Abstract
Purpose
The TransREctus sheath PrePeritoneal procedure (TREPP) was introduced as an alternative open and preperitoneal technique for inguinal hernia mesh repair, demonstrating safety and efficacy in retro- and prospective studies. However, little is known about the technique’s inherent learning curve. In this study, we aimed to determine TREPP learning curve effects after its implementation in high-volume surgical practice.
Methods
All primary, unilateral TREPP procedures performed in the first three years after implementation (between January 2016 and December 2018) were included out of a large preconstructed regional inguinal hernia database. Data were analyzed on outcome (i.e., surgical complications, hernia recurrences, postoperative pain). Learning curve effects were analyzed by assessing outcome in relation to surgeon experience.
Results
In total, 422 primary, unilateral TREPP procedures were performed in 419 patients. In three patients a unilateral TREPP procedure was performed on both sides separated in time. A total of 99 surgical complications were registered in 83 procedures (19.6% of all procedures), most commonly inguinal postoperative pain (8%) and bleeding complications (7%). Hernia recurrences were observed in 17 patients (4%). No statistically significant differences on outcome were found between different surgeon experience (< 40 procedures, 40–80 procedures, > 80 procedures).
Conclusion
Implementation of TREPP seems not to be associated with a notable increase of adverse events. We were not able to detect a clear learning curve limit, potentially suggesting a relatively short learning curve among already experienced hernia surgeons compared to other guideline techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The TransREctus sheath PrePeritoneal procedure (TREPP) has emerged as an alternative open and preperitoneal approach to inguinal hernia repair. During this procedure, the preperitoneal space is accessed by opening the anterior layer of the rectus sheath. After reduction of the medial, lateral and/or femoral hernia a mesh with a self-expanding ring is inserted covering all hernia sites [1,2,3]. Recent studies show comparable or more favorable outcomes than Lichtenstein repair or minimal invasive surgery (laparo-endoscopic or robotic) [4, 5]. It offers the possibility of preperitoneal mesh placement through an open but minimal invasive approach, without the need for endoscopic surgical facilities or general anesthesia risks. Other potential advantages attributed to TREPP may be lower treatment costs and its applicability in emergency surgery for strangulated inguinal hernia [6].
However, the implementation of TREPP in inguinal hernia treatment is hampered by limited experience and, thus, subject to debate. Although the body of evidence is expanding, questions still remain concerning its applicability in current surgical practice [7]. We have previously investigated that TREPP shows comparable efficacy (in terms of recurrences) and morbidity (in terms of postoperative pain and surgical site-related complications) compared to either conventional open (Lichtenstein) or endoscopic (totally extraperitoneal, TEP) inguinal hernia surgery in a large cohort [8]. Nonetheless, currently available literature does not allow any recommendation about the preferred approach to preperitoneal mesh placement, in accordance with the international guidelines for groin hernia management [9].
A major caveat both in interpreting current TREPP data as well as in implementing this novel technique in day-to-day surgical practice is our lacking understanding (knowledge) of its learning curve. It is likely that the ease of adding this technique to the surgeon’s operative armamentarium will determine its use alongside already established techniques.
The aim of this retrospective study is to gain insights in the TREPP learning curve by analyzing the occurrence of adverse events (surgical complications and hernia recurrences) and operating time—by way of proxy—during the implementation of this novel procedure in a high-volume, regional surgical collaborative.
Materials and methods
Study design
We previously performed a propensity-score-matched analysis of consecutive patients undergoing inguinal hernia repair in a multicenter regional surgical collaborative in the Netherlands [8]. For the current study, we included patients who underwent TREPP procedures between January 1st 2016 and December 31st 2018. In our selection, we included all primary and unilateral inguinal hernias for which TREPP was performed. Cases with bilateral inguinal hernias or recurrences were excluded. In this period, the TREPP was implemented in our surgical practice among experienced hernia surgeons. Follow-up registry was updated until November 2019, comprising data on surgical complications and hernia recurrence. In addition, procedural parameters were obtained from the operation logs, including duration of surgery and composition of the surgical team. All data were acquired and anonymized adhering to Dutch and institutional regulations. The Medical Ethics Committee of our institution (RTPO Leeuwarden) confirmed the conduct of this retrospective study without the need for ethical review, and the institutional board approved the execution of the study without the need for consent in accordance with Dutch regulations.
Surgical procedure
All patients underwent TREPP inguinal hernia repair following nine key-steps, as described previously [1]. For all procedures, a polypropylene mesh with a memory ring was used (PolySoft Hernia patch, Bard Medical, the Netherlands, and the Rebound mesh, Duomed, the Netherlands). Procedures were performed by 14 different surgeons with extensive experience in conventional open and endoscopic hernia repair techniques. Four surgeons also had previous TREPP experience (see Supplementary Table A). Surgeons without previous TREPP experience were introduced to the technique by proctor-TREPP surgeons. The procedure was implemented subsequently in our surgical group, with other surgeons being supervised by one of these proctors during the first procedures. When the proctoring surgeon deemed the surgeon sufficient in the described 9-step technique (as described by Akkersdijk et al. [1]), this surgeon would continue with performing the procedures without supervision.
Outcome measures
Postoperative follow-up at the outpatient clinic was performed routinely at 2–6 weeks after surgery. Additional visits were scheduled in case of adverse events, or after subsequent referral. Charts were reviewed for information on several procedure-related adverse events—including postoperative pain, surgical site infection, hematoma/bleeding, seroma formation—and hernia recurrence. Postoperative pain was defined as any registrations in the patient file of additional outpatient clinic evaluation after regular follow-up due to complaints of inguinal pain or by receiving additional diagnostic studies, analgesic treatment or referral to a pain specialist [8], Furthermore, operating time (i.e., time between incision and wound closure) and composition of surgical team (as procedures during the early implementation period were more often performed by two surgeons) were registered from the operation logs.
Adverse events (defined as both surgical complications—i.e., bleeding, infectious sequelae, postoperative pain and seroma formation—as well as hernia recurrence) were used as proxies to determine learning curve effects in keeping with similar studies [10], by analyzing their temporal incidence based on ranking consecutive procedures per surgeon.
Statistical analysis
Patient and procedural characteristics are displayed using descriptive statistics. Chi-square and two-tailed Fisher’s exact tests were used to analyze the relationships between categorical variables, to which end data were dichotomized as described explicitly in text and tables. To analyze the influence of increasing experience on our outcome variables, we plotted the occurrence of adverse events in relation to increasing surgeon experience for TREPP procedures. Surgeons were categorized based on experience, for which comparisons were performed using the Kruskal–Wallis test and cross-tabulation analyses as described above. All p values<0.05 (two sided) were considered statistically significant. All statistical analyses were performed using SPSS 24 (IBM, the Netherlands) and SAS 9.4 software (SAS Institute Inc., Cary, North Carolina, USA).
Results
Procedural characteristics
We overviewed data from 422 TREPP procedures in 419 patients, as shown in Fig. 1. Out of all cases, only primary, unilateral TREPPs were included. Table 1 shows patient and procedural characteristics.
The characteristics were representative for a general inguinal hernia cohort, with a male predominance, in general favorable ASA scores and median age at surgery of 58 years. TREPPs were mostly performed electively for primary, unilateral inguinal hernias. Median operating time was 21 min (range 9–70).
Adverse events
Table 2 summarizes the TREPP-related surgical complications and hernia recurrences—taken together as adverse events—observed in our cohort. A total of 94 surgical complications were registered, most commonly bleeding complications (6.6%) and postoperative inguinal pain (7.8%). The hernia recurrence rate was 4.0%.
Adverse events in relation to surgeon experience
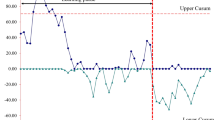
To further investigate the presence and magnitude of a learning curve effect on the occurrence of adverse events, data were analyzed sequentially by designating a rank number to each procedure performed per surgeon, thus reflecting the level of experience per surgeon. We considered previous experience (Supplementary Table A) of four surgeons with previous TREPP experience. Figure 2 shows the occurrence of adverse events in function of increasing TREPP experience. We corrected for previous TREPP experience when relevant, with lowest case numbers corresponding with surgeons new to this technique. Procedures performed by more experienced surgeons have higher case numbers. Adverse events are represented by the blue line. Recurrences are displayed by the green line.
Considering the lack of previous data on TREPP learning curve numbers, experience was divided based on tertiles, making experience groups of 40: little experience (<40 procedures), medium experience (40–80 procedures) and much experience (>80 procedures). This is consistent with learning curve studies for other inguinal hernia techniques that used cut off point at 30–35 procedures. Results in these groups are shown in Table 3. We did not observe a significantly higher overall incidence of adverse events among TREPPs performed by hernia surgeons with little TREPP experience, compared to their counterparts with much TREPP experience before implementation of the technique in our surgical practice. Recurrence rates were 3.5% (most experience) vs 2.0% (medium experience) vs 6.0% (no experience), p = 0.26. Postoperative pain was present in 8.2% of cases in the experienced group, compared to 5.9% (medium experience) and 8.7% (no experience), p = 0.71. We observed a statistically significant difference in operating time, being the shortest in the most experienced group; 21.6 (± 9.5) minutes (p = 0.001).
Discussion
TREPP seems to offer a promising alternative to more widely performed inguinal hernia mesh repairs, mainly endoscopic preperitoneal (TEP, TAPP) or open anterior (Lichtenstein) techniques. It enables preperitoneal mesh placement without the need for risk associated with general anesthesia or advanced technological resources. Previous large cohort studies show similar incidences of postoperative pain and recurrences when comparing TREPP to TEP or Lichtenstein [8, 11], while showing a significantly shorter operating time for TREPP [9, 11,12,13]. However, its place in the contemporary surgical practice has yet to be determined, and will likely depend on the ease with which the procedure can be learned and implemented [14, 15]. As stated by the HerniaSurge Group, there is a need for learning curve studies to determine the value of open preperitoneal mesh techniques [9].
This is currently the first study addressing a possible TREPP learning curve in common daily practice among experienced hernia surgeons. In our retrospective cohort, we analyzed the occurrence of adverse events (both surgical complications and inguinal hernia recurrences) in relation to surgeon experience with TREPP in 422 primary unilateral TREPP procedures (in 419 patients) with increasing level of TREPP procedure experience. These parameters are frequently used as proxies for learning curve effects, and have been widely used and validated in previous studies assessing the learning curves of various other hernia repair techniques [9, 16,17,18]. We conclude that the implementation of TREPP is not associated with a notable increase of adverse events, with outcomes comparable to known literature and no clear dependence on previous TREPP experience.
To our knowledge, this cohort is one of the largest available with physician-reported outcomes for TREPP surgery [6, 8]. One large retrospective study performed by Lange et al. described patient-reported (questionnaire) outcomes in 932 patients after TREPP, reporting 8% postoperative pain and 1–5% recurrence [2]. Both pain and recurrence have been primarily used as primary endpoints to describe the efficacy of TREPP. A recent randomized-controlled trial (ENTREPPMENT trial) comparing TREPP with transinguinal preperitoneal (TIPP) mesh repair reported inguinal pain in 7.2% and recurrence in 8.9% out of 400 patients one year after TREPP [14]. We assess a comparable 7.8% incidence of postoperative inguinal pain which is comparable to previous literature, as well as a 4% recurrence rate.
Although others have hypothesized that the TREPP learning curve could be favorable, total data were too small to support or reject this claim [3, 19]. Bökkerink et al. have recently shown in data from the ENTREPPMENT trial that the relatively high incidence of recurrences observed after TREPP was largely attributed to procedures performed by inexperienced TREPP surgeons [14]. After disregarding the first 10 procedures performed per surgeon, the recurrence rate dropped from 8.9% to 6.7%. Among the most experienced surgeons participating in that trial, they describe an even lower rate of 2.1% recurrences. However, no quantification is available for the length of the TREPP learning curve or the approximate number of proctored and/or supervised procedures needed by the individual surgeon to flatten the learning curve.
We hypothesized a learning curve of less than 40 procedures, but did not reach statistical significance in our analysis. This is likely caused by the inherently limited complication rate of inguinal hernia surgery, thus requiring a very large sample size for adequate statistical power, and the retrospective nature of our study. Nevertheless, the TREPP learning curve seems to compare favorably to its endoscopic counterpart. For the TEP procedure extensive clinical experience exists and several studies have been conducted analyzing its learning curve. Estimates between 50 and 100 procedures have been postulated for the TEP learning curve [20,21,22,23], but also upwards of 250–400 procedures results may further improve significantly before reaching a steady state [24].
It could be hypothesized that the apparently steep TREPP learning curve benefits from the generally shorter learning curves of open compared to endoscopic surgery. Another hypothesis could be the anatomical insight already available to surgeons with endoscopic experience. Therefore, it would be of great interest to analyze TREPP outcomes and learning curve effects among surgeons less or unfamiliar with endoscopic repair (i.e., residents or surgeons in developing countries). Although further research is suggested, our current data point out that the TREPP technique could be safely and expeditiously adapted into clinical practice.
References
Akkersdijk WL, Andeweg CS, Bokkerink WJ et al (2016) Teaching the transrectus sheath preperitoneal mesh repair: TREPP in 9 steps. Int J Surg 30:150–154. https://doi.org/10.1016/j.ijsu.2016.04.037
Lange JF, Lange MM, Voropai DA et al (2014) Trans rectus sheath extra-peritoneal procedure (TREPP) for inguinal hernia: the first 1,000 patients. World J Surg 38:1922–1928. https://doi.org/10.1007/s00268-014-2475-5
Koning GG, Andeweg CS, Keus F et al (2012) The transrectus sheath preperitoneal mesh repair for inguinal hernia: technique, rationale, and results of the first 50 cases. Hernia 16:295–299. https://doi.org/10.1007/s10029-011-0893-y
Reinhorn M, Fullington N, Agarwal D et al (2023) Posterior mesh inguinal hernia repairs: a propensity score matched analysis of laparoscopic and robotic versus open approaches. Hernia 27:93–104. https://doi.org/10.1007/s10029-022-02680-0
Agarwal D, Bharani T, Fullington N et al (2023) Improved patient-reported outcomes after open preperitoneal inguinal hernia repair compared to anterior Lichtenstein repair: 10-year ACHQC analysis. Hernia 27:1139–1154. https://doi.org/10.1007/s10029-023-02852-6
Zwols TLR, Akkersdijk WL, Bökkerink WJV et al (2020) Emergency TREPP for strangulated inguinal hernia repair: a consecutive case series. Surgery J 6:e62. https://doi.org/10.1055/S-0040-1705171
Andresen K, Rosenberg J (2017) Open preperitoneal groin hernia repair with mesh: a qualitative systematic review. Am J Surg 213:1153–1159. https://doi.org/10.1016/J.AMJSURG.2017.01.014
Zwols TLR, Slagter N, Veeger NJGM et al (2021) Transrectus sheath pre-peritoneal (TREPP) procedure versus totally extraperitoneal (TEP) procedure and Lichtenstein technique: a propensity-score-matched analysis in Dutch high-volume regional hospitals. Hernia 25:1265. https://doi.org/10.1007/S10029-020-02291-7
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Duclos A, Carty MJ, Peix JL et al (2012) Development of a charting method to monitor the individual performance of surgeons at the beginning of their career. PLoS ONE 7:e0041944. https://doi.org/10.1371/JOURNAL.PONE.0041944
Faessen J, Stoot J, Vugt R (2021) Safety and efficacy in inguinal hernia repair: a retrospective study comparing TREPP, TEP and Lichtenstein (SETTLE). Hernia 25:1309–1315. https://doi.org/10.1007/s10029-020-02361-w
Gutlic N, Gutlic A, Petersson U et al (2019) Randomized clinical trial comparing total extraperitoneal with Lichtenstein inguinal hernia repair (TEPLICH trial). Br J Surg 106:845–855. https://doi.org/10.1002/BJS.11230
Anwer AA, Hajibandeh S, Hajibandeh S et al (2022) Meta-analysis of the outcomes of trans rectus sheath extra-peritoneal procedure (TREPP) for inguinal hernia. Br J Surg 109:znac248.127. https://doi.org/10.1093/bjs/znac248.127
Bökkerink WJV, Koning GG, Vriens PWHE et al (2021) Open Preperitoneal Inguinal Hernia Repair, TREPP Versus TIPP in a Randomized Clinical Trial. Ann Surg 274:698. https://doi.org/10.1097/SLA.0000000000005130
Rosin D (2014) Trans-rectus sheath extra-peritoneal procedure (TREPP) for inguinal hernia: the first 1,000 patients. World J Surg 38:1929–1930. https://doi.org/10.1007/s00268-014-2495-1
Park YY, Lee K, Oh ST, Lee J (2022) Learning curve of single-incision laparoscopic totally extraperitoneal repair (SILTEP) for inguinal hernia. Hernia 26:959–966. https://doi.org/10.1007/s10029-021-02431-7
Feliu-Palà X, Martín-Gómez M, Morales-Conde S, Fernández-Sallent E (2001) The impact of the surgeon’s experience on the results of laparoscopic hernia repair. Surg Endosc 15:1467–1470. https://doi.org/10.1007/s00464-001-9017-6
Suguita FY, Essu FF, Oliveira LT et al (2017) Learning curve takes 65 repetitions of totally extraperitoneal laparoscopy on inguinal hernias for reduction of operating time and complications. Surg Endosc 31:3939–3945. https://doi.org/10.1007/s00464-017-5426-z
Bokkerink WJ, Persoon AM, Akkersdijk WL et al (2017) The TREPP as alternative technique for recurrent inguinal hernia after Lichtenstein’s repair: a consecutive case series. Int J Surg 40:73–77
Edwards CCII, Bailey RW (2000) Laparoscopic hernia repair the learning curve. Surg Laparosc Endosc Percutan Tech 10:149–153
Wright D, O’Dwyer PJ (1998) The learning curve for laparoscopic hernia repair. Semin Laparosc Surg 5:227–232. https://doi.org/10.1177/155335069800500405
Liem MSL, Van Steensel CJ, Boelhouwer RU et al (1996) The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg 171:281–285
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403. https://doi.org/10.1007/s10029-009-0529-7
Schouten N, Simmermacher RKJ, Van Dalen T et al (2013) Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? Surg Endosc 27:789–794. https://doi.org/10.1007/s00464-012-2512-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Informed consent
Not applicable.
Conflict of interest
All authors declare to have no conflicts of interest.
Research involving human participants:
The Medical Ethics Committee of our institution (RTPO Leeuwarden) confirmed the conduct of this retrospective study without the need for ethical review, and the institutional board approved the execution of the study without the need for consent in accordance with Dutch regulations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zwols, T.L.R., van der Bilt, A.R.M., Veeger, N.J.G.M. et al. Learning and implementation of TransREctus sheath PrePeritoneal procedure for inguinal hernia repair. Hernia (2024). https://doi.org/10.1007/s10029-024-03031-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-03031-x