Abstract
Background
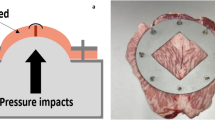
Excessive fascial tension is a major cause of ventral hernia recurrence. Although hernias are commonly characterized by area, the tension experienced by fascia is directly proportional to the surrounding tissue stiffness. We demonstrate an accurate and simple technique for intra-operative measurement of fascial closing tension and quantify the decrease in tension following Component Separation (CS).
Methods
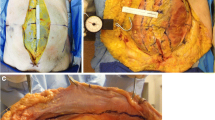
A tensiometer was created using a spring with a known recoil constant (k) and a surgical clamp. Using Hooke’s law (Force = kX; X = spring displacement), fascial tension was calculated. This method was first validated on a bench-top model and then applied to the anterior fascia of 4 fresh cadavers (8 hemi-abdomens) over a range of simulated hernia defect sizes. When fascia could no longer reach midline, CS was performed and measures repeated. Tissue stiffness was calculated by plotting defect size versus resulting tension.
Results
Fascial defects ranged from 1- to 18-cm wide with average midline closing tension prior to release 36.1 N (range 17–48) and 8.2 N (range 5–11) after CS, a mean 76% decrease (range 70%–85%). Mean R2 values between defect size and tension for the synthetic and cadaver models were 0.99 (p < 0.01) and 0.91 (p = 0.01; all hemi-abdomen measurements significant). Inter-rater Pearson’s correlation consistently found R2 values > 0.95 (p < 0.01) for each hemi-abdomen, showing high precision and reproducibility.
Conclusion
We have applied a cheap, simple, and precise method to sterilely assess fascial tension during herniorrhaphy and also quantified the decrease in tension following component separation. This technique may be rapidly translated into the operating room with minimal equipment to provide objective data critical for intraoperative decision-making.







Similar content being viewed by others
References
Burger JWA, Lange JF, Halm JA et al (2005) Incisional hernia: early complication of abdominal surgery. World J Surg 29:1608–1613. https://doi.org/10.1007/s00268-005-7929-3
Gray SH, Vick CC, Graham LA et al (2008) Variation in mesh placement for ventral hernia repair: an opportunity for process improvement? Am J Surg 196:201–206. https://doi.org/10.1016/j.amjsurg.2007.09.041
Höer J, Lawong G, Klinge U, Schumpelick V (2002) Einflussfaktoren der narbenhernienentstehung retrospektive untersuchung an 2.983 laparotomierten patienten über einen zeitraum von 10 jahren. Chirurg 73:474–480. https://doi.org/10.1007/s00104-002-0425-5
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. BJS (Br J Surg) 72:70–71. https://doi.org/10.1002/bjs.1800720127
Luijendijk RW, Hop WC, van den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. New Engl J Med Boston 343:392–398
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237:129–135. https://doi.org/10.1097/00000658-200301000-00018
Breuing K, Butler CE, Ferzoco S et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558. https://doi.org/10.1016/j.surg.2010.01.008
Muysoms FE, Miserez M, Berrevoet F et al (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414. https://doi.org/10.1007/s10029-009-0518-x
Afifi AM, Hartmann E, Talaat A et al (2017) Quantitative assessment of tension reduction at the midline closure during abdominal component separation. J Am Coll Surg 224:954–961. https://doi.org/10.1016/j.jamcollsurg.2016.12.052
Dragu A, Klein P, Unglaub F et al (2009) Tensiometry as a decision tool for abdominal wall reconstruction with component separation. World J Surg 33:1174–1180. https://doi.org/10.1007/s00268-009-9991-8
Klein P, Schmidt O, Reingruber B, Hohenberger W (1998) Reconstruction of incisional hernias with defined tensiometrically controlled tension–a possibility for anatomically correct reconstruction of the abdominal wall. Langenbecks Arch Chir Suppl Kongressbd 115:1027–1030
Klein P, Konzen G, Schmidt O, Hohenberger W (1996) Reconstruction of scar hernias–intraoperative tensiometry for objective determination of procedure of choice. Chirurg 67:1020–1027. https://doi.org/10.1007/s001040050098
Ramirez OMMD, Ruas EMD, Dellon ALMD (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86:519–526
Reingruber B, Kastl S, Stremmel C, Klein PD (2001) Incisional hernia repair: tensiometry for the selection of the appropriate procedure. Eur J Surg 167:903–908. https://doi.org/10.1080/110241501753361587
Hooke R (1678) Lectures de potentia restitutiva, or of spring explaining the power of springing bodies. John Martyn
Botsford T (1941) The tensile strength of sutured skin wound during healing. Surg Gynecol Obst 72:690
Capek L, Jacquet E, Dzan L, Simunek A (2012) The analysis of forces needed for the suturing of elliptical skin wounds. Med Biol Eng Comput 50:193–198. https://doi.org/10.1007/s11517-011-0857-5
Howes EL, Sooy JW, Harvey SC (1929) The healing of wounds as determined by their tensile strength. JAMA 92:42–45. https://doi.org/10.1001/jama.1929.02700270046011
Högström H, Haglund U, Zederfeldt B (1990) Tension leads to increased neutrophil accumulation and decreased laparotomy wound strength. Surgery 107:215–219
Horeman T, Meijer E-J, Harlaar JJ et al (2013) Force sensing in surgical sutures. PLoS ONE 8:e84466. https://doi.org/10.1371/journal.pone.0084466
Hwang K, Kim HJ, Kim KY et al (2015) Skin tension related to tension reduction sutures. J Craniofac Surg 26:e48–50. https://doi.org/10.1097/SCS.0000000000001311
Klink CD, Binnebösel M, Alizai HP et al (2011) Tension of knotted surgical sutures shows tissue specific rapid loss in a rodent model. BMC Surg 11:36. https://doi.org/10.1186/1471-2482-11-36
Paul SP, Matulich J, Charlton N (2016) A new skin tensiometer device: computational analyses to understand biodynamic excisional skin tension lines. Sci Rep 6:1–5. https://doi.org/10.1038/srep30117
Roca J, Nogués M, Villalobos R et al (2018) Surgical dynamometer to simultaneously measure the tension forces and the distance between wound edges during the closure of a laparotomy. Sens (Basel). https://doi.org/10.3390/s18010189
Schachtrupp A, Wetter O, Höer J (2016) An implantable sensor device measuring suture tension dynamics: results of developmental and experimental work. Hernia 20:601–606. https://doi.org/10.1007/s10029-015-1433-y
Acknowledgements
Presented in part at the American College of Surgeons Annual Meeting 2018 (Boston, MA), and the American Society of Plastic Surgeons (ASPS) Annual Meeting 2018 (Chicago, IL).
Funding
This article was funded by Plastic Surgery Foundation Pilot (PSF) Pilot Research Grant #512973. The PSF had no role in the study design, implementation or interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors have no relevant financial interests or relationships to disclose.
Ethics approval
This study was performed in accordance with the ethical standards and institutional review board approval was obtained (IRB #512973).
Human and animal rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Levy, A.S., Bernstein, J.L., Celie, KB. et al. Quantifying fascial tension in ventral hernia repair and component separation. Hernia 25, 107–114 (2021). https://doi.org/10.1007/s10029-020-02268-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02268-6