorax 49(9):924–932
Mckeever TM, Hearson G, Housley G et al (2016) Using venous blood gas analysis in the assessment of COPD exacerbations: a prospective cohort study[J. Thorax 71(3):210–215
Byrne AL, Bennett M, Chatterji R et al (2014) Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis[J. Respirology 19(2):168–175
Bloom BM, Grundlingh J, Bestwick JP et al (2014) The role of venous blood gas in the emergency department: a systematic review and meta-analysis[J. Eur J Emerg Med 21(2):81–88
Ak A, Ogun CO, Bayir A et al (2006) Prediction of arterial blood gas values from venous blood gas values in patients with acute exacerbation of chronic obstructive pulmonary disease[J. Tohoku J Exp Med 210(4):285–290
Kelly AM, Kerr D, Middleton P (2005) Validation of venous pCO2 to screen for arterial hypercarbia in patients with chronic obstructive airways disease[J. J Emerg Med 28(4):377–379
Mccanny P, Bennett K, Staunton P et al (2012) Venous vs arterial blood gases in the assessment of patients presenting with an exacerbation of chronic obstructive pulmonary disease[J. Am J Emerg Med 30(6):896–900
Novovic M, Topic V (2012) Correlation between arterial and venous blood gas analysis parameters in patients with acute exacerbation of chronic obstructive pulmonary disease][J. Srp Arh Celok Lek 140(7–8:436–440
O’connor TM, Barry PJ, Jahangir A et al (2011) Comparison of arterial and venous blood gases and the effects of analysis delay and air contamination on arterial samples in patients with chronic obstructive pulmonary disease and healthy controls[J. Respiration 81(1):18–25
Raoufy MR, Eftekhari P, Gharibzadeh S et al (2011) Predicting arterial blood gas values from venous samples in patients with acute exacerbation chronic obstructive pulmonary disease using artificial neural network[J. J Med Syst 35(4):483–488
Razi E, Moosavi GA (2007) Comparison of arterial and venous blood gases analysis in patients with exacerbation of chronic obstructive pulmonary disease[J. Saudi Med J 28(6):862–865
Sadariya Bhavesh R, Sharma H, Maheshwari AV et al (2014) Comparison of venous and arterial blood gases and pH in acute exacerbation of chronic obstructive pulmonary disease—an alternative approach[J. Int J Res Med 3(2):123–126
Medicare, Medicaid and CLIA programs; regulations implementing the Clinical Laboratory Improvement Amendments of 1988 (CLIA) and Clinical Laboratory Improvement Act Program fee collection—HCFA. Final rule with comment period[J]. Fed Regist, 1993, 58(11): 5215–37.
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses[J. BMJ 327(7414):557–560
Lin CS, Li YC, Mok MS et al (2002) Neural network modeling to predict the hypnotic effect of propofol bolus induction[J. Proc Amia Symp 37(4):450
Papala M, Kerenidi N, Gourgoulianis KI (2013) Everyday clinical practice and its relationship to 2010 and 2011 GOLD guideline recommendations for the management of COPD[J. Prim Care Respir J 22(3:362–364
Lim BL, Kelly AM (2010) A meta-analysis on the utility of peripheral venous blood gas analyses in exacerbations of chronic obstructive pulmonary disease in the emergency department[J. Eur J Emerg Med 17(5):246–248
Adrogue H J, Madias N E. Influence of chronic respiratory acid-base disorders on acute CO2 titration curve[J]. J Appl Physiol (1985), 1985, 58(4):1231–8.
Bass CM, Sajed DR, Adedipe AA et al (2015) Pulmonary ultrasound and pulse oximetry versus chest radiography and arterial blood gas analysis for the diagnosis of acute respiratory distress syndrome: a pilot study[J. Crit Care 19(1):282
Toftegaard M, Rees SE, Andreassen S (2008) Correlation between acid-base parameters measured in arterial blood and venous blood sampled peripherally, from vena cavae superior, and from the pulmonary artery[J. Eur J Emerg Med 15(2):86–91
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Bingheng, C. Jianxin, C. Yu and Y. Yijuan declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Chen Jianxin and Lou Bingheng contributed equally to the article and should be considered as co-first author.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bingheng, L., Jianxin, C., Yu, C. et al. Comparison of peripheral venous and arterial blood gas in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD): a meta-analysis. Notfall Rettungsmed 22, 620–627 (2019). https://doi.org/10.1007/s10049-018-0469-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10049-018-0469-9
Keywords
- Hypoxia
- Hypercarbia
- Chronic obstructive pulmonary disease
- Transcutaneous blood gas monitoring
- Puncture biopsy