Abstract
Purpose
To examine updated evidence on the efficacy and safety of mesh non-fixation in patients undergoing laparo-endoscopic repair of groin hernias.
Methods
We searched MEDLINE, Cochrane Central Library, Embase, ClinicalTrials. gov, and ICTRP databases to identify randomized controlled trials. The primary outcomes were recurrence, chronic pain, and return to daily life. The certainty of evidence (CoE) was assessed by grading recommendations, assessments, developments, and evaluations. We performed a subgroup analysis based on the surgical type. This study was registered with PROSPERO (CRD 42022368929).
Results
We included 25 trials with 3,668 patients (4,038 hernias) were included. Mesh non-fixation resulted in little to no difference in hernia recurrence (relative risk [RR]:1.40, 95% confidence interval [CI]:0.59–3.31; I2 = 0%; moderate CoE) and chronic pain (RR:0.48, 95% CI:0.13–1.78; I2 = 77%; moderate CoE), but reduced return to daily life (mean difference [MD]: − 1.79 days, 95% CI: − 2.79 to –0.80; I2 = 96%; low CoE). In subgroup analyses, the transabdominal preperitoneal approach (TAPP) (MD: − 2.97 days, 95% CI: − 4.87 to − 1.08; I2 = 97%) reduced return to daily life than total extraperitoneal inguinal approach (MD: − 0.24 days, 95% CI − 0.71 to 0.24; I2 = 61%) (p = 0.006).
Conclusions
Mesh nonfixation improves the return to daily life without increasing the risk of hernia recurrence or chronic pain. Surgeons and patients may discuss mesh nonfixation options to accommodate a patient’s desired return to daily life. Further trials focusing on TAPP are required to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Groin hernia repair is one of the most frequently performed general surgical procedures, with > 20 million patients undergoing standby repair worldwide [1]. Of all groin hernias, 96% were inguinal, and 4% were femoral [1]. The estimated lifetime risk of groin hernia repair was 27% in men and 3% in women, respectively [2, 3]. Lichtenstein tension-free hernia repair, is the most commonly performed technique with low recurrence and complication rates [4]. With the advent of innovative surgical platforms, minimally invasive approaches such as laparoscopic transabdominal preperitoneal repair (TAPP), total extraperitoneal repair (TEP), and robotic TAPP have emerged [1, 4, 5]. These minimally invasive approaches have similar wound-related complications, recurrence rates, and a more rapid return to work and activity than the Lichtenstein procedure [6, 7]. However, the recovery time and recurrence after groin hernia repair pose major socioeconomic problems, with chronic pain that interferes with daily life and employment occurring in approximately 6% of patients [8].
Mesh non-fixation is considered a means of avoiding the chronic pain associated with fixation devices; however, the high risk of recurrence is a primary concern among surgeons. Although various mesh fixation strategies exist, and a recent network meta-analysis suggested that absorbable tacks and adhesives may minimize recurrence and complications, no statistically or clinically applicable differences were found between strategies. Recent systematic reviews of mesh non-fixation showed that the risk of recurrence, complications, and postoperative pain did not differ between fixation and non-fixation; however, these reviews did not assess the certainty of evidence (CoE) using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach [9,10,11]. Therefore, the controversy has not subsided, and more randomized controlled trials (RCTs) have addressed this topic [12,13,14].
In this study, we aimed to assess the efficacy and safety of mesh nonfixation in patients who underwent groin hernia repair using the GRADE approach.
Methods
Protocol
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 [15]. The protocol was registered in PROSPERO (CRD 42022368929) and OSF (https://doi.org/10.17605/OSF.IO/RDHGX).
Study selection
This systematic review included RCTs assessing the efficacy of mesh fixation versus non-fixation and excluded non-RCTs. Adults aged ≥ 18 years who underwent laparo-endoscopic repair of groin hernias were included in this systematic review. Participants who could not tolerate a fixed mesh, such as those with metal allergies, were excluded. The intervention involved mesh non-fixation, which included non-fixation or self-gripping. The control was mesh fixation, including tacks, clips, staples, sutures, glue, and cyanoacrylate, as different types of mesh fixation are considered equally effective [16].
The primary outcomes were hernia recurrence, chronic postoperative inguinal pain (CPIP), and the number of days to return to daily life. Hernia recurrence was defined as the number of recurrent hernias of a single hernia on the side that underwent repair as directly diagnosed by an independent healthcare provider. Hernia formation at previously unrepaired or reinforced sites was excluded. CPIP was defined as bothersome moderate pain affecting daily activities, lasting at least 3 months postoperatively and decreasing over time. Days to return to daily life were defined as the period from surgery date to the return to normal daily activities. Secondary outcomes were postoperative pain, length of hospital stay (days), operative time (min), cost (US$), and adverse events. Postoperative pain was defined as the mean visual analog scale (VAS) or numeric rating scale (NRS) score for pain at rest or during activity on postoperative day (POD) 1. The final score was adopted after pain was measured multiple times. Pain at rest and during activity was measured. We modified the protocol to include cost as a secondary outcome.
We searched the following databases for studies published until October 20, 2022, the Cochrane Central Register of Controlled Trials (CENTRAL) using the Cochrane Library (inception–present), MEDLINE using PubMed (1966–present), and EMBASE using ProQuest Dialog (1988–present) (Supplementary 1). We also searched the World Health Organization International Clinical Trials Platform Search Portal (ICTRP) (inception–present) and ClinicalTrials.gov (inception–present) databases for ongoing and unpublished trials (Supplementary 2). We initially searched for studies published before October 20, 2022, and an updated search on May 2, 2023. We checked the reference lists of all eligible studies, including international guidelines [1, 4], and those citing eligible studies. Studies were not excluded based on the observation period, publication year, language, or country restrictions. All papers included published and unpublished articles, conference abstracts, and letters. We asked the authors of the original studies for unpublished or additional data.
Data collection and analysis
Two reviewers (FK and JW) independently screened the titles and abstracts, followed by an assessment of eligibility based on the full text. The same two reviewers (FK and JW) performed independent data extraction and evaluated the risk of bias using the risk of bias tool version 2 [17]. Disagreements were resolved through discussion. If a consensus could not be reached, a third reviewer acted as an arbiter to make the final decision (MK).
We pooled the risk ratio (RR) and 95% confidence intervals (CI) for hernia recurrence and CPIP according to the Cochrane Handbook [18], and the mean differences (MD) and 95% Cis for days to return to daily life, length of hospital stay, and operative time. Furthermore, we pooled the effect estimates using standard mean differences (SMDs) for postoperative pain measured using VAS and NRS. We summarized adverse events based on the definitions in the original article; however, no meta-analysis of adverse events was performed. We conducted an intention-to-treat analysis of the dichotomous data. We did not impute missing data for continuous based on the Cochrane Handbook recommendations [18]. We performed a meta-analysis using the data available in the original study and Review Manager software 5.4.2 (Cochrane Collaboration, London, UK) with a random-effects model.
Statistical heterogeneity was evaluated by visually inspecting forest plots and calculating I2 (0–40% might not be important; 30–60% may represent moderate heterogeneity; 50–90% may represent substantial heterogeneity; and 75–100%, considerable heterogeneity) based on the Cochrane Handbook [18]. The reasons for were assessed when substantial heterogeneity (I2 > 50%) was observed. We performed an extensive literature search of unpublished trials using the Clinical Trial Registry System (ClinicalTrials.gov and ICTRP). Following this, we performed a funnel plot and Egger’s test when ˃10 eligible studies were included in the meta-analysis based on the Cochrane Handbook guidelines [18].
A table summarizing our findings was created based on the Cochrane Handbook [18]. We adopted the corresponding risks from the medians of the included trials. We have included grading to evaluate the CoE based on the GRADE approach for each summary in the findings table [19].
Additional analyses
To clarify the influence of effect modifiers on the results, we conducted subgroup analyses of the primary outcomes based on the following factors: surgical type (TEP or TAPP), anesthesia type (spinal or general), and fixation type (tack, clip, staple, suture, glue, or cyanoacrylate). However, a subgroup analysis of the anesthesia type regarding recurrence and CPIP could not be performed because of the lack of outcomes in spinal anesthesia trials. We modified the protocol to include a subgroup analysis of the mesh type (polypropylene or three-dimensional (3D)/self-gripping mesh).
We performed the following sensitivity analyses of the primary outcomes to assess the robustness of the review results to decisions made during the review process: exclusion of studies with missing data, exclusion of studies in which hernia recurrence was defined according to the original authors’ definition, and exclusion of studies in which CPIP was defined according to the original authors’ definition. However, we could not perform a sensitivity analysis by excluding studies in which hernia recurrence or CPIP was defined according to the original authors’ definition because there were no such trials. We performed a sensitivity analysis to exclude studies that did not meet the criteria for properly designed trials.
Results
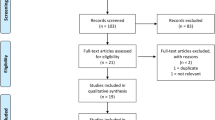
Figure 1 shows a flowchart of trial selection. After removing the duplicate records, 356 records were identified. After screening, we included 25 trials involving 3,668 patients (4,038 total hernias) [12,13,14, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41].
Table 1 presents the characteristics of the eligible studies. Of the 25 trials, 14 employed TEP approaches, and 11 used TAPP approaches. General anesthesia was administered in 16 trials, spinal anesthesia in one, general or spinal anesthesia in one, and unknown anesthesia in seven. Mesh fixation approaches involved staples in six trials, tacks in 14, sutures in one, glue in one, tacks or glue in two, and tacks and sutures in one. A polypropylene mesh was used in 17 trials, a 3D anatomical mesh in two, and a self-gripping mesh in six.
Table 2 displays the risk of bias for recurrence, with 21 trials exhibiting ‘some concerns’ and two trials presenting a ‘high’ risk of bias.
Outcomes
Table 3 summarizes the findings of the GRADE approach.
Primary outcomes
Twenty-three trials reported recurrence [12,13,14, 20,21,22,23,24,25,26,27,28,29,30,31,32, 34, 35, 37,38,39,40,41]. Of these, 13 patients did not experience recurrence. Mesh non-fixation likely resulted in little to no difference in hernia recurrence compared to mesh fixation (RR: 1.40, 95% CI: 0.59–3.31; I2 = 0%; moderate CoE; Fig. 2A).
Nine trials reported on CPIP [12, 13, 22,23,24, 27, 34, 35, 37]. Of these, four trials did not report CPIP [13, 23, 34, 35], and five trials did not report the number of tacks [12, 13, 22, 23, 37]. Mesh non-fixation resulted in little to no difference in CPIP compared with mesh fixation (RR: 0.48, 95% CI: 0.13 to 1.78; I2 = 77%; moderate CoE; Fig. 2B).
Nine trials reported return to daily life [14, 20, 21, 23, 25, 28, 38, 39, 41]. The median return to daily life with mesh fixation was 8 days. Mesh non-fixation may improve return to daily life than mesh fixation (MD: − 1.79 days, 95% CI: − 2.79 to − 0.80; I2 = 96%; low CoE; Fig. 2C).
Secondary outcomes
Twelve trials reported pain on POD 1 [14, 22,23,24, 28, 29, 31, 33,34,35, 38, 40]. Of those, nine used the VAS [14, 22, 23, 29, 33,34,35, 38, 40], and three used the NRS [24, 28, 31]. Mesh non-fixation may reduce pain on POD 1 compared with mesh fixation (SMD: − 0.53 days, 95% CI: − 1.00 to − 0.06; I2 = 93%; low CoE; Fig. 3A).
Thirteen trials reported the length of hospital stay [14, 22,23,24,25, 28, 29, 31, 34, 35, 37,38,39]. Mesh non-fixation may result in little to no difference in the length of hospital stay compared with mesh fixation (MD: − 0.72 days, 95% CI: − 2.10 to 0.66; I2 = 100%; low CoE; Fig. 3B).
Sixteen trials reported operative time [14, 21, 22, 24,25,26, 28, 30,31,32, 34, 35, 37,38,39,40]. Mesh non-fixation may reduce operative time compared with mesh fixation (MD: -2.17 min, 95% CI: − 3.80 to − 0.53; I2 = 94%; low CoE; Fig. 3C).
Seven trials reported costs [20, 22, 26, 32,33,34, 37]. Mesh non-fixation may reduce costs compared with mesh fixation (MD: –324.5 US$, 95% CI: − 451.6 to − 197.4; I2 = 100%; low CoE; Fig. 3D).
Twenty-three trials reported adverse events [12,13,14, 20,21,22,23,24, 26,27,28,29,30,31,32, 34,35,36,37,38,39,40,41]. Seroma, hematoma, and urinary retention were the primary complications. Seroma and hematoma are similar with and without fixation [12,13,14, 20, 21, 23, 24, 27,28,29,30,31,32, 34, 35, 37, 38, 40], whereas mesh non-fixation tends to reduce urinary retention [21, 24, 28, 29, 31, 38].
Additional analyses
We performed subgroup and sensitivity analyses (Supplementary Figs. 1–4). In the subgroup analysis of fixation type, mesh non-fixation reduced CPIP than mesh fixation with glue (RR: 0.14, 95% CI: 0.06–0.34), while mesh non-fixation resulted in little to no difference in CPIP compared with mesh fixation with tacker, staple, or suture (test for subgroup differences, p = 0.004). Mesh non-fixation with TAPP (MD: − 3.84 days, 95% CI: − 6.88 to − 0.80; I2 = 98%) improved the return to daily life than that with TEP (MD: − 0.24, 95% CI:− 0.71 to 0.24; I2 = 61%) (test for subgroup differences, p = 0.02). In the subgroup analysis of anesthesia type, mesh non-fixation with general anesthesia (MD: − 3.03 days, 95% CI: − 5.48 to − 0.58; I2 = 98%) improved return to daily life than that spinal anesthesia (MD: 0.19 days, 95% CI: − 0.29 to 0.67) (test for subgroup differences, p = 0.02). In the subgroup analysis of mesh type, non-fixation with polypropylene mesh (MD: − 1.90 days, 95% CI: − 2.97 to − 0.83; I2 = 97%) improved return to daily life faster than that with 3D or self-gripping mesh (MD: − 0.33 days, 95% CI: − 0.90 to 0.25; I2 = 1%) (test for subgroup differences, p = 0.01). The other subgroup analyses did not differ significantly (test for subgroup differences, p ≥ 0.05). After excluding studies with missing data [13, 21, 23,24,25,26, 28, 31, 37, 38, 40] and those that did not meet the criteria for a properly designed trial [13, 29, 39, 40], sensitivity analyses were consistent with the main results (Supplementary 3). Publication bias was not detected as the funnel plot was symmetrical (Egger’s test, p = 0.785; Supplementary Fig. 5).
Discussion
This systematic review and meta-analysis, including 25 trials with 3,668 patients (4,038 total hernias), demonstrated that mesh non-fixation improved return to daily life without increasing recurrence. However, little to no difference in CPIP was observed. Additionally, it reduced pain on POD 1, operative time, and costs without increasing the incidence of adverse events. This study provides new evidence that mesh non-fixation may improve the return to daily activities; therefore, it is important for surgeons and patients.
Our finding that mesh non-fixation did not increase hernia recurrence is consistent with previous findings [9,10,11]. Up to 2% of hernia recurrence after minimally invasive repair has been reported for TEP and TAPP repairs [1, 6]. Various risk factors for hernia recurrence have been identified, including mesh fixation (tack, clip, staple, suture, or glue), anesthesia type, mesh type, medial or lateral hernia sac, sliding hernia, operative time, registry database participation, femoral hernia, proper dissection and space creation, postoperative complications, and center/surgeon volume [1, 42]. The present meta-analysis included only RCTs; subgroup analyses of anesthesia and fixation type did not reveal any differences. Furthermore, the absence of heterogeneity (I2 = 0%) indicated less variability across studies, providing consistency and reliability of our findings.
The inclusion of a standard polypropylene mesh (> 50 g/m2) and the exclusion of large hernias, especially M3 hernias, according to the European Hernia Society classification, may limit the generalizability of the findings in this study. Notably, the 2018 international guidelines of the HerniaSurge Group recommended mesh fixation in M3 hernias (large medial) to reduce the risk of recurrence in both TEP and TAPP [1]. However, recent experimental and large database studies have suggested that mesh fixation may be unnecessary [43, 44]. Moreover, a recent meta-analysis and large database study reported that using a lightweight mesh (≤ 50 g/m2) in the laparo-endoscopic repair of direct or large inguinal hernias can potentially increase recurrence rates [44, 45]. A heavy mesh (> 70 g/m2) should be used in cases necessitating direct laparo-endoscopic repair of large inguinal hernias [45]. Another important point is that the International Endohernia Society’s guidelines recommend a mesh size of at least 10 × 15 cm2, but for large medial hernias, a larger mesh (i.e. 12 × 17 cm2 or larger) is recommended, independent of the fixation [46]. These are ongoing research areas that will be investigated further in future studies.
By conducting a meta-analysis of twice as many studies and cases as previous reviews [9,10,11], we found that mesh nonfixation improved the return to daily life, particularly in TAPP under general anesthesia. In contrast, previous systematic reviews focusing on TEP [9,10,11] found that mesh non-fixation did not improve return to daily life. The difference in results can be attributed to the present subgroup analysis, which found that TAPP improved the return to daily life compared with TEP. The exact mechanism is unknown; however, a reduction of approximately 1.8 days is critical, considering that the return to daily life did not differ between TEP and TAPP in a previous review [47]. Additionally, we found that mesh nonfixation led to a faster return to daily life with general anesthesia than with lumbar anesthesia. With the increasing incidence of groin hernias in the older population, these findings are clinically relevant, especially considering the recommended use of general anesthesia for patients aged ≥ 65 years [1]. This suggests that mesh nonfixation combined with general anesthesia may provide an optimal approach for groin hernia repair in the older population. However, our finding that nonfixation with a polypropylene mesh improved the return to daily life faster than with 3D or self-gripping meshes was inconsistent with that of a previous review. In the Meshkati Yazd study, return to daily life in the fixation group occurred only at 3 weeks postoperatively, and the results were heavily influenced by those of the mesh-type subgroup [41]. Future trials focusing on TAPP under general anesthesia with a preliminary definition of return to daily life are required to confirm these results.
Consistent with the findings of previous studies, mesh non-fixation did not reduce CPIP [10, 16]. This suggests that the mesh fixation method may not significantly influence the development of chronic pain after groin hernia repair. Therefore, other factors or surgical techniques should be considered to address this issue. One study found a significant correlation between the number of tacks used and the incidence of pain, with six tacks being the cutoff point [26]. In this review, subgroup analysis based on the number of tacks was impossible because many studies did not report this number; however, it may be related to the incidence of pain. Surgery is the main cause of postoperative pain after groin hernia repair due to pubic groin, iliopsoas muscle, or popliteal nerve injuries [48]. Therefore, a multifaceted surgical approach is required to prevent the development of CPIPs.
Our findings concerning postoperative pain, length of hospital stay, operative time, and cost were consistent with those of previous reviews [9,10,11], suggesting that our analysis aligns with prior research in terms of these outcomes and further supports the validity of our results. Moreover, we expand these findings using the GRADE approach to demonstrate low-to-moderate CoEs and provide a more comprehensive understanding of the outcomes.
This study has several limitations. First, although this review included only RCTs, the CoE remained moderate. This may have been due to the limited power and high heterogeneity in some trials. The imprecision and inconsistency of the results may be further refined by adjusting for preoperative patient characteristics (e.g., sex) and hernia characteristics (e.g., primary or bilateral). Second, several confounding factors may have influenced the results, including surgeon experience and expertise, inclusion and exclusion criteria, learning curve, hospital volume, surgical technique, mesh type, fixation technique, outcome reporting, and follow-up duration. These factors should be considered when interpreting the findings of this study. Further studies are required to better understand their impacts on the outcomes of interest.
In conclusion, this systematic review and meta-analysis showed that mesh non-fixation improved the return to daily life without increasing hernia recurrence or chronic pain. Surgeons and patients may discuss the mesh nonfixation option to accommodate the timing of the patient’s desired return to daily life. Further trials focusing on TAPP are required to confirm these findings.
Data availability
All data are available from public databases.
References
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571
Jenkins JT, O’Dwyer PJ (2008) Inguinal hernias. BMJ 336:269–272
National Institute for Health and Care Excellence NICE technology appraisal guidance no. 83: laparoscopic surgery for inguinal hernia repair. https://www.nice.org.uk/guidance/ta83. Accessed 22 May 2023
Waite KE, Herman MA, Doyle PJ (2016) Comparison of robotic versus laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair. J Robot Surg 10:239–244
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23:473–484
Aiolfi A, Cavalli M, Ferraro SD et al (2021) Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg 274:954–961
Fränneby U, Sandblom G, Nordin P et al (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212–219
Eltair M, Hajibandeh S, Hajibandeh S et al (2019) Meta-analysis of laparoscopic groin hernia repair with or without mesh fixation. Int J Surg 71:190–199
Lo C-W, Tsai Y-C, Yang SS-D et al (2019) Comparison of short- to mid-term efficacy of nonfixation and permanent tack fixation in laparoscopic total extraperitoneal hernia repair: a systematic review and meta-analysis. Ci Ji Yi Xue Za Zhi 31:244–253
Sahebally SM, Horan J, Rogers AC, Winter D (2020) Fixation versus no fixation in laparoscopic totally extraperitoneal repair of primary inguinal hernia-a systematic review and meta-analysis of randomized controlled trials. Langenbecks Arch Surg 405:435–443. https://doi.org/10.1007/s00423-020-01899-8
Habeeb TAAM, Mokhtar MM, Sieda B et al (2020) Changing the innate consensus about mesh fixation in trans-abdominal preperitoneal laparoscopic inguinal hernioplasty in adults: Short and long term outcome. Randomized controlled clinical trial. Int J Surg 83:117–124. https://doi.org/10.1016/j.ijsu.2020.09.013
Azevedo MA, de Oliveira GBT, Malheiros CA, Roll S (2022) Are there differences in chronic pain after laparoscopic inguinal hernia repair using the transabdominal technique comparing with fixation of the mesh with staples, with glue or without fixation? A clinal randomized, double-blind trial. Arq Bras Cir Dig 35:e1670. https://doi.org/10.1590/0102-672020220002e1670
Yıldırım MB, Sahiner IT (2023) The effect of mesh fixation on migration and postoperative pain in laparoscopic TEP repair: prospective randomized double-blinded controlled study. Hernia 27:63–70. https://doi.org/10.1007/s10029-022-02587-w
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Techapongsatorn S, Tansawet A, Kasetsermwiriya W et al (2019) Mesh fixation technique in totally extraperitoneal inguinal hernia repair-a network meta-analysis. Surgeon 17:215–224. https://doi.org/10.1016/j.surge.2018.09.002
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.I4898
Higgins JPT TJ Cochrane handbook for systematic reviews of interventions Version 6.3.2022. https://training.cochrane.org/handbook/current. Accessed 17 May 2022
Guyatt G, Oxman AD, Akl EA et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Ferzli GS, Frezza EE, Pecoraro AM Jr, Ahern KD (1999) Prospective randomized study of stapled versus unstapled mesh in a laparoscopic preperitoneal inguinal hernia repair. J Am Coll Surg 188:461–465. https://doi.org/10.1016/s1072-7515(99)00039-3
Smith AI, Royston CM, Sedman PC (1999) Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair a prospective randomized trial. Surg Endosc 13:804–806. https://doi.org/10.1007/s004649901104
Moreno-Egea A, Torralba Martínez JA, Morales Cuenca G, Aguayo Albasini JL (2004) Randomized clinical trial of fixation vs nonfixation of mesh in total extraperitoneal inguinal hernioplasty. Arch Surg 139:1376–1379. https://doi.org/10.1001/archsurg.139.12.1376
Parshad R, Kumar R, Hazrah P, Bal S (2005) A randomized comparison of the early outcome of stapled and unstapled techniques of laparoscopic total extraperitoneal inguinal hernia repair. JSLS 9:403–407
Koch CA, Greenlee SM, Larson DR et al (2006) Randomized prospective study of totally extraperitoneal inguinal hernia repair: fixation versus no fixation of mesh. JSLS 10:457–460
Li JW, Zheng MH, Li HQ et al (2007) A randomized controlled clinical trial comparing stapling with non-stapling of mesh in laparoscopic total extraperitoneal inguinal hernioplasty. Chin J Gen Surg 22:440–442
Taylor C, Layani L, Liew V et al (2008) Laparoscopic inguinal hernia repair without mesh fixation, early results of a large randomised clinical trial. Surg Endosc 22:757–762. https://doi.org/10.1007/s00464-007-9510-7
Bittner R, Schmedt C-G, Leibl BJ, Schwarz J (2011) Early postoperative and one year results of a randomized controlled trial comparing the impact of extralight titanized polypropylene mesh and traditional heavyweight polypropylene mesh on pain and seroma production in laparoscopic hernia repair (TAPP). World J Surg 35:1791–1797. https://doi.org/10.1007/s00268-011-1148-x
Garg P, Nair S, Shereef M et al (2011) Mesh fixation compared to nonfixation in total extraperitoneal inguinal hernia repair: a randomized controlled trial in a rural center in India. Surg Endosc 25:3300–3306. https://doi.org/10.1007/s00464-011-1708-z
Ayyaz M, Farooka MW, Malik AA et al (2015) Mesh fixation vs. non-fixation in total extra peritoneal mesh hernioplasty. J Pak Med Assoc 65:270–272
Claus CMP, Rocha GM, Campos ACL et al (2016) Prospective, randomized and controlled study of mesh displacement after laparoscopic inguinal repair: fixation versus no fixation of mesh. Surg Endosc 30:1134–1140. https://doi.org/10.1007/s00464-015-4314-7
Buyukasik K, Ari A, Akce B et al (2017) Comparison of mesh fixation and non-fixation in laparoscopic totally extraperitoneal inguinal hernia repair. Hernia 21:543–548. https://doi.org/10.1007/s10029-017-1590-2
Li W, Sun D, Sun Y et al (2017) The effect of transabdominal preperitoneal (TAPP) inguinal hernioplasty on chronic pain and quality of life of patients: mesh fixation versus non-fixation. Surg Endosc 31:4238–4243. https://doi.org/10.1007/s00464-017-5485-1
Reddy RRS, Girish TU, Chandra BJS (2017) A prospective comparative study of total extraperitoneal inguinal hernia repair: fixation versus without fixation of the mesh. Int Surg J. https://doi.org/10.18203/2349-2902.isj20164380
Shen Y-M, Liu Y-T, Chen J, Sun L (2017) Efficacy and safety of NBCA (n-butyl-2-cyanoacrylate) medical adhesive for patch fixation in totally extraperitoneal prosthesis (TEP): a prospective, randomized, controlled trial. Eur Rev Med Pharmacol Sci 21:680–686
Abd-Raboh OH, Hablus MA, Elshora AA, Saber SA (2018) Comparative study between mesh fixation vs. non-fixation in totally extraperitoneal hernioplasty for inguinal Hernia. JAMA Surg 6:23–28. https://doi.org/10.11648/j.js.20180601.15
Lau PC, Low KY (2018) Post operative pain in laparoscopic groin hernia repair using a self-gripping mesh versus stapler fixation: a randomized double blinded study. Surg Endosc 32:430–482. https://doi.org/10.1007/s00464-018-6180-6
Wang L, Jin X, Wang H, Zhou X (2018) Laparoscopic transabdominal preperitoneal procedure with and without mesh-fixation for inguinal hernia repairs. Int J Clin Exp Med 11:8651–8655
Kalidarei B, Mahmoodieh M, Sharbu Z (2019) Comparison of mesh fixation and nonfixation in laparoscopic transabdominal preperitoneal repair of inguinal hernia. Formosan J Surgery 52:212
Khalil AA, Ebeid EF, Ismail AI (2019) Comparative study between the use of self-fixating mesh and non-self-fixating mesh in laparoscopic inguinal hernia repair transabdominal preperitoneal technique. Egyptian J Surg 38:588
Zayed ME, Essa MS (2020) Impact of mesh fixation vs non-fixation in laparoscopic transabdominal preperitoneal inguinal hernia repair on chronic groin pain and quality of life: a prospective randomized study. Egyptian J Surg 39:574
Meshkati Yazd SM, Kiany F, Shahriarirad R et al (2023) Comparison of mesh fixation and non-fixation in transabdominal preperitoneal (TAPP) inguinal hernia repair: a randomized control trial. Surg Endosc. https://doi.org/10.1007/s00464-023-10040-x
Siddaiah-Subramanya M, Ashrafi D, Memon B, Memon MA (2018) Causes of recurrence in laparoscopic inguinal hernia repair. Hernia 22:975–986. https://doi.org/10.1007/s10029-018-1817-x
Zamkowski M, Tomaszewska A, Lubowiecka I, Karbowski K, Śmietański M (2023) Is mesh fixation necessary in laparoendoscopic techniques for M3 inguinal defects? An experimental study. Surg Endosc 37:1781–1788. https://doi.org/10.1007/s00464-022-09699-5
Novik B, Sandblom G, Ansorge C, Thorell A (2022) Association of mesh and fixation options with reoperation risk after laparoscopic groin hernia surgery: a Swedish hernia registry study of 25,190 totally extraperitoneal and transabdominal preperitoneal repairs. J Am Coll Surg 234:311–325. https://doi.org/10.1097/XCS.0000000000000060
Bakker WJ, Aufenacker TJ, Boschman JS, Burgmans JPJ (2021) Heavyweight mesh is superior to lightweight mesh in laparo-endoscopic inguinal hernia repair: a meta-analysis and trial sequential analysis of randomized controlled trials. Ann Surg 273:890–899. https://doi.org/10.1097/SLA.0000000000003831
Bittner R, Arregui ME, Bisgaard T et al (2011) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25:2773–2843. https://doi.org/10.1007/s00464-011-1799-6
Aiolfi A, Cavalli M, Del Ferraro S et al (2021) Total extraperitoneal (TEP) versus laparoscopic transabdominal preperitoneal (TAPP) hernioplasty: systematic review and trial sequential analysis of randomized controlled trials. Hernia 25:1147–1157. https://doi.org/10.1007/s10029-021-02407-7
Lange JFM, Kaufmann R, Wijsmuller AR et al (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19:33–43. https://doi.org/10.1007/s10029-014-1292-y
Acknowledgements
None.
Funding
This work was supported by JSPS KAKENHI [grant number JP21K21121 and 23K16289].
Author information
Authors and Affiliations
Contributions
Study concept, FK and JW; study design, FK and JW; statistical analyses, JW; data interpretation, FK, JW, MK, and NS; manuscript preparation, FK and JW; manuscript editing, MK and NS; manuscript review, JW, MK, and NS; literature screening, FK, JW, and MK. All the authors approved the final version of the manuscript and agreed to be accountable for the accuracy and integrity of this work.
Corresponding author
Ethics declarations
Conflicts of interest
Fusympti Kobayashi, MD, Jun Watanabe, MD, PhD, Masaru Koizumi, MD, PhD, and Naohiro Sata, MD, PhD declare that they have no conflict of interest.
IRB approval code and name of the institution
Not applicable.
Ethical approval
Not applicable.
Human and animal rights
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kobayashi, F., Watanabe, J., Koizumi, M. et al. Efficacy and safety of mesh non-fixation in patients undergoing laparo-endoscopic repair of groin hernia: a systematic review and meta-analysis. Hernia 27, 1415–1427 (2023). https://doi.org/10.1007/s10029-023-02919-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02919-4