Abstract
Objective
To assess mesh behaviour and clinical outcomes of open complex abdominal wall reconstruction (CAWR) with the use of a polypropylene reinforced tissue matrix.
Methods
A multicenter retrospective study of adult patients who underwent open CAWR with the use of a permanent polypropylene reinforced tissue matrix (OviTex®) between June 2019 and January 2021.
Results
Fifty-five consecutive patients from four hospitals in the Netherlands were analysed; 46 patients with a ventral hernia and 9 patients with an open abdomen. Most patients with a ventral hernia had one or more complicating comorbidities (91.3%) and one or more complicating hernia characteristics (95.7%). Most procedures were performed in a (clean) contaminated surgical field (69.6% CDC 2–4; 41.3% CDC 3–4). All nine patients with an open abdomen underwent semi-emergent surgery. Twelve out of 46 patients with a ventral hernia (26.1%) and 4 of 9 patients with an open abdomen (44.4%) developed a postoperative surgical site infection that made direct contact with the mesh as confirmed on computed tomography (CT), suspicious of mesh infection. No patient needed mesh explantation for persistent infection of the mesh. During a median follow-up of 13 months, 4 of 46 ventral hernia patients (8.7%) developed a CT confirmed hernia recurrence.
Conclusion
Polypropylene reinforced tissue matrix can withstand infectious complications and provides acceptable mid-term recurrence rates in this retrospective study on open complex abdominal wall reconstructions. Longer follow-up data from prospective studies are required to determine further risk of hernia recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ventral incisional hernia is a common complication of open abdominal surgery. A recent meta-analysis of 35 studies demonstrated that its incidence ranges between 2 and 69%, heavily dependent on study design, type of assessment, and duration of follow-up. For midline laparotomies the 1 year incisional hernia incidence was 12% [1]. Mesh reinforcement has shown to reduce the risk of a recurrent hernia and has become the standard of care in abdominal wall reconstruction (AWR) for incisional hernia [2]. Synthetic mesh has low purchase costs but if a surgical site infection (SSI) spreads towards the mesh, it frequently becomes infected with the subsequent need to be surgically removed [3]. As a result, surgeons have become reserved in using permanent synthetic mesh in patients that are at high risk of developing a SSI, e.g., patients with high-risk comorbidities or patients with contaminated hernia sites.
Although several new types of mesh have been developed, it remains an ongoing discussion which mesh to use best in patients that are at high risk of infectious complications [4, 5]. Biologic meshes are derived from decellularized human or animal tissue. Their main advantage is that they can be used in contaminated surgical fields and seldom require explantation following an infectious complications [6]. Their purchase costs are, however, extremely high and recurrence rates are disappointing [7, 8]. This was confirmed by a recently published randomized controlled trial that compared use of bovine biologic mesh with synthetic mesh in retrorectus position in clean-contaminated and contaminated hernia repair, demonstrating a significantly higher hernia recurrence rate for bovine biologic mesh at 2 years after surgery [9]. Biosynthetic meshes are composed of different resorbable polymers. Compared to biologic meshes, biosynthetics cost less and seem to provide a more durable repair when used in complex reconstructions. Long-term data are, however, limited, and recent data show that not all types of biosynthetics can withstand infection [10, 11].
OviTex® (TELA Bio, Inc, Malvern, PA, USA) is a reinforced tissue matrix. It consists of biologic material that is derived from ovine rumen and processed into a multi-layered extracellular matrix (ECM). The ECM is permeable to fluid shifts and serves as a temporary scaffold for tissue ingrowth and remodelling of the native abdominal wall. The ECM is interwoven with polymer fibers—either polypropylene (permanent) or polyglycolic acid (resorbable) —that provide additional strength whilst minimizing the foreign body reaction as these fibers consist of only 5% of the mesh. Preclinical research shows that the implantation of OviTex® in a primate model is associated with an initial inflammatory response, followed by collagen deposition, tissue integration and remodelling of the abdominal wall [12]. Data on the use of OviTex® mesh in human AWR are very limited [13]. Two studies that investigate the use of OviTex® in open ventral hernia repair report low hernia recurrence rates (0–6%) and no mesh related complications [14, 15]. Although these results seem promising, further data on OviTex® are lacking. Especially when used in patients that are at high risk of developing an infectious complication, it is interesting to see whether this hybrid mesh can indeed withstand infection or that it requires to be removed because of persistent infection. The aim of this study was therefore to investigate mesh behaviour and clinical outcomes of open complex abdominal wall reconstruction with the use of a polypropylene reinforced tissue matrix.
Methods
Study design
This multicenter study was conducted in four teaching hospitals in the Netherlands. These hospitals were selected as they performed five or more open complex abdominal wall reconstructions (CAWR) with the use of OviTex®. Data were retrospectively retrieved from the electronic patient charts using a predefined data extraction sheet. Data items and definitions were standardized to ensure data were collected universally. Approval from the Institutional Review Board of all participating centers was obtained. This study is reported following the Reporting of Observational Studies in Epidemiology (STROBE) statement [16].
Inclusion criteria
Adult patients who underwent abdominal wall reconstruction with a permanent polypropylene reinforced tissue matrix (OviTex®) for a ventral abdominal wall defect or closure of an open abdomen were eligible for inclusion. Patients who underwent parastomal hernia repair were not included. All patients gave informed consent for use of their data.
Data items
Preoperative data included: age, gender, body mass index (BMI), smoking status, diabetes mellitus (DM), cardiac disease (other than hypertension), chronic obstructive pulmonary disease (COPD), history of an abdominal wound infection, use of immunosuppressive and anticoagulative medication, presence of stomata (any kind), intestinal fistula(s), infected mesh, previous abdominal surgery and hernia repair, preoperative botulinum toxin injections (BTA), transverse hernia width measured on computed tomography (CT) (cm), and loss of domain (LOD) measured on CT using the method described by Sabbagh [17]. The preoperative risk of surgical site occurrences (SSO) and hernia recurrence was assessed using the modified Ventral Hernia Working Group (mVHWG) grading scale [18], and the Hernia Patient Wound (HPW) classification system [19]. The latter is more comprehensive, as it also incorporates the transverse hernia width. The level of complexity of all reconstructions was also classified into minor, moderate, and major according to expert consensus as described by Slater et al. [20].
Procedural data included: procedural status (emergency or elective), concomitant procedures, wound classification (according to CDC criteria) [21], component separation techniques (anterior component separation (ACS) or transversus abdominis release (TAR)), type and number of OviTex®, position with respect to the layers of the abdominal wall (only, inlay, retromuscular, preperitoneal or intra-abdominal), use of additional other mesh, anterior and posterior fascial closure, major skin/wound reconstruction, and postoperative negative pressure wound therapy (NPWT).
Outcome variables
The assessed clinical outcomes were the incidence of SSI in direct contact with the mesh (suspicious of acute mesh infection), mesh excision for persistent infection, SSI, SSO, SSO requiring procedural intervention (SSOPI), hospital stay (days), hernia recurrence, and mortality.
Surgical site infection in direct contact with the mesh was defined as a SSI that made direct contact with the mesh, CT confirmed. Surgical site infections were divided into superficial, deep and organ space according to the CDC criteria [21]. SSO were divided into SSI, hematoma/seroma, wound dehiscence, soft tissue ischemia, intestinal fistula, and clinically exposed or infected mesh [22].
Due to the COVID pandemic (2020–2021) we did not routinely invite patients for clinical assessment of their abdominal wall. Via telephone questionnaire, all patients were asked if they thought that a hernia recurrence had developed, if they felt pain, or felt or saw bulging at the site of the scar. A negative reply to these questions has a negative predictive value of 94% for hernia recurrence [23]. Only patients with symptoms possibly indicating a hernia recurrence were assessed by physical examination. Hernia recurrence was subsequently confirmed by CT.
Surgical technique
Because this study involved patients from four different hospitals and was conducted retrospectively, no standardized treatment algorithm was used. All patients were treated according to local preferences, with respect to preoperative patient optimizing, surgical technique, and postoperative care. Certain aspects, however, were similar for all patients. This included the use of preoperative antibiotic prophylaxis and an open surgical approach. When present, bioburden was reduced by excision of non-viable tissue and existing mesh, and resection of enterocutaneous or enteroatmospheric fistulas. The polypropylene reinforced tissue matrix was preferably positioned intra-abdominal or retromuscular. Component separation techniques were performed whenever deemed indicated by the surgeon to achieve midline fascial closure, and to avoid a bridged repair whenever possible. Separation of the posterior fascia from the rectus muscle, creating the retromuscular space for mesh positioning was not scored as CST.
Analysis
Numerical data are summarized and expressed as mean and standard deviation (SD) or median and interquartile range (IQR) depending on normality. Normality was checked by plotting a frequency distribution. Categorical data are summarized as count and percentage. Follow-up time was measured from the day of surgery to the day of the telephone questionnaire, or the last outpatient visit for deceased patients. Being different disease entities, patients with a ventral hernia and patients with an open abdomen were analysed separately.
Results
Fifty-five consecutive patients operated between June 2019 and January 2021 were analysed; 46 patients with a ventral hernia and 9 patients with an open abdomen. Using the complexity classification described by Slater et al. [20] we found that 2 patients (3.6%) had a minor complex hernia, 17 patients (30.9%) a moderate complex hernia, and 36 patients (65.5%) a major complex hernia. A summary overview of the preoperative patient characteristics, procedural data, and postoperative wound complications/clinical outcomes is presented in the online supplementary material 1. To illustrate the types of patients that were included this study, three cases with a complex abdominal wall defect, their preoperative CT scan, and clinical outcomes are presented in the online supplementary material 2.
Ventral hernia
Forty-six patients underwent a ventral hernia repair; all repairs were open procedures. (Table 1) More than half (54.3%) had a previous abdominal wound infection, seventeen patients (37.0%) an intestinal fistula, and seven patients (15.2%) an infected mesh. The median preoperative hernia width was 8.9 cm (IQR 5.3–16.3). As such, most patients had one or more complicating comorbidities (91.3%) and one or more complicating hernia characteristics (95.7%).
A concomitant intra-abdominal procedure was performed in 31 patients (67.4%). (Table 2) Thirty-two of 46 procedures (69.6%) were performed in a to some extent contaminated surgical field (CDC 2–4); 41.3% contaminated / dirty sites (CDC 3 or 4). Most meshes were positioned intra-abdominal (56.5%) or retromuscular (37.0%). With the use of preoperative BTA injections in 24 patients (52.2%), and a CST in 22 patients (47.8%), closure of the anterior fascia was achieved in 35 patients (76.1%).
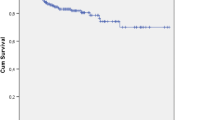
Twenty-one patients (45.7%) developed a SSI within 30 days after surgery. (Table 3) Twelve of 46 patients (26.1%) developed a SSI that made direct contact with the mesh, confirmed by CT. Twenty-nine patients (63.0%) developed one or more SSOPI; 10 patients (21.7%) underwent opening or debridement of the wound, and 23 patients (50%) underwent percutaneous drainage for a symptomatic sterile or infected collection. Not one patient needed mesh explantation for persistent infection involving the mesh. At a median follow-up of 13 months (IQR 9.0–17.0), 4 of 46 patients (8.7%) had developed a CT confirmed hernia recurrence. (Fig. 1) One of 8 patients (12.5%) who underwent a bridging repair developed a recurrent hernia, whereas 3 of 38 patients (7.9%) who underwent primary fascial closure with mesh reinforcement developed a recurrent hernia. The median time at which the recurrences were diagnosed was 4.5 months (IQR 1.1 – 9.5).
Cumulative hernia recurrence rate of the patients undergoing a ventral hernia repair. During a median follow-up of 13 months the recurrence rate was 4/46 (8.7%). The median time to recurrence was 4.5 months. One of the nine patients (11.1%) that underwent closure of an open abdomen developed an incisional hernia (patients with an open abdomen are not included in this figure)
Four patients (8.7%) had deceased at follow-up. Three patients died within 30 days after surgery due to respiratory insufficiency and cardiac ischemia. One patient died 5 months after surgery from a persistent bowel obstruction with no desire for further treatment.
Open abdomen
Nine patients underwent semi-emergency closure of an open abdomen. These procedures were performed in clean (66.7%) or clean-contaminated (33.3%) surgical fields. The mesh was positioned intra-abdominal in all cases, and closure of the anterior fascia was achieved in 6 of 9 patients (66.7%).
Five patients (55.6%) developed a SSI within 30 days after surgery. Four of nine patients (44.4%) developed a CT confirmed SSI that made direct contact with the mesh, and four patients (44.4%) had a SSOPI. None of the patients had their mesh removed for persistent infection of the mesh. At a median follow-up of 10 months (IQR 8.5–14.0), 1 patient (11.1%) had a CT confirmed incisional hernia, that was diagnosed 4 months after surgery. Two patients (22.2%) had deceased at follow-up. One patient died within 30 days after surgery due to repository insufficiency, and one patient died 9 months after surgery from metastatic disease.
Discussion
This study investigated mesh behaviour and clinical outcomes of open complex abdominal wall reconstruction with the use of a polypropylene reinforced tissue matrix. We found that—although a considerable number of patients developed a surgical site infection that made direct contact with the mesh—no mesh needed to be removed for persistent infection. After a median follow-up of 13 months, 8.7% of the patients with a ventral hernia had developed a CT confirmed recurrence.
The relative high rate of SSI and SSO can be seen as a direct consequence of the level of complexity of the patients and their hernia. The vast majority had at least one complicating comorbidity or complicating hernia characteristic, and more than one out of three repairs were performed in a contaminated or dirty setting (CDC 3–4). This wound complication rate is consistent with the observed rate in our recently published study investigating a similar cohort of patients undergoing CAWR with the use of biosynthetic mesh, being 55.7% [10]. Comparably, a wound complication rate of 50% is reported in a pooled analysis of ten studies with somewhat less complicated patients undergoing clean–contaminated and potentially contaminated hernia repairs [24].
Surgical site infection and SSO are frequently reported outcomes in ventral hernia studies. Preoperative optimizing of modifiable risk factors, such as smoking cessation, diabetes control, and weight reduction in overweight patients, has shown to greatly reduce the risk of wound complications [25, 26]. When it comes to the investigation of a specific mesh, it is questionable to what degree a certain mesh affects these short-term outcomes, and if it does, the relevance of these outcomes. Importantly, in patients that are at high risk of developing a wound complication, reports of outcomes that reflect how a certain mesh behaves when it comes in contact with an infection—for example frequency of SSO needing intervention, mesh infection and mesh excision—are much needed.
Comparison with other studies that investigate a specific type of mesh is difficult and should be done with caution for several reasons. Different studies use different ways to preoperatively classify the level of complexity. For instance, the four graded Ventral Hernia Working Group grade and its modified three graded version are used interchangeably, which can easily lead to incorrect interpretations [18, 27]. Reporting and interpretation of levels of complexity vary, which further hampers comparability. Studies investigating the use of a certain mesh perform different surgical techniques, with different mesh positions, with or without component separation techniques, and different duration of follow-up. Furthermore, the definition of fascial closure is inconsistent and may be defined by closing the anterior- or posterior fascia only, or both. Finally, reporting of postoperative wound complications following AWR lacks standardization and direct comparison of published studies is, therefore, frequently not suitable. Differences in SSO rates may also be explained by differences in registration of complications. Experts propose that future studies should report at least the standardized definitions SSI, SSO, and SSOPI [22, 28].
Keeping the difficulty of comparing different mesh studies in mind, two previous studies have assessed outcomes of reinforced tissue matrix as a mesh used in complex abdominal wall reconstruction. The BRAVO study, a prospective, single arm, multicenter study, investigates patients that either have one or more comorbidities or a (potentially) contaminated hernia site [15]. From the first 76 patients that completed the 12 months follow-up, 3% developed a hernia recurrence and not one patient required mesh explantation for infection. Furthermore, from the first 20 patients that completed the 2 year follow-up, no patient developed a recurrence [29]. In the BRAVO study, however, only 20% of repairs have been performed in potentially contaminated surgical fields (CDC 2 or higher).
Another study retrospectively compares 50 patients with reinforced tissue matrix to 50 patients with permanent synthetic mesh in open ventral hernia repair [14]. The proportion of patients with complicating comorbidities (modified VHWG 2), contaminated hernia sites (modified VHWG 3), and type of surgical repair including component separation rates and mesh position is comparable with present study. With 70% of patients from the reinforced tissue matrix group undergoing a concomitant procedure versus only 10% of patients in the synthetic mesh group, the former group has a longer hospital stay, readmission, and SSO (36 vs 22%). Strikingly, among patients who develop a SSO, use of a reinforced tissue matrix is associated with a significantly lower risk of hernia recurrence compared to the use of a synthetic mesh (17 versus 55%, p = 0.048). The incidence of mesh removal is not reported. The hernia recurrence rate with reinforced tissue matrix is 6% after 12 months, which is comparable to our present results (8.7%).
Conservative treatment of infected synthetic mesh has a high failure rate. Depending on the specific type of mesh, the majority (84%) will need to be removed [3]. As such, Kao et al. proposed an algorithm for the management of infected mesh. Salvage of the mesh is only recommended for lightweight polypropylene mesh; all other types of mesh should be explanted. In line with this, Carbonell et al. retrospectively evaluated clinical outcomes of 100 patients who underwent ventral hernia repair with a lightweight polypropylene synthetic mesh in contaminated fields [30]. Eleven patients developed a superficial and/or deep SSI. Whether or not these infections made direct contact with the mesh is not reported, however, at 1 year follow-up there were no mesh removals because of mesh infection. A recently published randomized controlled trial, performed by the same group, compared synthetic mesh with bovine biologic mesh in clean-contaminated and contaminated ventral hernia repair in retrorectus position. The cumulative 2 year hernia recurrence rate was significantly lower in the synthetic mesh group (5.6 vs 20.5%). Interestingly, there was no difference in SSI, SSOPI and mesh removals between both groups. If these results can be extrapolated to the most complex patients, e.g., dirty wound (CDC 4) and bridged repairs, needs to be investigated.
Several studies with relatively large sample sizes have investigated mid-term and long-term outcomes of biologic mesh [6, 8, 31, 32] and biosynthetic mesh [10, 33,34,35,36] used to repair complex and contaminated abdominal wall defects. Not one study on biologic mesh reports a single necessity for mesh removal. With follow-up times between 7 and 24 months recurrence rates are high, varying between 13.0 and 31.3%. Biosynthetic meshes seem to do better. With follow-up times between 20 and 36 months, hernia recurrence rates vary between 5.7 and 17.9%. Recent data, however, indicate that long-term degradable biosynthetic mesh is not always able to withstand infection and may require removal [10, 11].
In the present study, the median time at which the five recurrences were diagnosed was 4.5 months. This is interesting because the major part (95%) of OviTex® consists of resorbable biologic tissue. In an animal model is shown that the biologic material is fully resorbed 6 months after implantation, and diffuse tissue integration with collagen deposition and blood vessel infiltration is seen [12]. This implies that reinforced tissue matrix fully remodels the local abdominal wall approximately 6 months after surgery with only 5% synthetic component left. Whether or not this new native abdominal wall is able to withstand the daily applied forces to the abdominal wall or that recurrence rates will increase over time, as is the case for both biologic and biosynthetic mesh, needs to be clarified by longer follow-up data.
The main strength of this study is that we provide a comprehensive and detailed description of the included patients. For patient characteristics, we report the presence of individual comorbidities but also the preoperative risk of developing a wound complication using the modified VHWG and HPW classification. Clinical outcomes are reported using the standardized variables SSI, SSO, SSOPI, and hernia recurrence. This is important because it makes it possible to pool and/or compare results with other studies. Furthermore, we used a prespecified data extraction form with standardized variables and definitions which ensures comparability of data between participating centers. A major limitation of this study is its retrospective design. Standardised inclusion criteria regarding patient characteristics (for instance level of contamination), preoperative patient optimizing (for instance the use of botulinum toxin), as well as the performed surgical techniques (for instance the use of CST, mesh position and use of NPWT) were absent. Second, although the multicenter design provided the opportunity to report on a real-life clinical practice cohort of fifty-five patients, which is relatively large for studies specifically investigating one type of mesh, clinical heterogeneity was high. Third, our follow-up by telephone questionnaire is only mid-term follow-up and may be less accurate to assess the actual recurrence rate; longer follow-up data after 1 year from prospective studies are needed. Another limitation is the absence of patient reported outcome measures. A key question that is put forward more and more is how abdominal wall reconstruction affects the patients’ quality of life, and which parameter reflects this outcome best. The absence of a recurrence is frequently used to express a successful repair. Although, without patient reported outcome measures it is uncertain whether a patient who repeatedly visits the emergency department for an ongoing wound complication is better off than a patient with a (asymptomatic) hernia recurrence.
In this study high rates of SSI, SSO, and SSOPI were seen. The most frequently performed procedural intervention was radiological drainage for either a sterile or infected collection adjacent to the reinforced tissue matrix. Seeing these data, in the Amsterdam UMC we started soaking the mesh in a gentamycin solution (240 mg / 400 mL) just before implantation and rinsing the wound with the remnant solution. Furthermore, we extended the use of subcutaneous quilting sutures and the presence of subfascial and subcutaneous suction drains.
Conclusion
This study investigated clinical outcomes of open complex abdominal wall reconstruction with the use of permanent polypropylene reinforced tissue matrix (OviTex®). None of the patients with a surgical site infection that made direct contact with the mesh needed mesh explantation for persistent infection involving the mesh. As such, this hybrid mesh seems to be able to withstand infectious complications and provide acceptable mid-term recurrence rates. Although the retrospective design introduced high level of clinical heterogeneity, this study presents clinical outcomes of actual daily practice. Longer follow-up data from prospective studies are required to determine further risk of hernia recurrence.
References
Stabilini C et al (2022) An evidence map and synthesis review with meta-analysis on the risk of incisional hernia in colorectal surgery with standard closure. Hernia. https://doi.org/10.1007/s10029-021-02555-w
Luijendijk RW et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398
Kao AM et al (2018) Prevention and treatment strategies for mesh infection in abdominal wall reconstruction. Plast Reconstr Surg 142(3 Suppl):149S-155S
Costa A et al (2019) Biological scaffolds for abdominal wall repair: future in clinical application? Materials (Basel) 12(15):2375
Lak KL, Goldblatt MI (2018) Mesh selection in abdominal wall reconstruction. Plast Reconstr Surg 142(3 Suppl):99S-106S
Itani KM et al (2012) Prospective study of single-stage repair of contaminated hernias using a biologic porcine tissue matrix: the RICH Study. Surgery 152(3):498–505
Huntington CR et al (2016) Biologic mesh in ventral hernia repair: outcomes, recurrence, and charge analysis. Surgery 160(6):1517–1527
Rosen MJ et al (2013) A 5-year clinical experience with single-staged repairs of infected and contaminated abdominal wall defects utilizing biologic mesh. Ann Surg 257(6):991–996
Rosen MJ et al (2022) Biologic vs synthetic mesh for single-stage repair of contaminated ventral hernias: a randomized clinical trial. JAMA Surg. https://doi.org/10.1001/jamasurg.2021.6902
Claessen JJM et al (2021) Outcomes of mid-term and long-term degradable biosynthetic meshes in single-stage open complex abdominal wall reconstruction. Hernia 25:1647–1657
Van Rooijen MMJ et al (2021) Slowly resorbable biosynthetic mesh: 2-year results in VHWG grade 3 hernia repair. Hernia 26:131–138
Overbeck N et al (2020) In-vivo evaluation of a reinforced ovine biologic: a comparative study to available hernia mesh repair materials. Hernia 24:1293–1306
Sawyer M, Ferzoco S, DeNoto G (2021) 3rd, A polymer-biologic hybrid hernia construct: review of data and early experiences. Polymers (Basel) 13(12):1928
Parker MJ et al (2020) A novel biosynthetic scaffold mesh reinforcement affords the lowest hernia recurrence in the highest-risk patients. Surg Endosc 35:5173–5178
DeNoto G et al (2021) 3rd A Prospective, single arm, multi-center study evaluating the clinical outcomes of ventral hernias treated with OviTex((R)) 1S permanent reinforced tissue matrix: the BRAVO study 12-month analysis. J Clin Med 10(21):4998
von Elm E et al (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Sabbagh C et al (2011) Peritoneal volume is predictive of tension-free fascia closure of large incisional hernias with loss of domain: a prospective study. Hernia 15(5):559–565
Kanters AE et al (2012) Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am Coll Surg 215(6):787–793
Novitsky YW (2016) Hernia surgery. Springer, Cham
Slater NJ et al (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18(1):7–17
Mangram AJ et al (1999) Guideline for prevention of surgical site infection, 1999. Centers for disease control and prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control 27(2):97–132 (quiz 133-4; discussion 96)
DeBord J et al (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia 22(5):737–738
Sneiders D et al (2020) Incisional hernia cannot be diagnosed by a patient-reported diagnostic questionnaire. J Surg Res 245:656–662
Atema JJ, de Vries FE, Boermeester MA (2016) Systematic review and meta-analysis of the repair of potentially contaminated and contaminated abdominal wall defects. Am J Surg 212(5):982-995.e1
Liang MK et al (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265(1):80–89
Petro CC, Prabhu AS (2018) Preoperative planning and patient optimization. Surg Clin North Am 98(3):483–497
Ventral Hernia Working Group et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148(3):544–558. https://doi.org/10.1016/j.surg.2010.01.008
Haskins IN et al (2018) A call for standardization of wound events reporting following ventral hernia repair. Hernia 22(5):729–736
DeNoto, o.b.o.t.B.s.g. (2020) Final outcomes of the initial 20 subjects reaching 2 year follow up in the BRAVO ventral hernia study. Poster presented at: Americas Hernia society annual meeting. September 25th, virtual meeting
Carbonell AM et al (2013) Outcomes of synthetic mesh in contaminated ventral hernia repairs. J Am Coll Surg 217(6):991–998
Atema JJ et al (2017) Major complex abdominal wall repair in contaminated fields with use of a non-cross-linked biologic mesh: a dual-institutional experience. World J Surg 41(8):1993–1999
Diaz JJ Jr et al (2009) Multi-institutional experience using human acellular dermal matrix for ventral hernia repair in a compromised surgical field. Arch Surg 144(3):209–215
Rosen MJ et al (2017) Multicenter, prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: The COBRA study. Ann Surg 265(1):205–211
Roth JS et al (2021) Prospective, multicenter study of P4HB (Phasix) mesh for hernia repair in cohort at risk for complications: 3-year follow-up. Ann Med Surg (Lond) 61:1–7
Levy AS et al (2021) Poly-4-hydroxybutyrate (Phasix) mesh onlay in complex abdominal wall repair. Surg Endosc 35(5):2049–2058
Messa, C.A.t, et al (2019) When the mesh goes away: an analysis of poly-4-hydroxybutyrate mesh for complex hernia repair. Plast Reconstr Surg Glob Open 7(11):e2576
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
A.S. Timmer, J.J.M. Claessen, I.M. Brouwer de Koning, S.M. Haenen, E.J.T. Belt, A.J.N.M. Bastiaansen, E.G.G. Verdaasdonk, C.P. Wolffenbuttel, W.H. Schreurs and W.A. Draaisma declare no conflicts of interest. M.A. Boermeester reported receiving institutional grants from J and J/Ethicon, KCI/3 M, and New Compliance; and being a speaker and/or instructor for KCI/3 M, J and J/Ethicon, BD Bard, Gore, GD Medical, Medtronic, TELABio, and Smith and Nephew.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Written informed consent was obtained from all patients reported in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Timmer, A.S., Claessen, J.J.M., Brouwer de Koning, I.M. et al. Clinical outcomes of open abdominal wall reconstruction with the use of a polypropylene reinforced tissue matrix: a multicenter retrospective study. Hernia 26, 1241–1250 (2022). https://doi.org/10.1007/s10029-022-02604-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-022-02604-y