Abstract
Purpose
To sum all available evidence regarding mesh or mesh fixation material intestinal erosion following inguinal hernia repair and identify the parameters that lead to early (< 6 months) versus late (> 6 months) symptom presentation.
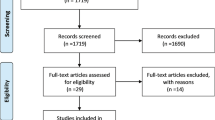
Methods
A systematic literature search of the MEDLINE, Scopus and Google Scholar databases was undertaken to identify relevant studies published up to June 2020.
Results
A total of 54 case reports or cases series, incorporating 57 intestinal erosions were identified. Overall, 13 patients (23%) experienced early intestinal erosions occurring during the first 6 postoperative months while the remaining 44 events (67%) occurred after 6 months. Patients presented most commonly with symptoms of acute obstruction (n = 18, 31.5%), followed by signs of a palpable inguinal mass in 15 patients (26.3%). The late presentation group exhibited significantly more cases of mesh erosion when compared to the early presentation group (100% versus 46.2%, respectively, p < 0.001). Conversely, early presenting cases were more often associated with mesh fixation material erosion (53.8% versus 6.8% in the late group, p < 0.001) and were more likely to develop symptoms of acute intestinal obstruction (61.5% versus 22.8%, p = 0.01). An open primary procedure was more common in late presenting cases (65.9% versus 7.7%, p < 0.001) while early presentation was linked to minimally invasive primary procedures (92.3% versus 34.2%, p < 0.001). Bowel resection was more frequently required in late presenting cases (84.1% versus 46.2%, p = 0.009).
Conclusions
Intestinal erosion from prosthetic material is a rare complication of hernia repair leading to considerable morbidity. Prompt operative repair is key in avoiding catastrophic consequences.




Similar content being viewed by others
References
Rastegarpour A, Cheung M, Vardhan M et al (2016) Surgical mesh for ventral incisional hernia repairs: understanding mesh design. Plast Surg (Oakville, Ont) 24:41–50. https://doi.org/10.4172/plastic-surgery.1000955
Baylón K, Rodríguez-Camarillo P, Elías-Zúñiga A et al (2017) Past, present and future of surgical meshes: a review. Membranes (Basel) 7:47. https://doi.org/10.3390/membranes7030047
Elango S, Perumalsamy S, Ramachandran K, Vadodaria K (2017) Mesh materials and hernia repair. BioMedicine 7:16. https://doi.org/10.1051/bmdcn/2017070316
Gavriilidis P, Davies RJ, Wheeler J et al (2019) Total extraperitoneal endoscopic hernioplasty (TEP) versus Lichtenstein hernioplasty: a systematic review by updated traditional and cumulative meta-analysis of randomised-controlled trials. Hernia 23:1093–1103. https://doi.org/10.1007/s10029-019-02049-w
Wu JJ, Way JA, Eslick GD, Cox MR (2018) Transabdominal Pre-peritoneal versus open repair for primary unilateral inguinal hernia: a meta-analysis. World J Surg. https://doi.org/10.1007/s00268-017-4288-9
Cunningham HB, Weis JJ, Taveras LR, Huerta S (2019) Mesh migration following abdominal hernia repair: a comprehensive review. Hernia 23(2):235–243
Gossetti F, D’Amore L, Annesi E et al (2019) Mesh-related visceral complications following inguinal hernia repair: an emerging topic. Hernia. https://doi.org/10.1007/s10029-019-01905-z
Khan FA, Hashmi A, Edelman DA (2016) Small bowel obstruction caused by self-anchoring suture used for peritoneal closure following robotic inguinal hernia repair. J Surg Case Reports. https://doi.org/10.1093/jscr/rjw117
Degheili JA, Aboul Hosn M, El Lakis M, Hallal AH (2015) Sigmoid to scrotal fistula secondary to mesh erosion: a rare complication of inguinal hernia repair in a patient on anticoagulation. BMC Surg. https://doi.org/10.1186/s12893-015-0070-9
Zuvela M, Krivokapic Z, Galun D, Markovic V (2012) Rare late mesh complications following inguinal prolene hernia system hernioplasty: report of three cases. Surg Today. https://doi.org/10.1007/s00595-012-0189-6
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Köckerling F, Bittner R, Jacob DA et al (2015) TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc. https://doi.org/10.1007/s00464-015-4150-9
van der Linden W, Warg A, Nordin P (2011) National register study of operating time and outcome in hernia repair. Arch Surg 146:1198–1203. https://doi.org/10.1001/archsurg.2011.268
Agrawal A, Avill R (2006) Mesh migration following repair of inguinal hernia: a case report and review of literature. Hernia 10(1):79–82
Fitzgerald HL, Orenstein SB, Novitsky YW (2010) Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutaneous Tech. https://doi.org/10.1097/SLE.0b013e3181dfbc05
Azurin DJ, Schuricht AL, Stoldt HS et al (1995) Small Bowel obstruction following endoscopic extraperitoneal-preperitoneal herniorrhaphy. J Laparoendosc Surg. https://doi.org/10.1089/lps.1995.5.263
Yilmaz I, Karakaş DO, Sucullu I et al (2013) A rare cause of mechanical bowel obstruction: mesh migration. Hernia. https://doi.org/10.1007/s10029-011-0867-0
Yamamoto S, Kubota T, Abe T (2015) A rare case of mechanical bowel obstruction caused by mesh plug migration. Hernia. https://doi.org/10.1007/s10029-014-1247-3
Murphy JW, Misra DC, Silverglide B (2006) Sigmoid colonic fistula secondary to perfix-plug, left inguinal hernia repair. Hernia. https://doi.org/10.1007/s10029-006-0113-3
Benedetti M, Albertario S, Niebel T et al (2005) Intestinal perforation as a long-term complication of plug and mesh inguinal hernioplasty: case report. Hernia. https://doi.org/10.1007/s10029-004-0256-z
Nowak DD, Chin AC, Singer MA, Helton WS (2005) Large scrotal hernia: a complicated case of mesh migration, ascites, and bowel strangulation. Hernia. https://doi.org/10.1007/s10029-004-0260-3
D’Amore L, Gossetti F, Manto O, Negro P (2012) Mesh plug repair: can we reduce the risk of plug erosion into the sigmoid colon? Hernia 16(4):495
Zubaidi A, Al Saghier M, Kabbani M, Abdo A (2006) Colocutaneous fistula after mesh plug inguinal hernia repair—a delayed complication. Ann Saudi Med. https://doi.org/10.5144/0256-4947.2006.385
Barreto SG, Schoemaker D, Siddins M, Wattchow D (2009) Colovesical fistula following an open preperitoneal "Kugel" mesh repair of an inguinal hernia. Hernia. https://doi.org/10.1007/s10029-009-0496-z
Tamam M, Yavuz HS, Hacımahmutoğlu Ş et al (2009) Direct radionuclide cystography imaging in colovesical fistula due to inguinal hernia operation complication. Ann Nucl Med. https://doi.org/10.1007/s12149-009-0276-y
El Hakam MZ, Sharara AI, Chedid V (2010) Persistent Left Lower Abdominal Pain. Gastroenterology 138(1):e5–e6
Karls KA, Lillemoe KD, DeWitt JM (2011) Mesh erosion after inguinal hernia repair: a rare cause of acute lower GI bleeding (with video). Gastrointest Endosc. https://doi.org/10.1016/j.gie.2010.08.057
Isaia M, Christou D, Kallis P et al (2016) Colocutaneous Fistula after open inguinal hernia repair. Case Rep Surg. https://doi.org/10.1155/2016/2019212
Hollinsky C, Göbl S (1999) Bursting strength evaluation after different types of mesh fixation in laparoscopic herniorrhaphy. Surg Endosc 13:958–961. https://doi.org/10.1007/s004649901146
Techapongsatorn S, Tansawet A, Kasetsermwiriya W et al (2019) Mesh fixation technique in totally extraperitoneal inguinal hernia repair—a network meta-analysis. The Surgeon 17:215–224. https://doi.org/10.1016/j.surge.2018.09.002
Sajid MS, Ladwa N, Kalra L et al (2012) A meta-analysis examining the use of tacker fixation versus no-fixation of mesh in laparoscopic inguinal hernia repair. Int J Surg 10:224–231. https://doi.org/10.1016/j.ijsu.2012.03.001
Teng YJ, Pan SM, Liu YL et al (2011) A meta-analysis of randomized controlled trials of fixation versus nonfixation of mesh in laparoscopic total extraperitoneal inguinal hernia repair. Surg Endosc 25:2849–2858. https://doi.org/10.1007/s00464-011-1668-3
Gutlic N, Rogmark P, Nordin P et al (2016) Impact of mesh fixation on chronic pain in total extraperitoneal inguinal hernia repair (tep): a nationwide register-based study. Ann Surg 263:1199–1206. https://doi.org/10.1097/SLA.0000000000001306
Simons MP, Smietanski M, Bonjer HJ et al (2018) International guidelines for groin hernia management. Hernia. https://doi.org/10.1007/s10029-017-1668-x
Gupta A, Mazari F, Samuel N, Balchandra S (2017) Mesh fixation techniques for laparoscopic inguinal hernia repair in adults. Cochrane Database Syst Rev 2017:CD008954. https://doi.org/10.1002/14651858.CD008954.pub2
Novik B, Nordin P, Skullman S et al (2011) More recurrences after hernia mesh fixation with short-term absorbable sutures: a registry study of 82 015 Lichtenstein repairs. Arch Surg 146:12–17. https://doi.org/10.1001/archsurg.2010.302
de Goede B, Klitsie PJ, van Kempen BJH et al (2013) Meta-analysis of glue versus sutured mesh fixation for Lichtenstein inguinal hernia repair. Br J Surg 100:735–742. https://doi.org/10.1002/bjs.9072
Andresen K, Fenger AQ, Burcharth J et al (2017) Mesh fixation methods and chronic pain after transabdominal preperitoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacks. Surg Endosc 31:4077–4084. https://doi.org/10.1007/s00464-017-5454-8
Kaul A, Hutfless S, Le H et al (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26:1269–1278. https://doi.org/10.1007/s00464-011-2025-2
Withers L, Rogers A (2006) A spiral tack as a lead point for volvulus. JSLS J Soc Laparoendosc Surg 10:247–249
Köhler G, Mayer F, Lechner M, Bittner R (2015) Small bowel obstruction after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report and review of the literature. Hernia 19(3):389–394
Tonolini M (2016) Multidetector CT of expected findings and complications after contemporary inguinal hernia repair surgery. Diagn Interv Radiol 22:422–429. https://doi.org/10.5152/dir.2016.15578
Tonolini M, Ippolito S (2016) Multidetector CT of expected findings and early postoperative complications after current techniques for ventral hernia repair. Insights Imaging 7:541–551. https://doi.org/10.1007/s13244-016-0501-x
Liu S, Zhou XX, Li L et al (2018) Mesh migration into the sigmoid colon after inguinal hernia repair presenting as a colonic polyp: a case report and review of literature. World J Clin Cases. https://doi.org/10.12998/WJCC.V6.I12.564
Han HJ, Kim CY, Choi SB et al (2010) Sigmoid colon fistula following totally extraperitoneal hernioplasty: an improper treatment for mesh infection or iatrogenic injury? Hernia. https://doi.org/10.1007/s10029-010-0700-1
Weyhe D, Tabriz N, Sahlmann B, Uslar V-N (2017) Risk factors for perioperative complications in inguinal hernia repair—a systematic review. Innov Surg Sci 2:47–52. https://doi.org/10.1515/iss-2017-0008
Lebeau R, Traoré M, Anzoua KI et al (2016) Prognostic Factors of postoperative morbidity and mortality of adult strangulated groin hernia. Indian J Surg 78:192–196. https://doi.org/10.1007/s12262-015-1343-3
Shah HN, Badlani GH (2012) Mesh complications in female pelvic floor reconstructive surgery and their management: a systematic review. Indian J Urol 28:129–153. https://doi.org/10.4103/0970-1591.98453
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
All the authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Financial disclosure statement
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Koliakos, N., Papaconstantinou, D., Nastos, C. et al. Intestinal erosions following inguinal hernia repair: a systematic review. Hernia 25, 1137–1145 (2021). https://doi.org/10.1007/s10029-020-02324-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02324-1