Abstract
Purpose
Chronic postoperative inguinal pain (CPIP), a complication of inguinal hernia repair, may negatively affect mental health. The rates of psychological disorders in patients with CPIP are unknown. We aimed to describe the prevalence of psychological disorders coinciding with CPIP.
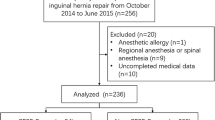
Methods
A retrospective chart review was performed of all patients seen at the Cleveland Clinic Center for Abdominal Core Health’s inter-disciplinary Chronic Groin Pain Clinic. This clinic is unique in that all patients are evaluated by a surgeon, a sonographer and radiologist, and a behavioral medicine psychologist. Patient psychological history and treatment, Depression Anxiety and Stress Scale (DASS) scores, pain catastrophizing, and trauma or abuse history were captured.
Results
From January 2018 to January 2022, 61 patients were evaluated and included in the study. Psychological treatment had been provided to 37 (61%) patients (present: 16 (27%), past: 21 (35%)). The most common psychological disorders represented were depression (N = 13, 22%), anxiety (N = 10, 17%), and post-traumatic stress disorder (N = 5, 8%). DASS scores indicated that 20 (33%) patients were reporting symptoms of depression and 16 (27%) patients were reporting symptoms of anxiety. Of the 40 patients assessed for pain catastrophizing, 28 (70%) reported rumination, 9 (23%) reported magnification, and 23 (58%) reported feelings of helplessness. A childhood history of emotional or physical abuse was reported by 11 (18%) patients.
Conclusion
An inter-disciplinary groin pain clinic has revealed that patients with CPIP frequently have pre-existing complex psychosocial issues. A multi-specialty approach to CPIP may improve preoperative assessments and identify patients who may benefit from further psychological evaluation and treatment.
Similar content being viewed by others
References
Nguyen DK, Amid PK, Chen DC (2016) Groin pain after inguinal hernia repair. Adv Surg 50(1):203–220. https://doi.org/10.1016/j.yasu.2016.04.003
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625. https://doi.org/10.1016/S0140-6736(06)68700-X
Fafaj A, Tastaldi L, Alkhatib H, Zolin S, Alaedeen D, Petro C, Prabhu AS, Rosenblatt S, Rosen MJ, Krpata DM (2020) Surgical treatment for chronic postoperative inguinal pain—short term outcomes of a specialized center. Am J Surg 219(3):425–428. https://doi.org/10.1016/j.amjsurg.2019.10.020
Kalliomaki ML, Sandblom G, Gunnarsson U, Gordh T (2009) Persistent pain after groin hernia surgery: a qualitative analysis of pain and its consequences for quality of life. Acta Anaesthesiol Scand 53(2):236–246. https://doi.org/10.1111/j.1399-6576.2008.01840.x
Fine PG (2011) Long-term consequences of chronic pain: mounting evidence for pain as a neurological disease and parallels with other chronic disease states. Pain Med 12(7):996–1004. https://doi.org/10.1111/j.1526-4637.2011.01187.x
Dobscha SK, Corson K, Perrin NA, Hanson GC, Leibowitz RQ, Doak MN, Dickinson KC, Sullivan MD, Gerrity MS (2009) Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA 301(12):1242–1252. https://doi.org/10.1001/jama.2009.377
Courtney CA, Duffy K, Serpell MG, O’Dwyer PJ (2002) Outcome of patients with severe chronic pain following repair of groin hernia. Br J Surg 89(10):1310–1314. https://doi.org/10.1046/j.1365-2168.2002.02206.x
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Washington
Henry JD, Crawford JR (2005) The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 44(2):227–239. https://doi.org/10.1348/014466505X29657
Pollard CA (1984) Preliminary validity study of the pain disability index. Percept Mot Skills 59(3):974. https://doi.org/10.2466/pms.1984.59.3.974
Pain disability index. https://www.med.umich.edu/1info/FHP/practiceguides/pain/detpdi.pdf Accessed 15 April 2022
Sullivan MJL (1995) The pain catastrophizing scale: user manual. https://aspecthealth.ca/wp-content/uploads/2017/03/PCSManual_English1.pdf Accessed 15 April 2022
Darnall BD, Sturgeon JA, Cook KF, Taub CJ, Roy A, Burns JW, Sullivan M, Mackey SC (2017) Development and validation of a daily pain catastrophizing scale. J Pain 18(9):1139–1149. https://doi.org/10.1016/j.jpain.2017.05.003
Terlizzi EP, Zablotsky B (2019) Mental health treatment among adults: United States, 2019. NCHC Brief no. 380, September 2020. https://www.cdc.gov/nchs/products/databriefs/db380.htm#:~:text=Interview%20Survey%2C%202019.-,Summary,from%20a%20mental%20health%20professional Accessed 30 Mar 2022
Major depression. National institute of mental health. https://www.nimh.nih.gov/health/statistics/major-depression Accessed 30 Mar 2022
Any anxiety disorder. National institute of mental health. https://www.nimh.nih.gov/health/statistics/any-anxiety-disorder#part_2579 Accessed 30 Mar 2022
Villarroel MA, Terlizzi EP (2019) Symptoms of depression among adults: United States, 2019. Centers for disease control and prevention. https://www.cdc.gov/nchs/products/databriefs/db379.htm Accessed 30 Mar 2022
Terlizzi EP, Villarroel MA (2019) Symptoms of generalized anxiety disorder among adults: United States, 2019. Centers for disease control and prevention. https://www.cdc.gov/nchs/products/databriefs/db378.htm Accessed 30 Mar 2022
Kind S, Otis JD (2019) The interaction between chronic pain and PTSD. Curr Pain Headache Rep 28(23):91. https://doi.org/10.1007/s11916-019-0828-3
Post-traumatic stress disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/statistics/post-traumatic-stress-disorder-ptsd Accessed 30 Mar 2022
Siqveland J, Hussain A, Lindstrøm JC, Ruud T, Hauff E (2017) Prevalence of posttraumatic stress disorder in persons with chronic pain: a meta-analysis. Front Psychiatry 8:1–8. https://doi.org/10.3389/fpsyt.2017.00164
Lampe A, Doering S, Rumpold G, Solder E, Krismer M, Kantner-Rumplmair W, Schubert C, Sollner W (2003) Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res 54(4):361–367. https://doi.org/10.1016/S0022-3999(02)00399-9
Wildeman C, Emanuel N, Leventhal JM, Putnam-Hornstein E, Waldfogel J, Lee H (2014) The prevalence of confirmed maltreatment among US children, 2004 to 2011. JAMA Pediatr 168(8):706–713. https://doi.org/10.1001/jamapediatrics.2014.410
Leung L (2012) Pain catastrophizing: an updated review. Indian J Psychol Med 34(3):204–217. https://doi.org/10.4103/0253-7176.106012
Kneeland ET, Griffin ML, Taghian N, Weiss RD, McHugh RK (2019) Associations between pain catastrophizing and clinical characteristics in adults with substance use disorders and co-occurring chronic pain. Am J Drug Alcohol Abuse 45(5):488–494. https://doi.org/10.1080/00952990.2019.1581793
Sansone RA, Sansone LA (2012) Rumination. Innov Clin Neurosci 9(2):29–34
Staal E, Nienhuijs SW, Keemers-Gels ME, Rosman C, Strobbe LJA (2008) The impact of pain on daily activities following open mesh inguinal hernia repair. Hernia 12:153–157. https://doi.org/10.1007/s10029-007-0297-1
Rusu AC, Santos R, Pincus T (2016) Pain-related distress and clinical depression in chronic pain: a comparison between two measures. Scand J Pain 12:62–67. https://doi.org/10.1016/j.sjpain.2016.04.001
Arnow BA, Blasey CM, Constantino MJ, Robinson R, Hunkeler E, Lee J, Fireman B, Khaylis A, Feiner L, Hayward C (2011) Catastrophizing, depression, and pain-related disability. Gen Hosp Psychiatry 33(2):150–156. https://doi.org/10.1016/j.genhosppsych.2010.12.008
Kaye AD, Kandregula S, Kosty J, Sin A, Guthikonda B, Ghali GE, Craig MK, Pham AD, Reed DS, Gennuso SA, Reynolds RM, Ehrhardt KP, Cornett EM, Urman RD (2020) Chronic pain and substance use disorders: preoperative assessment and strategies. Best Pract Res Anaesthesiol 34(2):255–267. https://doi.org/10.1016/j.bpa.2020.04.014
Key substance use and mental health indicators in the United States: results from the 2019 National survey on drug use and health. https://www.samhsa.gov/data/sites/default/files/reports/rpt29393/2019NSDUHFFRPDFWHTML/2019NSDUHFFR090120.htm Accessed 1 April 2022
Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chaou SP, Jung J, Zhang H, Smith SM, Pickering RP, Huang B, Hasin DS (2016) Epidemiology of DSM-5 drug use disorder: results from the national epidemiological survey on alcohol and related conditions-III. JAMA Psychiat 73(1):39–47. https://doi.org/10.1001/jamapsychiatry.2015.2132
Author information
Authors and Affiliations
Contributions
BTM contributed to study design, data acquisition and interpretation, manuscript writing, and final approval. JS, CCP, LRAB, ASP, MJR, and DMK contributed to study design, data interpretation, manuscript revision, and final approval.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ajita S. Prabhu is a consultant for Verb Surgical and CMR Surgical. She has also been a speaker for and has received grant support from Intuitive Surgical. Dr. Michael J. Rosen receives salary support as medical director of the Abdominal Core Health Quality Collaborative and is a board member of Ariste Medical with stock options. Drs. Benjamin T. Miller, Judith Scheman, Clayton C. Petro, Lucas R. A. Beffa, and David M. Krpata have no conflicts of interest or financial ties to disclose.
Human and animal rights and Informed consent
The Cleveland Clinic Foundation Institutional Review Board reviewed and approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miller, B.T., Scheman, J., Petro, C.C. et al. Psychological disorders in patients with chronic postoperative inguinal pain. Hernia 27, 35–40 (2023). https://doi.org/10.1007/s10029-022-02662-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02662-2



