Abstract
Purpose
We studied the effectiveness of biomechanically calculated abdominal wall reconstructions for incisional hernias of varying complexity in an open, prospective observational registry trial.
Methods
From July 1st, 2017 to December 31st, 2020, four hospitals affiliated with the University of Heidelberg recruited 198 patients with complex incisional hernias. Hernias were repaired using biomechanically calculated reconstructions and materials classified on their gripping force towards cyclic load. This approach determines the required strength preoperatively based on the hernia size, using the Critical Resistance to Impacts related to Pressure. The surgeon is supported in reliably determining the Gained Resistance, which is based on the mesh-defect-area-ratio, as well as other mesh and suture factors, and the tissue stability. Tissue stability is defined as a maximum distension of 1.5 cm upon a Valsalva maneuver. In complex cases, a CT scan of the abdomen can be used to assess unstable tissue areas both at rest and during Valsalva’s maneuver.
Results
Larger and stronger gripping meshes were required for more complex cases to achieve a durable repair, especially for larger hernia sizes. To achieve durable repairs, the number of fixation points increased while the mesh-defect area ratio decreased. Performing these repairs required more operating room time. The complication rate remained low. Less than 1% of recurrences and low pain levels were observed after 3 years.
Conclusions
Biomechanical stability, defined as the resistance to cyclic load, is crucial in preventing postoperative complications, including recurrences and chronic pain.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Many people worldwide require surgical treatment for an abdominal incisional hernia every year [1]. Recurrence and chronic pain are significant risks. Around 25% recur within five years. Ten percent of chronic pain is observed [2]. Patients with complex incisional hernias experience more recurrences and higher pain levels. Biomechanically calculated reconstruction (BCR) offers superior outcomes [3].
BCR determines the required strength (critical resistance to impacts related to pressure—CRIP). The surgeon calculates the strength of the designed repair preoperatively (gained resistance—GRIP). The GRIP considers the mesh-defect-area-ratio (MDAR), mesh, suture and other factors [3,4,5].
We investigated the effectiveness of BCR for incisional hernias of varying complexity. Our analysis is based on a cohort of patients observed prospectively.
Materials and methods
Patients
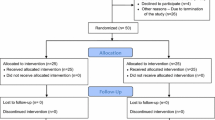
From July 1st, 2017 to December 31st, 2020, four hospitals affiliated with the University of Heidelberg recruited 198 patients for an open observational prospective registry study on complex incisional hernia repair. These patients were included in the Stronghold chapter of the Herniamed® Registry [3].
The Stronghold study is an extension of the Herniamed® registry. Stronghold started in 2017. The aim of the registry is to improve the quality of patient care by monitoring procedures and analysing outcome data. All interested surgeons can easily enter data according to a scientifically validated standard procedure. Patient consent is required [6]. STRONGHOLD follows the same principles as any Herniamed® subset. But it collects seven additional items for biomechanically calculated reconstruction: form of mesh implanted, minimal overlap, number and kind of fixation, pull-out or adapting sutures, type of peritoneal closure and MDAR.
We excluded seven deceased patients from the analysis. The only recurrence is presented and discussed separately. The remainder of 190 patients were classified for complexity. The complexity of incisional hernia repair was evaluated using the Herniamed® approach published in 2021 [2]. The complexity of incisional hernia increases with a defect width above 10 cm, a lateral defect site, a recurrent hernia, age over 80, BMI over 30, comorbidities with adverse metabolic consequences (such as diabetes mellitus), elevated intraabdominal pressure (such as chronic obstructive airways disease), increased risk of bleeding (such as genetic or iatrogenic clot reduction), reduced wound healing (such as concomitant chemotherapy), abnormal gait (for example after a stroke or an amputation), concomitant stoma or intra-abdominal bowel repair (e.g. for the relief of obstruction) and intensified surgery such as component separation. We developed the incisional hernia complexity score by awarding one point for each category. If multiple comorbidity-related risk factors were present, they were combined into a single point.
Surgical procedures
Our hernia repair is based on the concept of biomechanically calculated reconstruction (BCR). The concept is guided by three questions to be answered during the evaluation process (as illustrated in Fig. 1).
The clinical pathway for biomechanically calculated repair (BCR) involves clinical assessment, abdominal CT with Valsalva if necessary, and calculation of MDAR, CRIP and GRIP values as previously described in references [3,4,5] and [10]. The process is guided by three questions (Q 1–3). The arrow shows the iteration process to reach GRIP > CRIP. The following calculations are included: CRIP = (0.5 * hernia size + 15) * tissue distension [3]. GRIP = MDAR * coefficients for mesh adhesiveness, mesh position in the abdominal wall, number and type of fixation plus factors for peritoneal and fascial closure [3]. For a durable reconstruction, GRIP should be above CRIP
BCR yields CRIP and GRIP to guide the design of the surgical procedure. BCR preoperatively determines the required strength, depending on the hernia size, using Critical Resistance to Impacts related to Pressure (CRIP). Mesh-defect-area-ratio, CRIP and GRIP values were calculated as previously described (Fig. 1) [3,4,5]. GRIP is based on the mesh-defect-area-ratio, mesh and suture factors. The distension of the hernia size and/or the unstable area of the abdominal wall as a measure of tissue stability influences CRIP. Calculating CRIP and GRIP involves four divisions, six multiplications, and one to two additions. It takes approximately five minutes with a pocket calculator. We used a conventional Excel® sheet to determine the hernia and mesh sizes, the number and type of fixation, and the position within the abdominal wall.
Tissue stability was defined as a maximum distension of 1.5 cm during the Valsalva maneuver. In complex cases, unstable tissue areas can be assessed with a CT scan of the abdomen at rest and during Valsalva’s maneuver. To evaluate by hand, three observers must take at least four independent readings of the hernia's width, length, and height. This ensures an interobserver variation of less than 5% [7]. To speed up the process, we developed HEDI [8] as an AI tool to assess tissue stability. HEDI’s evaluation of dynamic computed tomography at rest and during the Valsalva maneuver automatically detects and assesses hernia size, volume and abdominal wall instability. The tool has been in development since the detection of the only recurrence in 2020. Each unstable abdominal wall exhibits a unique strain pattern upon cyclic load (Fig. 2 as an illustration).
Output of HEDI [8] for 3 patients with a CRIP of approximately 230 during a Valsalva maneuver. For a–c top: at rest, bottom: during Valsalva maneuver, from left to right: strain distribution with higher strain values in red, area of instability > 15 mm starting at the edge of red to blue, hernia opening (shaded in dark red) with musculature (blue and grey) and mesh landing zone (ochre). The iteration process in Fig. 1 has to take into account the needs to dissipate the energy input by cyclic load and to counteract the anisotropic distension of mesh and tissue. The larger the sizes of the hernia and the unstable wall area, the larger the mesh. More distension increases the need for fixation
DIS class A meshes (Dynamesh® Cicat, Progrip®) with high gripping coefficients were used for complex abdominal wall reconstruction [9]. Most procedures were performed with an open access but MILOS or laparoscopic approaches were also used [4, 5].
The number of intraoperative complications may include bowel lacerations that do not open the internal lining and may be closed with simple sutures. It may also include bleeding requiring hemostatic sutures and unwanted events of any kind. Postoperative complications may include wound or mesh infection or seroma formation, deep vein thrombosis, pulmonary embolism, pneumonia, bleeding, urinary infection, transient or prolonged myocardial or brain ischemia and stroke. Any re-operation within 30 days was recorded.
Hernia repair was embedded into a pre- and rehabilitation program (Fig. 3).
Pre- and rehabilitation before and after BCR. CTAV computed tomography at rest and during a Valsalva maneuver, CRIP critical resistance to impacts related to pressure, GRIP gained resistance to impacts related to pressure. Wounds typically heal within two weeks. To promote stable scar formation, the authors recommend to wear an abdominal binder during wound healing, both day and night, and during physical activity afterwards
Follow up procedures
Patients were regularly followed-up via telephone interviews with themselves, known relatives, or family physicians. During these interviews, patients were asked about any unwanted effects, such as pain at rest or during exercise, that required medication. All re-operations, including imaging and a review of the OR report, were assessed. Patients with bulges on the body were asked to come to the hospital for clinical examination and, if necessary, ultrasonography, magnetic resonance imaging or computed tomography. No patient was lost to follow-up.
Statistics
Key descriptive statistics were calculated as given in Tables 1–5. As the data were skewed, non-parametric tests (group homogeneity with Kruskal–Wallis, then u-tests if necessary) were evaluated.
Results
In the study group without recurrences, 95 women and 95 men had a median age of 64 years (mean ± SD: 63 ± 12, range: 27–92 years). The only recurrence occurred in May 2020, eight months after the initial repair, in a female recipient of liver transplant.
After classification to the new Herniamed® approach, 18 patients no longer underwent a complex incisional hernia repair. Each remaining patient had between one and five risk factors (refer to Table 1).
In the remaining 172 patients, the complexity of the incisional hernia ranged from one to five, as shown in Table 2. Otherwise, the cohorts are comparable.
Uncomplicated cases with a complexity score of 0 consisted of primary incisional hernias treated electively. As complexity increases, the number of male patients increases, while age and BMI remain constant. The increase in preoperative pain levels tended to coincide with higher complexity. No significant trends were found.
Hernia sizes increased significantly as the complexity increased (p < 0.00001). Larger meshes are required to achieve durable repair for larger hernia sizes (p < 0.00001; see Table 3). The number of fixation points increased while the mesh-defect area ratio decreased (p < 0.00001) to achieve a GRIP value above CRIP. Additional OR time is required to perform durable repair for larger or more complex herniae (p < 0.00001).
HEDI was not necessary for less complex repairs. The HEDI output is related to abdominal wall instability. The distorsion field is calculated using a symmetric diffeomorphic registration method [8]. It was first applied in 2% of cases with a complexity score of 2, 6% in group 3, and 9% in group 4. In the most complex cases, one-third of cases were assessed using HEDI. However, since HEDI became available in 2020, the last year of recruitment for this report, this does not reflect the true need. Today, every complex case is evaluated with HEDI before elective repair. This is done to gain insight into biomechanical parameters [8].
In the highest-complexity group, 94% of patients underwent transversus abdominis release augmented with a DIS class A mesh with non-resorbable suture fixation. Furthermore, half of the patients underwent a single crown tack fixation using absorbable tacks. In addition, 44% had a second mesh in the intraperitoneal underlay repair (IPUM as a sandwich, usually with a biosynthetic Phasix® mesh). To counteract a jump of tissue compliance at fascial or bony edges, transmural fully absorbable pull-out sutures and Arthrex® bone anchors were used in 11% and 9% of cases. Area bonding with fibrin glue was used to dissipate the energy of cyclic loading in 6%. The patient with over 80% domain loss and tissue distension exceeding 10 cm was treated with progressive pneumoperitoneum. No botulinum toxin or Fasciotens® was necessary in any case. The calculated GRIP increased from no complexity to complexity level 4 (p = 0.00203) and remained constant thereafter because the GRIP coefficients of these combined procedures for complexity class 5 cases have not yet been determined. Surgical access was open for retromuscular, TAR, and sandwich repair in 82%, MILOS in 11%, and laparoscopic eTAR in 7% of all cases. No robotic procedures were performed in this study. The increase in operation time reflects the increasing complexity of the surgical requirements.
Patients with increasingly complex abdominal wall repairs required a longer hospital stay (p = 0.00031, Table 4). There was a tendency for more intra- and postoperative complications with increasing complexity. The rate of reoperations remained constant. Pain at discharge was comparable in all groups and diminished thereafter (Table 5). At the 3-year follow-up, only one patient occasionally took an analgesic, while 189 patients did not take any. All patients under the age of 62 were able to return to work after 14 weeks of rehabilitation. Some of these patients had been on and off work for up to 20 years prior to BCR.
Discussion
In an open prospective observational registry trial, we studied the effectiveness of biomechanically calculated abdominal wall reconstructions for incisional hernias of varying complexity. This report expands previous knowledge on biomechanical stability of herniated abdominal walls on a larger patient base [3, 10]. Our study provides insight into complexity-related biomechanical aspects of incisional hernia repair. Our results are positive.
The human abdominal wall consists of different layers of polymers, including the aponeurosis, fascia, and musculature [11]. BCR repairs a defect with a DIS class A textile [3]. Similar to engineering and materials science, cyclic loading is crucial to test the behavior of structural composite. It refers to the application of repeated or fluctuating stresses, strains or stress intensities at specific locations on structural elements. In complex incisional hernia repair as well as in aerospace, automotive, civil engineering, and orthopedics, cyclic loading can cause degradation over time [12].
To develop BCR, two new technologies were necessary [8, 9]. First, biomechanical testing is required using a home-built cyclic loading bench test. This test is now in its fourth generation and includes temperature control, varying tissue stretch, pressure, impact area and other features. Second, HEDI was developed as an AI based tool to assess tissue quality. The HEDI program can be run on a standard computer from 2021 at a cost of US$ 1,500 and is available for free on GitHub.
It is important to stabilize unstable wall areas in our biomechanical concept. It is also important to durably close hernia openings. Unstable wall areas, such as rectal diastasis, can occur without a hernia. Hernia openings, such as those in lateral inguinal hernia, can occur without unstable wall areas. In the case of complex incisional hernia, it is necessary to consider both aspects together. The issue of stability revolves around collagen turnover because freshly formed collagen is unstable and requires approximately 84 days for durable cross-linking [13, 14]. Comorbidities affect the time required for collagen formation and stabilisation as well as other tissue components, which can affect the extent of instability. The hernia size is influenced by previous surgical procedures (Fig. 4).
The biomechanical parameters of durable abdominal wall repairs are influenced by complexity and comorbidity. The hernia orifice, located in the center, is often surrounded by an unstable area of the abdominal wall (solid and broken lines). Weak collagen resulting from comorbidities can increase tissue distension and the unstable area of the abdominal wall, leading to higher CRIP values. Complexity-related factors determine the size and location of the hernia orifice. These factors can cause increased tissue distension and instability (see Fig. 2 for further illustration)
Consideration of the biomechanical principles of cyclic loading enables durable repair of incisional hernias, even in very complex cases [3, 5]. Approximately 50% of our patients have an elasticity of >20% or a shift of >15 mm; therefore, it is important to identify and repair any unstable areas of the abdominal wall [4, 15].
We observed one recurrence in a 64-year-old woman with a 20 cm wide and 32 cm long incisional hernia after liver transplantation under continued immunosuppression. At that time, we calculated the hernia size from four repeated assessments of a CT scan at rest and during a Valsalva maneuver performed by three different observers to achieve less than 5% variation [4, 7]. In this patient, the interobserver variation was 18%. After eight months of follow-up, a recurrence was observed at the right lateral edge of the L-shaped incision. In retrospect, this was caused by a high laxity area, which resulted in a high variation of hernia size assessment. We believe that the recurrence is a consequence of this area.
To address this issue, we developed HEDI, an AI tool that detects unstable abdominal wall [8]. HEDI is now routinely used to identify lax tissue zones with high tissue distortion. We believe that HEDI analysis is superior to computer simulation. Because the effects are directly observed, can be checked by independent observers, and depend only on the power exerted by the patient [16]. Simulation scenarios are often limited by neglecting the effects of cyclic impacts or boundary conditions that do not reflect realistic loads [17].
Our group has published papers on biomechanics to evaluate the underlying shakedown concept in more detail [4, 10, 13]. We found that 15 mm is a good general value for distinguishing between stable and unstable areas; therefore, we use this limit in our clinical work. The latest application of HEDI enables alternative options in millimetre steps, as well as 2D and 3D projection. Further research is required on this topic.
Recently, there have been attempts to classify the complexity of incisional hernia repair. This is done to prioritise patients on waiting lists, assess quality of life, outcomes, recovery, and recurrence rates. New meshes and modern surgical techniques are also considered [2, 18, 19]. Our study is the first to relate biomechanics to the complexity of incisional hernia repair. Our results are positive. We summed all comorbidities into one point owing to their biomechanical effect, which increases tissue laxity (Fig. 2 refer to Fig 4).
Bleeding disorders were thought to have a direct impact on complication rate, but this study shows otherwise. Our CEDAR risk analysis revealed complication risks ranging from 25 to 99%, but complication rates in our study ranged from 0 to 26%, including minor events [20]. Stabilized tissue appears to minimize complications such as seroma or hematoma formation.
Biomechanical stability is crucial to prevent postoperative complications and recurrence. Similar to calcified tissue, soft tissue fusion and healing requires stability [21]. Stabilized tissue exudates briefly followed by collagen formation. Crosslinks form in stable tissue within weeks [13]. These data, our group’s previous publications [3,4,5, 7,8,9, 12] and the work presented in [15, 22] were used to develop a clinical pathway (Figs. 1–3).
Abdominal wall instability can lead to burst abdomen and incisional hernia. They may develop within days or weeks after surgery [23]. In a pilot study of 800 patients who underwent major surgery at our hospital, we found that 13% developed incisional hernias after 1 year, with 3% being complex cases (20% of all incisional hernias after one year). Therefore, we recommend secondary prophylaxis: all patients at risk should be assessed within months after surgery, and hernias should be repaired early to avoid complex cases.
Recurrences of incisional hernias occur early but may not become apparent until later, with two-thirds of recurrent incisional hernias becoming apparent after three years [24]. Our study shows that complex incisional hernias can be repaired with very low recurrence rates when considering biomechanical and cyclic loading principles. This study found that after three years, BCR can result in 99% durable repairs of complex incisional hernias.
A complex incisional hernia cannot be repaired by simply using a larger mesh or more fixation [12, 25]. For a stable mesh-tissue interface and for pain-free fixation, it is important to consider the gripping force towards cyclic load [3, 9, 15].
Complex surgeries result in longer surgery times and hospital stays. They require better materials, ultimately resulting in more investment. However, the investment is balanced by the benefit of doing the correct repair the first time around. BCR can help achieve this. Additionally, pain, which increases with complexity, decreases after a biomechanically calculated repair.
Conclusions
Preoperative calculations of biomechanical stability can guide the surgical design of complex hernia repair. Complexity can be scored related to biomechanics. Durable repairs require materials and OR time that are significantly related to increasing complexity of incisional hernia. Complex incisional hernia can be repaired at very low recurrence and chronic pain rates considering biomechanical and cyclic loading principles. Randomized trials are needed to confirm the advances possible with BCR, as this study provides the first promising long-term results.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation considering restrictions by national and European data protection laws. All data supporting the findings of this study are available within the paper.
Abbreviations
- BCR:
-
Biomechanically calculated reconstruction
- CRIP:
-
Critical resistance to impacts related to pressure
- GRIP:
-
Gained resistance to impacts related to pressure
- BMI:
-
Body mass index
- NAS:
-
Numerical-analog scale
- MDAR:
-
Mesh-to-defect-area-ratio
- HEDI:
-
Hernia evaluation, detection and imaging
- AI:
-
Artificial intelligence
- MILOS:
-
Mini- or less-open sublay operation
- OR:
-
Operation room
- DIS:
-
Dynamic intermittent strain
- IPUM:
-
Intraperitoneal underlay mesh
- CT:
-
Computed tomography
- CEDAR:
-
Carolina estimate of disease adjusted risk
- HbA1c:
-
Glycosylated hemoglobin type A1c
- CTAV:
-
CT abdomen at rest and during a Valsalva maneuver
References
Deerenberg EB, Henriksen NA, Antoniou GA, Antoniou SA, Bramer WM, Fischer JP, Fortelny RH, Gök H, Harris HW, Hope W, Horne CM, Jensen TK, Köckerling F, Kretschmer A, López-Cano M, Malcher F, Shao JM, Slieker JC, de Smet GHJ, Stabilini C, Torkington J, Muysoms FE (2022) Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. Br J Surg 109:1239–1250. https://doi.org/10.1093/bjs/znac302
Hoffmann H, Köckerling F, Adolf D, Mayer F, Weyhe D, Reinpold W, Fortelny R, Kirchhoff P (2021) Analysis of 4,015 recurrent incisional hernia repairs from the Herniamed registry: risk factors and outcomes. Hernia 25:61–75. https://doi.org/10.1007/s10029-020-02263-x
Lesch C, Nessel R, Adolf D, Hukauf M, Köckerling F, Kallinowski F, STRONGHOLD, Herniamed-Collaborators GROUP; Willms A, Schwab R, Zarras K, (2024) STRONGHOLD first-year results of biomechanically calculated abdominal wall repair: a propensity score matching. Hernia 28:63–73. https://doi.org/10.1007/s10029-023-02897-7
Kallinowski F, Ludwig Y, Löffler T, Vollmer M, Lösel PD, Voß S, Görich J, Heuveline V, Nessel R (2021) Biomechanics applied to incisional hernia repair - Considering the critical and the gained resistance towards impacts related to pressure. Clin Biomech (Bristol, Avon) 82:105253. https://doi.org/10.1016/j.clinbiomech.2020.105253
Nessel R, Löffler T, Rinn J, Lösel P, Voss S, Heuveline V, Vollmer M, Görich J, Ludwig YM, Al-Hileh L, Kallinowski F (2021) Primary and recurrent repair of incisional hernia based on biomechanical considerations to avoid mesh-related complications. Front Surg 8:764470. https://doi.org/10.3389/fsurg.2021.764470
Herniamed Qualitätssicherungsstudie. Datenschutzrechtliche Aufklärung und Einwilligung inkl. Information gem. Art.13 DS-GVO und Information über die wesentlichen Inhalte der Vereinbarung über die gemeinsame Verantwortlichkeit nach Art. 26 Abs. 2 S.2 der DS-GVO (2022). Available at https://www.herniamed.de/sites/default/files/Einwilligungserklaerung.pdf
Kallinowski F, Nessel R, Gorich J, Grimm A, Loffler T (2020) CT Abdomen with Valsalva’s maneuver facilitates grip-based incisional hernia repair. J Abdom Wall Reconstr. 2:1006
Relle JJ, Voß S, Raschidi R, Nessel R, Görich J, Wielpütz MO, Löffler T, Heuveline V, Kallinowski F, Lösel PD (2023) HEDI: First-Time Clinical Application and Results of a Biomechanical Evaluation and Visualisation Tool for Incisional Hernia Repair. Preprint at arXiv.2307.01502
Kallinowski F, Harder F, Gutjahr D, Raschidi R, Silva TG, Vollmer M, Nessel R (2018) Assessing the GRIP of ventral hernia repair: How to securely fasten dis classified meshes. Front Surg 4:78. https://doi.org/10.3389/fsurg.2017.00078
Deeken CR, Lake SP (2017) Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J Mech Behav Biomed Mater 74:411–427. https://doi.org/10.1016/j.jmbbm.2017.05.008
Karrech A, Ahmad H, Hamdorf JM (2023) Biomechanical stability of hernia-damaged abdominal walls. Sci Rep 13:4936. https://doi.org/10.1038/s41598-023-31674-w
Kallinowski F, Ludwig Y, Gutjahr D, Gerhard C, Schulte-Hörmann H, Krimmel L, Lesch C, Uhr K, Lösel P, Voß S, Heuveline V, Vollmer M, Görich J, Nessel R (2021) Biomechanical influences on mesh-related complications in incisional hernia repair. Front Surg 8:763957. https://doi.org/10.3389/fsurg.2021.763957
Münster S, Jawerth LM, Leslie BA, Weitz JI, Fabry B, Weitz DA (2013) Strain history dependence of the nonlinear stress response of fibrin and collagen networks. Proc Natl Acad Sci USA 110:12197–12202. https://doi.org/10.1073/pnas.1222787110
Ristaniemi A, Torniainen J, Stenroth L, Finnilä MAJ, Paakkonen T, Töyräs J, Korhonen RK (2020) Comparison of water, hydroxyproline, uronic acid and elastin contents of bovine knee ligaments and patellar tendon and their relationships with biomechanical properties. J Mech Behav Biomed Mater 104:103639. https://doi.org/10.1016/j.jmbbm.2020.103639
Nessel R, Lesch C, Vollmer M, Kallinowsk F (2023) Biomechanical principles of a permanently durable abdominal wall reconstruction: current status and potential future development. Mini-invasive Surg 7:21. https://doi.org/10.20517/2574-1225.2023.21
Chittajallu SNSH, Richhariya A, Tse KM, Chinthapenta V (2022) A Review on damage and rupture modelling for soft tissues. Bioengineering 9:26. https://doi.org/10.3390/bioengineering9010026
Aly OE (2023) Addressing parastomal herniation through biomechanical simulation. Hernia 27:565–573. https://doi.org/10.1007/s10029-022-02704-9
Roth JS, Anthone GJ, Selzer DJ, Poulose BK, Bittner JG, Hope WW, Dunn RM, Martindale RG, Goldblatt MI, Earle DB, Romanelli JR, Mancini GJ, Greenberg JA, Linn JG, Parra-Davila E, Sandler BJ, Deeken CR, Voeller GR (2018) Prospective evaluation of poly-4-hydroxybutyrate mesh in CDC class I/high-risk ventral and incisional hernia repair: 18-month follow-up. Surg Endosc 32:1929–1936. https://doi.org/10.1007/s00464-017-5886-1
Petersson P, Montgomery A, Petersson U (2020) Modified peritoneal flap hernioplasty versus retromuscular technique for incisional hernia repair: a retrospective Cohort study. Scand J Surg 109:279–288. https://doi.org/10.1177/1457496919863943
Katzen M, Ayuso SA, Sacco J, Ku D, Scarola GT, Kercher KW, Colavita PD, Augenstein VA, Heniford BT (2023) Outcomes of biologic versus synthetic mesh in CDC class 3 and 4 open abdominal wall reconstruction. Surg Endosc 37:3073–3083. https://doi.org/10.1007/s00464-022-09486-2
Saul D, Menger MM, Ehnert S, Nüssler AK, Histing T, Laschke MW (2023) Bone healing gone wrong: pathological fracture healing and non-unions-overview of basic and clinical aspects and systematic review of risk factors. Bioengineering (Basel) 10:85. https://doi.org/10.3390/bioengineering10010085
Kallinowski F (2022) Biomechanics of mesh repair of the herniated abdominal wall: requires some knowledge of stochastic processes. https://websurg.com/doi/lt03en24558. Accessed 16 Mar 2022
Franz MG (2008) The biology of hernia formation. Surg Clin North Am 88(1–15):vii. https://doi.org/10.1016/j.suc.2007.10.007
Köckerling F, Koch A, Lorenz R, Schug-Pass C, Stechemesser B, Reinpold W (2015) How long do we need to follow-up our hernia patients to find the real recurrence rate? Front Surg 2:24. https://doi.org/10.3389/fsurg.2015.00024
Zamkowski M, Tomaszewska A, Lubowiecka I, Śmietański M (2023) Biomechanical causes for failure of the Physiomesh/Securestrap system. Sci Rep 13: 17504. https/doi.org/https://doi.org/10.1038/s41598-023-44940-8
Acknowledgements
We are grateful for the cooperation with Dr. Philipp Lösel, Department of Materials Physics at the Australian National University, and Jacob Relle, M.Sc., Engineering Mathematics and Computing Lab (EMCL), Interdisciplinary Center for Scientific Computing (IWR), Heidelberg University, for the HEDI project. We cordially thank Cristina Debellis, Personal Secretarial Assistant to the Surgical Directorate, for consistently following the patients with great enthusiasm and dedicated care who now eagerly performs the five-year recalls.
Funding
Open Access funding enabled and organized by Projekt DEAL. Heidelberger Stiftung Chirurgie grants No. 2016/22, 2017/171, 2018/215, 2019/288, 2020/376 and 2021/444
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The studies for computed tomography at rest and during Valsalva maneuver were reviewed and approved by the Ethics Committee of the Heidelberg University vote S-522/2020. STRONGHOLD as part of the HERNIAMED registry complies with the Declaration of Consent of the HERNIAMED database [amedHernie; 6]. The Herniamed Registry has ethical approval (BASEC Nr. 2016-00123, 287/2017BO2/F-2022-111). The patients/participants provided their written informed consent to participate in the respective study in accordance with the national legislation and the institutional requirements.
Informed consent
The patients/participants provided their written informed consent to participate in the respective study in accordance with the national legislation and the institutional requirements.
Conflict of interests
The institution of FK recieved honoraria for lectures or educational events from Medtronic® and Becton Dickinson®, support for attending meetings by Becton Dickinson® and Dahlhausen® and receipt of equipment and materials from Dahlhausen® and Corza® medical, Germany. The other authors have no conflict of interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Complex Incisional Hernia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nessel, R., Löffler, T., Rinn, J. et al. Three-year follow-up of the grip concept: an open, prospective, observational registry study on biomechanically calculated abdominal wall repair for complex incisional hernias. Hernia 28, 913–924 (2024). https://doi.org/10.1007/s10029-024-03064-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-024-03064-2