Abstract
Liver abscess remains a life-threatening disease, particularly when it results in systemic organ failure necessitating intensive care. Only few cases of respiratory failure caused by liver abscess and treated with veno-venous extracorporeal membrane oxygenation (ECMO) have been reported. Here we present a case of liver abscess with rapid progression of multiple organ dysfunction, including severe acute respiratory failure on admission to the intensive care unit (ICU). Upon admission, we immediately initiated artificial organ support systems, including ventilator, continuous renal replacement therapy, and cardiovascular drug infusion for septic multiple organ failure and source control. Despite this initial management, respiratory failure deteriorated and V-V ECMO was introduced. The case developed abdominal compartment syndrome, for which we performed a bedside decompressive laparotomy in the ICU. The case gradually recovered from multiple organ failure and was discharged from the ICU on day 22 and from the hospital on day 53. Since liver abscess is potentially lethal and respiratory failure on admission is an additional risk factor of mortality, V-V ECMO may serve as an adjunctive choice of artificial organ support for cases of severe acute respiratory failure caused by liver abscess.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver abscess remains a life-threatening illness when patients develop organ failure, including circulatory, respiratory, and renal failure, and need intensive care [1, 2]. The clinical symptoms of liver abscess include abdominal pain, fever, and lethargy, and are non-specific and sometimes even asymptomatic. However, liver abscess can rapidly develop into a systemic infection via the liver circulatory system, resulting in a serious and potentially fatal condition [1, 2]. Here we present a case of multiple organ failure, including severe acute respiratory failure, caused by liver abscess and treated with veno-venous extracorporeal membrane oxygenation (ECMO).
Case report
An 80-year-old man was transferred from another hospital to the emergency department of the hospital with rapid progression of multiple organ failure. The case’s medical history included hypertension, hyperuricemia, and atrial fibrillation. He experienced the earliest symptoms of abdominal pain and lethargy 5 days prior to transfer to our hospital. Three days after onset of these initial symptoms, he developed high fever (39 °C) and was initially admitted at another hospital with a suspected infection. He was administered intravenous piperacillin/tazobactam; however, he rapidly developed multiple organ failure and was transferred to our emergency department (ED).
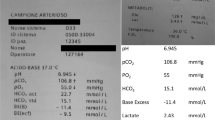
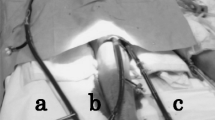
Upon admission to the ED, he had an axillary temperature of 35.2 °C, respiratory rate of 26 breaths per minute, blood pressure (BP) of 61/48 mm Hg, and heart rate (HR) of 102 beats per minute; oxygen saturation was 96 % while breathing 100 % oxygen with a reservoir mask. The Glasgow Coma Scale score was E3V5M6. The abdomen was tender without rigidity. Arterial blood gas analysis showed a pH of 7.287, PO2 of 91.4 mm Hg, PCO2 of 30.7 mm Hg, base excess of −11.0 mmol/L, and blood lactate level of 2.5 mmol/L (Supplementary Table 1). Transthoracic echocardiography revealed that the inferior vena cava was 6 mm with an inspiratory collapse and no impairment of ventricular wall motion. Crystalloid fluid bolus of 30 mL/kg for initial fluid resuscitation of septic shock followed by administration of norepinephrine of 0.2 μg/kg/min elevated the mean arterial pressure over 65 mmHg (BP 125/55, HR 128). Due to circulatory and respiratory failure, endotracheal intubation and mechanical ventilation were subsequently initiated (Fig. 1a). Computed tomography (CT) revealed two gas-forming liver abscesses in segment 6 with portal venous gas (size 17 × 18 × 19 mm, 31 × 25 × 36 mm) (Fig. 1b, c). Laboratory tests revealed bacterial infection, inflammation, coagulopathy, and acute kidney injury (AKI) (Supplementary Table 1). Empiric broad-spectrum antimicrobial therapy using intravenous meropenem was initiated. After the CT scan, he was moved to the ICU at 1.5 h after the ED admission. The sequential organ failure assessment (SOFA) score was 18 and acute physiology and chronic health evaluation (APACHE) II score was 33 on ICU admission.
Upon ICU admission, echocardiographic and hemodynamic monitoring revealed insufficient preload and increased vascular permeability without impairment of ventricular wall motion. Consecutive fluid therapy, vasopressor infusion targeting a mean arterial pressure of 65 mmHg, and acute low-dose corticosteroid therapy for septic shock were performed. The blood lactate level peaked at 30 min after ICU admission (5.1 mmol/L, BP 105/51, HR 125), followed by improvement. Arterial pH, base excess and lactate levels returned to the normal range 18 h after ICU admission (BP 152/89, HR 95) and remained within the normal range during ICU stay. Continuous hemodiafiltration using a polymethylmethacrylate hemofilter for AKI caused by septic shock was initiated 2 h after ICU admission [3]. An ultrasound-guided percutaneous transhepatic drainage abscess tube was successfully inserted 3 h after ICU admission. While the initial management of septic shock improved hemodynamic status, hypoxemia and hypercapnia deteriorated. The PaO2/FIO2 (P/F) ratio decreased from 89 on ICU admission to 67, with an elevated PaCO2 of 96 mmHg 5 h after admission, despite increasing PEEP to 15 cmH2O and switching to airway pressure release ventilation with a P high of 25. The Murray score was 3.5. Therefore, veno-venous extracorporeal membrane oxygenation (VV-ECMO) from the femoral to the jugular vein [right femoral 21Fr (Medtronic); right jugular 13.5Fr (Terumo)] was initiated and maintained with blood flow set at 3.5 L/min [equals to 55 mL/kg/min, (recommended flow range in the ELSO Guidelines [4], 50–80 mL/kg/min)], oxygen flow at 3.5 L/min, the V:Q ratio and FIO2 of the artificial lung at 1.0 (Blood pump, CAPIOX emergency bypass system; artificial lung CAPIOX LX, Terumo). Percutaneous ECMO cannulas were inserted under ultrasound guidance and subsequently cannula positions were confirmed using X-ray. During ECMO, heparin was titrated to maintain the activated clotting time between 180 and 220 s, resulting in no serious bleeding or thrombotic adverse events. Although hypoxemia improved upon VV-ECMO, he had progressive abdominal distension and developed abdominal compartment syndrome (ACS). The intra-abdominal pressure was >20 mmHg, and decompressive laparotomy followed by temporary abdominal vacuum-packing closure was immediately performed 3 h after ECMO initiation in the ICU. Intraoperative finding indicated that peritoneal tissue edema leaded to ACS. After this initial management, the progression of organ failure halted. Peptostreptococcus micros was isolated from the blood, and the abscess aspirated. Multiple organ failure gradually recovered and the patient was weaned off vasopressor infusion on day 4. Subsequently, the patient was weaned off ECMO for severe respiratory failure, and ECMO was stopped on day 8 (Figs. 1d, 2). There was no abnormality observed in ECMO devices after use including blood clotting. CHDF for AKI was terminated on day 15 and he was weaned off and removed from the ventilator on day 21. He was discharged from the ICU to a general ward on day 22 and was discharged for rehabilitation on day 53.
Discussion
Liver abscess is still a life-threatening disease. The associated mortality is high, in particular in critically ill patients admitted to ICU (28 %) [1], compared to hospitalized patients (4–10 %) [1, 2, 5, 6]. It was reported that the size of liver abscess, pathogens, or comorbidities were not associated with the mortality of critically ill patients with liver abscess, whereas non-survivors more frequently had acute respiratory failure, septic shock, and renal failure on the first day of admission to ICU compared to survivors [1]. Furthermore, using a multivariate regression analysis, the same study showed that acute respiratory failure and an APACHE II score >16 were independently associated with increased mortality of liver abscess in ICU [1]. Moreover, two additional studies of liver abscess, which were not limited to the ICU patients, demonstrated that APACHE II scores of >16, septic shock, acute respiratory distress syndrome (ARDS) on admission, development of multiple organ failure, and gas formation were significant predictors of mortality [2, 6]. The present case with a gas-forming liver abscess had septic shock, respiratory failure, renal failure and an APACHE II score of 33 on ICU admission, and, based on these reports, had a substantial risk factors for liver abscess fatality.
The respiratory failure was notably critical in this case and ECMO was required on the first day of ICU admission. Although acute respiratory failure is a risk factor for mortality in liver abscess, ECMO for respiratory failure in liver abscess is rare in general, but a similar case was reported [7]. The subject in that reported case also suffered severe respiratory failure after source control and required potent respiratory support by ventilator for 5 days, resulting in pneumothorax, followed by prolonged ECMO support for 47 days [7]. In our case, ECMO was initiated on the first day of ICU admission and weaned off on day 8 without the need of changing ECMO equipments including larger sized cannulas and extracorporeal circulation devices designed for long-term bypass. Early initiation of ECMO with non-invasive ventilator support may result in early weaning off ECMO. There was a significant improvement of lung in chest X-ray on day 8, including an increase of normal lung area, compared to day 1 (Fig. 1a, d), suggesting that liver abscess might cause a diaphragmatic elevation, abnormal respiratory pattern and increased pulmonary vascular permeability on day 1.
The use of ECMO to treat acute respiratory failure is increasing [8–10]. V-VECMO for adult patients with sepsis-induced acute respiratory failure or pneumonia is not rare, while veno-arterial ECMO for adult patients with refractory septic shock is rare and remains unsatisfactory [11]. In this liver abscess case, acute respiratory failure was mainly caused by pulmonary edema due to an increased vascular permeability, which is called “extrapulmonary” ARDS (also referred to as “secondary” or “indirect” ARDS) [12]. ECMO for extrapulmonary ARDS is not rare, and accounted for 28 % of study subjects in a multicenter randomized controlled trial showing efficacy of ECMO for severe adult respiratory failure [13].
Abdominal compartment syndrome may represent a possible complication with ECMO and the increased permeability may contribute to its occurrence [14, 15]. Decompressive laparotomy is a traditional intervention for abdominal compartment syndrome [16]. Decompression by drained fluid using a peritoneal dialysis catheter was also reported in children with ACS during ECMO[17]. We successfully introduced a rescue bedside laparotomy in the ICU. The bedside decompressive laparotomy may be an appropriate therapy during ECMO in the ICU [18].
To conclude, we reported a case of multiple organ failure, including severe respiratory failure that was treated with V-V ECMO. Since liver abscess is potentially lethal, and as respiratory failure, in particular on admission, is a risk factor for mortality, V-V ECMO may represent an adjunctive choice to avoid fatality in cases of severe acute respiratory failure caused by liver abscess.
References
Chen W, Chen CH, Chiu KL, Lai HC, Liao KF, Ho YJ, Hsu WH. Clinical outcome and prognostic factors of patients with pyogenic liver abscess requiring intensive care. Crit Care Med. 2008;36:1184–8.
Chen CH, Wu SS, Chang HC, Chang YJ. Initial presentations and final outcomes of primary pyogenic liver abscess: a cross-sectional study. BMC Gastroenterol. 2014;14:133.
Nakada TA, Oda S, Matsuda K, Sadahiro T, Nakamura M, Abe R, Hirasawa H. Continuous hemodiafiltration with PMMA hemofilter in the treatment of patients with septic shock. Mol Med. 2008;14:257–63.
Siu LK, Yeh KM, Lin JC, Fung CP, Chang FY. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis. 2012;12:881–7.
Lee SS, Chen YS, Tsai HC, Wann SR, Lin HH, Huang CK, Liu YC. Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis. 2008;47:642–50.
Ko WJ, Hsu HH, Tsai PR. Prolonged extracorporeal membrane oxygenation support for acute respiratory distress syndrome. J Formos Med Assoc. 2006;105:422–6.
Terragni P, Faggiano C, Ranieri VM. Extracorporeal membrane oxygenation in adult patients with acute respiratory distress syndrome. Curr Opin Crit Care. 2014;20:86–91.
Sonoo T, Ohshima K, Kobayashi H, Asada T, Hiruma T, Doi K, Gunshin M, Murakawa T, Anraku M, Nakajima S, Nakajima J, Yahagi N. Acute respiratory distress syndrome (ARDS) treated successfully by venovenous extracorporeal membrane oxygenation (ECMO) in a nearly drowned patient. J Artif Organs. 2014;17:281–4.
Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011;365:1905–14.
Huang CT, Tsai YJ, Tsai PR, Ko WJ. Extracorporeal membrane oxygenation resuscitation in adult patients with refractory septic shock. J Thorac Cardiovasc Surg. 2013;146:1041–6.
Agarwal R, Srinivas R, Nath A, Jindal SK. Is the mortality higher in the pulmonary vs the extrapulmonary ARDS? A meta analysis. Chest. 2008;133:1463–73.
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–63.
Augustin P, Lasocki S, Dufour G, Rode J, Karsenti A, Al-Attar N, Bazeli R, Montravers P. Abdominal compartment syndrome due to extracorporeal membrane oxygenation in adults. Ann Thorac Surg. 2010;90:e40–1.
Okhuysen-Cawley R, Prodhan P, Imamura M, Dedman AH, Anand KJ. Management of abdominal compartment syndrome during extracorporeal life support. Pediatr Crit Care Med. 2007;8:177–9.
Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, Duchesne J, Bjorck M, Leppaniemi A, Ejike JC, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190–206.
Prodhan P, Imamura M, Garcia X, Byrnes JW, Bhutta AT, Dyamenahalli U. Abdominal compartment syndrome in newborns and children supported on extracorporeal membrane oxygenation. ASAIO J. 2012;58:143–7.
Schreiber J, Nierhaus A, Vettorazzi E, Braune SA, Frings DP, Vashist Y, Izbicki JR, Kluge S. Rescue bedside laparotomy in the intensive care unit in patients too unstable for transport to the operating room. Crit Care. 2014;18:R123.
Acknowledgements
Written informed consent for the publication of individual details was obtained from the participant.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Katsuhara, K., Nakada, Ta., Yamada, M. et al. Veno-venous extracorporeal membrane oxygenation (ECMO) for acute respiratory failure caused by liver abscess. J Artif Organs 18, 173–176 (2015). https://doi.org/10.1007/s10047-014-0807-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-014-0807-8