Abstract
Purpose
The use of laparoscopy for paediatric inguinal hernia repairs has increased significantly over the past 2 decades. However, there is significant variation in the reported recurrence rates in the literature, with many studies reporting higher rates than the open operation. This may be explained by the range of different techniques currently included under the term laparoscopic inguinal hernia repair. The purpose of this study is to determine whether dividing the hernia sac before ligation improves surgical outcomes following a paediatric laparoscopic inguinal hernia repair compared to ligation alone.
Methods
A systematic review of the literature was performed following PRISMA guidelines of all studies reporting the outcomes following paediatric laparoscopic inguinal hernia repair where the technique was recorded as laparoscopic suture ligation alone (LS) or laparoscopic sac division and suture ligation (LSDS). Studies were assessed for risk of bias and exclusion criteria included reported follow-up of less than 6 months.
Results
A total of 8518 LS repairs and 6272 LSDS repairs were included in the final analysis. LSDS repair was associated with a significantly lower recurrence rate (odds ratio 0.51, 95% CI 0.36–0.71, p = 0.001). There was no significant difference in the rates of testicular ascent or atrophy.
Conclusion
Recreating the open operation by hernia sac division followed by suture ligation significantly reduces the risk of hernia recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most frequently performed operations in pediatric practice, with more than 6000 in children under the age of 16 years in England alone in 2019 [1]. The traditional ‘open’ inguinal herniotomy remains the most commonly utilized technique worldwide but since the 1990s there has been growing use of laparoscopy [2,3,4]. This provides the potential benefits of reduced post-operative pain and quicker recovery, but more importantly has the advantage of visualizing the contralateral deep inguinal ring [5,6,7,8,9]. Yet, it has not achieved the universal acceptance seen with other procedures, such as laparoscopic cholecystectomy which may partly be due to a concern that recurrence rates are higher than those for the open operation thus negating any potential benefits [10, 11].
However, the term laparoscopic hernia repair is used to describe a range of different techniques which may explain the variation in the recurrence rates reported in the literature [11,12,13,14,15,16]. Despite the heterogeneity in technique, the majority of studies can be broadly divided into two groups: those that replicate the open operation by dividing then ligating the sac versus those that simply ligate it. As with much of the pediatric surgical literature, many of these studies are limited to case series or small, non-randomized comparative studies, making it difficult to draw any firm conclusions.
Therefore, the aim of this study is to perform a systematic review of the literature on pediatric laparoscopic inguinal hernia repairs, to determine whether replication of the open operation (i.e. laparoscopic complete sac dissection and suture (LSDS) cligation) leads to decreased rates of recurrence compared to laparoscopic suture (LS) ligation alone.
Methods
Search strategy
This study protocol was designed according to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) 2020 guidelines [17]. The complete EMBASE and MEDLINE databases were searched from inception until November 2020 using the Medical Subject Headings (MeSH) terms “Inguinal” AND “Hernia” OR “Herniotomy” AND “Laparoscopy” OR “Laparoscopic”. For the population we used the terms “Child” or “Pediatric” or “Paediatric”. Papers selected were restricted to those published in English.
All abstracts identified were then screened by two independent investigators based on our inclusion and exclusion criteria (Table 1).
Although in the initial selection phase all papers reporting outcomes from laparoscopic intracorporeal sutured ring closure were included, for detailed analysis only those papers in which the technique was described as either LSDS or LS and the results were clearly attributable to the individual techniques were kept. The technique of LSDS was defined as complete dissection of the hernial sac at the level of the internal ring, followed by suture ligation of the ring. If the internal ring was ligated with a suture, without division of the sac the technique was classified as a LS ligation. Reference lists of identified articles were manually searched to identify additional studies.
The quality of individual studies was assessed independently by two investigators (AG and CV) using the MINORS criteria [18] for all studies apart from randomized controlled studies (RCTs) for which the ROB-2 assessment tool was used [19]. The MINORS score was chosen as a validated method of identifying and assessing non-randomized surgical studies. Similarly, the ROB-2 assessment tool is appropriately validated for randomized controlled studies. In the case of a discrepancy of more than 2 points between investigators, a final decision was made by the senior authors.
Data extraction
All included studies were analyzed to extract study characteristics (including country, study design and sample size), population characteristics (age, technique) outcomes (recurrence rates, testicular atrophy/ascent) and any reported post-operative complications. Data extraction was performed independently by AG and CV and any discrepancies resolved by the senior author.
Statistical analysis
Due to the significant heterogeneity and the lack of trials comparing the two techniques formal meta-analysis was not possible. Data are presented as median (interquartile range) unless otherwise stated. Pooled analysis of non-parametric data was performed using Chi-square with Yates correction. Statistical significance was defined as p < 0.05.
Results
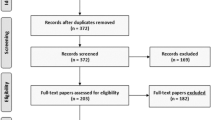
The initial search returned 998 abstracts after duplicates were removed (Fig. 1). After full review, only 46 met the full-text inclusion criteria and were selected for final analysis [4, 9,10,11,12, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62]. These studies included 8 randomized control trials (RCTs), including 2 RCTs comparing LSDS and LS techniques, 3 prospective comparative studies, 5 prospective non-comparative studies, 13 retrospective comparative and 14 retrospective non-comparative which leaves 3 cohort studies (Table 2).
Study quality was reasonable for the comparative studies with a median MINORS score of 16/24 (IQR14-17) and slightly lower for the non-comparative studies with a median score of 10 (IQR 9–10) (Figs. 2–3). A total of 8 non-comparative papers (6 cohort and 3 retrospective cohort studies) were excluded because of poor methodology (taken as a MINORS score of less than 50%). Reason for exclusion was predominantly due to a combination of unmentioned/unclear follow-up period, failure to achieve the targeted follow-up of 95% of the patients, and inclusion of non-consecutive patients.
Following assessment with the RoB-2 tool 5 of 8 RCTs were reported as having a high risk of potential bias. This was often due to the blinding/control methodology used and was not thought to impact on the reporting of recurrence outcomes. Therefore, these studies remained included in the final analysis. Full results of the methodological analysis are included in Supplemental Tables 1, 2, and 3.
In total, these studies included 12555 patients, of which 5520 were in the LSDS group, undergoing 6272 hernia repairs and 7035 in the LS group undergoing 8518 hernia repairs. Study characteristics and patient demographics are reported in Table 1. Median reported follow-up was 22.9 months (15.5–30).
Recurrence rates
In total, there were 45/6272 (0.7%) recurrences in the LSDS group compared to 120/8518 (1.4%) in the LS group, this gives an odds ratio of 0.51 (95% CI 0.36–0.71), p = 0.001. However, as the overall recurrence rate remains low, the absolute risk reduction is 0.8% (95% CI 0.48–1.12%) and a number to treat of 125 (95% CI 89.4–206.6).
Testicular atrophy/ascent
In the LSDS group, 7 studies (401 patients) reported testicular atrophy as an outcome with no cases of atrophy identified. However, no significant difference was identified between the two groups—2 cases reported in 16 studies (3842 patients) in the LS group (p = 1).
With regard to testicular ascent, 8 LSDS studies (2201 patients) reported outcomes for testicular ascent in which 2 cases were identified. Again, no difference was seen between the techniques, with 2 cases in 11 studies (2119 patients) in the LS group (P = 0.68). In addition, 6 patients required a later orchidopexy for an undescended testicle identified but not treated at the time of the original hernia repair.
Discussion
The potential benefits of utilizing a laparoscopic approach for the management of pediatric inguinal hernias, such as to treat metachronous hernias, has prompted many surgeons to develop techniques that provide this benefit without increasing morbidity [5,6,7,8,9]. As such, there are a large number of papers reporting outcomes under the label of a ‘laparoscopic hernia repair.’ However, the umbrella term ‘laparoscopic inguinal hernia repair’ is used to described a wide range of approaches, including sutureless, LS and LSDS repairs [8, 9, 63]. This may explain the significant variation in complication rates reported in the literature [4, 9,10,11,12, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62] and makes subsequent comparison of studies difficult. This study is the first systematic review to compare two strict definitions to determine whether recreating the open operation—performing a herniotomy before ligating the sac (LSDS) is superior to ligating the sac alone (LS).
The quality of the current literature remains mixed, with large numbers of small studies with inconsistent outcome reporting. Many studies do not provide enough detail of the actual technique and had to be discarded with many more reporting outcomes within weeks of the operation and therefore at high risk of missing recurrences. Furthermore, additional but important outcomes, such as testicular atrophy and ascent are rarely reported.
Despite strict inclusion criteria, the risk of bias in most studies was moderate, this was predominantly due to the lack of comparative groups and small study size. Further potential limitations include the failure to separate study populations out into different risk groups, such as premature infants. However, the size of the combined groups should minimize the effect of these subgroups in the overall analysis.
Despite these issues, we identified a significant reduction in the risk of recurrence associated with the LSDS repair; however, it must be said that the overall recurrence rate remains low for both techniques. This difference may be explained by the reliance of the LS technique on a single suture. If that suture fails, or as is the case in some studies resorbs, then the open hernial sac is still present and the hernia recurs. However, in the LSDS group performing a herniotomy prior to closure provides a second layer of protection.
There are some who suggest that cutting the sac may increase the risk of vas or vessel injury [64] and there is certainly an increased technical challenge in safely dissecting the sac in small infants. These outcomes are poorly reported by many of the included studies and we cannot comment on whether there is a significant learning curve to achieve good results, as it was outside the study parameters. However, we did not identify any increased risk of testicular atrophy associated with sac dissection and in the authors’ experience [65], we have not found this to be an issue whether the procedure is performed by an experienced surgeon or surgeon in training.
The laparoscopic approach has been found to be associated with lower rates of testicular ascent compared to the open repair; however, the reason why remains unclear [66]. We had postulated that division of the sac would further prevent the testis from becoming tethered to the sutured internal ring and therefore being at risk of subsequent ascent, i.e. that the LSDS repair would be associated with a lower rate of ascent. However, we were unable to identify a significant difference between the groups. Again, thorough analysis was limited by the lack of long-term active follow-up in the papers to specifically address this issue.
This study was limited to intraperitoneal LS repairs only, but there has been increased interest in laparoscopically assisted extraperitoneal repairs. The suggested benefit of the laparoscopic assisted extraperitoneal techniques is reduced operative time and improved cosmetic results [20, 21, 67, 68]. Although both techniques close the ring, we did not include them in this analysis as we felt the approach was too different. A recent systematic review was published comparing intraperitoneal vs extraperitoneal hernia repairs [69]; however, this still included a number of different techniques (both LS and LSDS) in both groups and had no minimum follow-up period, thus making an accurate determination of recurrence rates difficult. A further review would be needed to fully address the extraperitoneal technique; however, as the basis of the operation is the same we would anticipate that without sac disruption the recurrence rate would remain higher than for an LSDS repair.
Although there is a 50% reduction in recurrence rate between the two techniques this only equates to an actual reduction of 0.7% as the overall recurrence rate remains low for both techniques. The LS technique has tens of reported modifications and has widely reported low recurrence rates. However, this is a high volume procedure, in England alone in 2019, 6491 children had an inguinal hernia repair. Therefore, if a technique like the LSDS that is based on recreating the open technique is to be adopted as the procedure of choice for laparoscopic hernia repairs, then hundreds of children could potentially avoid redo operations worldwide each year.
Setting standards and comparing outcomes between individual centers is always difficult in pediatric surgical practice, given that the volume of individual cases is often low and this is compounded further when complication rates are low. However, this study identified an overall recurrence rate of < 1% for over 6000 LSDS hernia repairs. We suggest that this should be the outcome towards which surgeons should be aiming for in their practice and one that other techniques should be tested against when conducting large studies.
Conclusion
The LSDS technique for the repair of pediatric inguinal hernias is a safe technique which has the benefits of a laparoscopic repair while replicating the steps of the open operation. This review identified a significant reduction in recurrence rate when it was compared to the LS technique, but the studies included -especially RCTs—had moderate to high risk of bias. Large-scale multicentric prospective RCTs are needed for good quality results and to decrease confounding factors.
Data Availability
All study data is available on request.
References
NHS Digital. [Hospital episode statistics website]. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics. Accessed 10 Sep 2021
Alzahem A (2011) Laparoscopic versus open inguinal herniotomy in infants and children: a meta-analysis. Pediatr Surg Int 27:605–612. https://doi.org/10.1007/s00383-010-2840-x
Gause C, Casamassima M, Yang J et al (2017) Laparoscopic versus open inguinal hernia repair in children ≤3: a randomized controlled trial. Pediatr Surg Int 33:367–376. https://doi.org/10.1007/s00383-016-4029-4
Koivusalo A, Korpela R, Wirtavuori K et al (2009) A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 123:332–337. https://doi.org/10.1542/peds.2007-3752
Lee Y, Liang J (2002) Experience with 450 cases of microlaparoscopic herniotomy in infants and children. Pediatr Endosurg Innov Tech 6:25–28. https://doi.org/10.1089/10926410252832410
Schier F, Montupet P, Esposito C (2002) Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 37:395–397. https://doi.org/10.1053/jpsu.2002.30842
Clarke S (2010) Pediatric inguinal hernia repair and hydrocele: an evidence-based review in the era of minimal access surgery. J Laparoendosc Adv Surg Tech A 20:305–309. https://doi.org/10.1089/lap.2010.9997
Davies D, Rideout D, Clarke S (2020) The international pediatric endosurgery group evidence-based guideline on minimal access approaches to the operative management of inguinal hernia in children. J Laparoendosc Adv Surg Tech A 30(2):221–227. https://doi.org/10.1089/lap.2016.0453
Almetaher H, Hassan H, Effat A et al (2020) Laparoscopic repair of congenital inguinal hernia: a comparative study between purse-string suture and peritoneal disconnection with ligation techniques in bilateral cases. J Pediatr Endosc Surg 2:83–89. https://doi.org/10.1007/s42804-020-00052-y
Boo Y, Han H, Ji W et al (2012) Laparoscopic hernia sac transection and intra-corporeal ligation show very low recurrence in pediatric inguinal hernia. J Laparoendosc Adv Surg Tech A 22:720–723. https://doi.org/10.1089/lap.2012.0040
Abd-Alrazek M, Alsherbiny Mahfouz H et al (2017) Laparoscopic pediatric inguinal hernia repair: a controlled randomised study. J Pediatr Surg 52:1539–1544. https://doi.org/10.1016/j.jpedsurg.2017.07.003
Becmeur F, Phillipe P, Lemandat-Schultz A et al (2004) A continuous series of 96 laparoscopic inguinal hernia repair in children by a new technique. Surg Endosc 18:1738–1741. https://doi.org/10.1007/s00464-004-9008-5
Tsai Y, Wu C, Yang S (2007) Minilaparoscopic herniorraphy with hernia sac transection in children and young adults: a preliminary report. Surg Endosc 21:1623–1625. https://doi.org/10.1007/s00464-007-9207-y
Giseke S, Glass M, Tapadar P et al (2010) A true laparoscopic herniotomy in children: evaluation of long term outcome. J Laparoendosc Adv Surg Tech A 20(2):191–194. https://doi.org/10.1089/lap.2009.0069
Ostlie D, Ponksy T (2014) Technical options of the laparoscopic pediatric inguinal hernia repair. J Laparoendosc Adv Surg Tech A 24(3):194–198. https://doi.org/10.1089/lap.2014.0081
Svetanoff W, Fraser J, Briggs K et al (2021) A single institution experience with laparoscopic hernia repair in 791 children. J Pediatr Surg 56:1185–1189. https://doi.org/10.1016/j.jpedsurg.2021.02.021
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):71. https://doi.org/10.1136/bmj.n71
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 28(366):l4898. https://doi.org/10.1136/bmj.l4898
Shalaby R, Ismail M, Dorgham A et al (2010) Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg 45(11):2210–2216. https://doi.org/10.1016/j.jpedsurg.2010.07.004
Wang F, Liu S, Shen Y, Chen J (2018) A comparative study of the single-site laparoscopic herniorrhaphy using needle instruments and double-site laparoscopic herniorrhaphy in the minimally invasive treatment of inguinal hernias in children. Exp Ther Med 15(3):2896–2900. https://doi.org/10.3892/etm.2018.5756
Borkar NB, Pant N, Ratan S et al (2012) Laparoscopic repair of indirect inguinal hernia in children: does partial resection of the sac make any impact on outcome? J Laparoendosc Adv Surg Tech A 22(3):290–294. https://doi.org/10.1089/lap.2011.0259
Elbatarny AM, Khairallah MG, Elsayed MM et al (2020) Laparoscopic repair of pediatric inguinal hernia: disconnection of the hernial sac versus disconnection and peritoneal closure. J Laparoendosc Adv Surg Tech A 30(8):927–934. https://doi.org/10.1089/lap.2018.0679
Esposito C, Montinaro L, Alicchio F et al (2010) Laparoscopic treatment of inguinal hernia in the first year of life. J Laparoendosc Adv Surg Tech A 20(5):473–476. https://doi.org/10.1089/lap.2009.0323
Esposito C, Montinaro L, Alicchio F et al (2009) Technical standardization of laparoscopic herniorraphy in pediatric patients. World J Surg 33(9):1846–1850. https://doi.org/10.1007/s00268-009-0121-4
Lee SR, Park PJ (2019) Laparoscopic reoperation for pediatric recurrent inguinal hernia after previous laparoscopic repair. Hernia 23(4):663–669. https://doi.org/10.1007/s10029-018-1840-y
Lee SR, Park PJ (2021) Adding iliopubic tract repair to high ligation reduces recurrence risk in pediatric laparoscopic transabdominal inguinal hernia repair. Surg Endosc 35(1):216–222. https://doi.org/10.1007/s00464-020-07382-1
Montupet P, Esposito C (2011) Fifteen years experience in laparoscopic inguinal hernia repair in pediatric patients results and considerations on a debated procedure. Surg Endosc 25(2):450–453. https://doi.org/10.1007/s00464-010-1188-6
Pant N, Aggarwal SK, Ratan SK (2014) Laparoscopic repair of hernia in children: comparison between ligation and nonligation of sac. J Indian Assoc Pediatr Surg 19(2):76–79. https://doi.org/10.4103/0971-9261.129597
Shalaby R, Abd Alrazek M, Elsaied A et al (2018) Fifteen years experience with laparoscopic inguinal hernia repair in infants and children. J Laparoendosc Adv Surg Tech A 28(1):101–105. https://doi.org/10.1089/lap.2017.0269
Tsai YC, Wu CC, Yang SS (2010) Open versus minilaparoscopic herniorrhaphy for children: a prospective comparative trial with midterm follow-up evaluation. Surg Endosc 24(1):21–24. https://doi.org/10.1007/s00464-009-0645-6
Van Batavia JP, Tong C, Chu DI et al (2018) Laparoscopic inguinal hernia repair by modified peritoneal leaflet closure: description and initial results in children. J Pediatr Urol 14(3):272.e1-272.e6. https://doi.org/10.1016/j.jpurol.2018.02.015
Wheeler AA, Matz ST, Schmidt S et al (2011) Laparoscopic inguinal hernia repair in children with transperitoneal division of the hernia sac and proximal purse string closure of peritoneum: our modified new approach. Eur J Pediatr Surg 21(6):381–385. https://doi.org/10.1055/s-0031-1291181
Lin CD, Tsai YC, Chang SJ et al (2011) Surgical outcomes of mini laparoscopic herniorrhaphy in infants. J Urol 185(3):1071–1076. https://doi.org/10.1016/j.juro.2010.10.044
Esposito C, Escolino M, Cortese G et al (2017) Twenty-year experience with laparoscopic inguinal hernia repair in infants and children: considerations and results on 1833 hernia repairs. Surg Endosc 31(3):1461–1468. https://doi.org/10.1007/s00464-016-5139-8
Hasanein A, Rabea M, Fathi M et al (2017) Laparoscopic purse-string suture sac closure is appropriate procedure for children with unilateral indirect inguinal hernia: comparative study versus laparoscopic sac excision and closure procedure. Egyptian J Surg 36:394–400. https://doi.org/10.4103/ejs.ejs_62_17
Shehata SM, Attia MA, Attar AAE et al (2018) Algorithm of laparoscopic technique in pediatric inguinal hernia: results from experience of 10 years. J Laparoendosc Adv Surg Tech A 28(6):755–759. https://doi.org/10.1089/lap.2017.0273
Esposito C, Turial S, Escolino M et al (2012) Laparoscopic inguinal hernia repair in premature babies weighing 3 kg or less. Pediatr Surg Int 28(10):989–992. https://doi.org/10.1007/s00383-012-3156-9
Ho IG, Ihn K, Koo EJ et al (2018) Laparoscopic repair of inguinal hernia in infants: comparison with open hernia repair. J Pediatr Surg 53(10):2008–2012. https://doi.org/10.1016/j.jpedsurg.2018.01.022
Geiger S, Bobylev A, Schädelin S et al (2017) Single-center, retrospective study of the outcome of laparoscopic inguinal herniorrhaphy in children. Medicine 96(52):e9486. https://doi.org/10.1097/md.0000000000009486
Koivusalo A, Pakarinen MP, Rintala RJ (2007) Laparoscopic herniorrhaphy after manual reduction of incarcerated inguinal hernia. Surg Endosc 21(12):2147–2149. https://doi.org/10.1007/s00464-007-9318-5
Koivusalo AI, Korpela R, Wirtavuori K et al (2009) A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 123(1):332–337. https://doi.org/10.1542/peds.2007-3752
Lee DY, Baik YH, Kwak BS et al (2015) A purse-string suture at the level of internal inguinal ring, taking only the peritoneum leaving the distal sac: is it enough for inguinal hernia in pediatric patients? Hernia 19(4):607–610. https://doi.org/10.1007/s10029-015-1348-7
Lee SR, Choi SB (2017) The efficacy of laparoscopic intracorporeal linear suture technique as a strategy for reducing recurrences in pediatric inguinal hernia. Hernia 21(3):425–433. https://doi.org/10.1007/s10029-016-1546-y
Li S, Tang ST, Aubdoollah TH et al (2015) A modified approach for inguinal hernias in children: hybrid single-incision laparoscopic intraperitoneal ligation. J Laparoendosc Adv Surg Tech A 25(8):689–693. https://doi.org/10.1089/lap.2014.0474
Marte A, Sabatino MD, Borrelli M et al (2009) Decreased recurrence rate in the laparoscopic herniorrhaphy in children: comparison between two techniques. J Laparoendosc Adv Surg Tech A 19(2):259–262. https://doi.org/10.1089/lap.2008.0292
Montupet P, Esposito C (1999) Laparoscopic treatment of congenital inguinal hernia in children. J Pediatr Surg 34(3):420–423. https://doi.org/10.1016/s0022-3468(99)90490-6
Pastore V, Bartoli F (2015) Neonatal laparoscopic inguinal hernia repair: a 3-year experience. Hernia 19(4):611–615. https://doi.org/10.1007/s10029-014-1269-x
Schier F (2006) Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg 41(6):1081–1084. https://doi.org/10.1016/j.jpedsurg.2006.02.028
Schier F, Montupet P, Esposito C (2002) Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 37(3):395–397. https://doi.org/10.1053/jpsu.2002.30842
Shalaby R, Desoky A (2002) Needlescopic inguinal hernia repair in children. Pediatr Surg Int 18(2–3):153–156. https://doi.org/10.1007/s003830100655
Shalaby R, Ismail M, Samaha A et al (2014) Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg 49(3):460–464. https://doi.org/10.1016/j.jpedsurg.2013.10.019
Steven M, Carson P, Bell S et al (2016) Simple purse string laparoscopic versus open hernia repair. J Laparoendosc Adv Surg Tech A 26(2):144–147. https://doi.org/10.1089/lap.2014.0276
Turial S, Saied A, Schier F (2011) Microlaparoscopic hernia repair in children: initial experiences. Surg Innov 18(4):368–372. https://doi.org/10.1177/1553350611406742
Turial S, Enders J, Krause K et al (2011) Laparoscopic inguinal herniorrhaphy in babies weighing 5 kg or less. Surg Endosc 25(1):72–78. https://doi.org/10.1007/s00464-010-1132-9
Rahman FU, Rahman IU, Amin H (2019) Laparoscopic treatment of inguinal hernia in children, an experience of purse string at the level of deep ring. J Med Sci 27(2):111–115
Walsh CM, Ng J, Saxena AK (2020) Comparative analysis of laparoscopic inguinal hernia repair in neonates and infants. Surg Laparosc Endosc Percutan Tech 30(5):459–463. https://doi.org/10.1097/sle.0000000000000815
Yildiz A, Çelebi S, Akin M et al (2012) Laparoscopic herniorrhaphy: a better approach for recurrent hernia in boys? Pediatr Surg Int 28(5):449–453. https://doi.org/10.1007/s00383-012-3078-6
Wang F, Zhong H, Shou T et al (2019) Single-site laparoscopic percutaneous extraperitoneal closure versus modified transumbilical two-port laparoscopic suturing of the hernia sac for the treatment of pediatric inguinal hernia: comparison of the outcomes of two different approaches. J Laparoendosc Adv Surg Tech A 29(1):103–108. https://doi.org/10.1089/lap.2018.0405
Shou T, Zhong H, Wang F (2018) Trans-umbilical two-port laparoscopic suturing of the inguinal hernia defect with percutaneous assistance: a safe and efficient scarless surgery for pediatric inguinal hernia repair. Hernia 22(4):681–684. https://doi.org/10.1007/s10029-018-1749-5
Kozlov Y, Novozhilov V (2015) Technology of single-incision laparoscopic surgery in treatment of inguinal hernia in small babies. J Laparoendosc Adv Surg Tech A 25(6):526–530. https://doi.org/10.1089/lap.2014.0206
Karadag GA, Erginel B, Sever N et al (2016) Laparoscopic hernia repair in children: which method is the best? J Exp Clin Med 33(1):11–13. https://doi.org/10.5835/jecm.omu.33.01.004
Marte A, De Rosa L, Pintozzi L et al (2019) Toward sutureless laparoscopic inguinal hernia repair in children? Pediatr Med Chir. https://doi.org/10.4081/pmc.2019.167
Zani A, Eaton S, Hoellwarth M et al (2014) Management of pediatric inguinal hernias in the era of laparoscopy: results of an international survey. Eur J Pediatr Surg 24(1):9–13. https://doi.org/10.1055/s-0033-1354586
Ducey J, Peters RT, Wilkinson DJ et al (2021) Laparoscopic inguinal herniotomy: recreating the open operation optimises outcomes. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2021.10.042
Feng S, Zhao L, Liao Z et al (2015) Open versus laparoscopic inguinal herniotomy in children: a systematic review and meta-analysis focusing on postoperative complications. Surg Laparosc Endosc Percutan Tech 25(4):275–280. https://doi.org/10.1097/sle.0000000000000161
Uchida H, Kawashima H, Goto C et al (2010) Inguinal hernia repair in children using single-incision laparoscopic-assisted percutaneous extraperitoneal closure. J Pediatr Surg 45(12):2386–2389
Rahman UF (2018) Comparison of single port and three port laparoscopic technique of inguinal hernia repair in children. Pak J Med Res 57(4):181–188
Maat S, Dreuning K, Nordkamp S et al (2021) Comparison of intra- and extra-corporeal laparoscopic hernia repair in children: a systematic review and pooled data-analysis. J Pediatr Surg 56(9):1647–1656. https://doi.org/10.1016/j.jpedsurg.2021.01.049
Funding
There were no sources of funding to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ayman Goneidy, Christian Verhoef, Nick Lansdale, Robert T Peters and David J Wilkinson declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goneidy, A., Verhoef, C., Lansdale, N. et al. Laparoscopic hernia repair in children: does recreating the open operation improve outcomes? A systematic review. Hernia 27, 1037–1046 (2023). https://doi.org/10.1007/s10029-023-02772-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02772-5