Abstract
Purpose
Persistent pain is a known side effect after TEP inguinal repair disabling 2–5 % of patients. A standardized diagnostic work-up so far is not available. MRI is a diagnostic tool in the work-up of inguinal hernias. In the present study the yield of MRI in evaluating chronic pain after TEP hernia repair is addressed.
Methods
In our database patients receiving an MRI scan for groin pain lasting more than 3 months after TEP inguinal hernia repair were identified. A checklist with potential pathologic findings was filled out for each groin by two blinded observers. Findings in painful, pain-free and unoperated groins were compared and statistical analysis done based upon their relative incidences. Cohen’s kappa coefficients were calculated to determine interobserver agreement.
Results
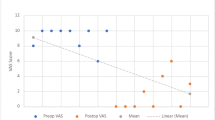
Imaging studies of 53 patients revealed information regarding 106 groins. Fifty-five groins were painful after the initial operation, 12 were pain-free postoperatively and 39 groins were not operated. None of the predefined disorders was observed statistically more often in the patients with painful groins. Only fibrosis appeared more prevalent in patients with chronic pain (P = 0.11). Interobserver agreement was excellent for identifying the mesh (κ = 0.88) and observing bulging or a hernia (κ = 0.74) and was substantial for detecting fibrosis (κ = 0.63). In 40 % of the patients, MRI showed a correct mesh position and observed nothing else than minor fibrosis. A wait and see policy resolved complaints in the majority of the patients. In 15 % of the patients, MRI revealed treatable findings explanatory for persisting groin pain.
Conclusion
For patients with post-TEP hernia groin pain, MRI is useful to confirm a correct flat mesh position and to identify possible not operation-related causes of groin pain. It is of little help to identify a specific cause of groin repair-related pain.



Similar content being viewed by others
References
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88(1):1122–1126
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19(1):48–54
Aasvang E, Kehlet H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaest 95(1):69–76
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194(3):394–400
Linderoth G, Kehlet H, Aasvang EK, Werner MU (2011) Neurophysiological characterization of persistent pain after laparoscopic inguinal hernia repair. Hernia 15:521–529
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, Di Miceli D, Doglietto GB (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15(3):239–249
Aasvang EK, Brandsborg B, Christenen B, Jensen TS, Kehlet H (2008) Neurophysiological characterisation of postherniotomy pain. Pain 137(1):173–181
Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, Bittner R, Kehlet H (2010) Predictive risk factors for persistent post-herniotomy pain. Anesthesiology 112:957–969
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13(4):343–403
Van den Berg JC, de Valois J, Rosenbusch G (1999) Detection of groin hernia with physical examination, ultrasound and MRI compared with laparoscopic findings. Invest Radiol 34:739–743
Van den Berg JC, Go PM, de Valois J, Rosenbusch G (2000) Preoperative and postoperative assessment of laparoscopic inguinal hernia repair by dynamic MRI. Invest Radiol 35:695–698
Leander P, Ekberg O, Sjoberg S, Kesek P (2000) MR imaging following herniography in patients with unclear groin pain. Eur Radiol 10:1691–1696
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139:1297–1298
Barile A, Erriquez D, Cacchio A, De Paulis F, Di Cesare E, Masciocchi C (2000) Groin pain in athletes: role of magnetic resonance. Radiol Med 100:216–222
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Aasvang EK, Jensen K, Fiirgaard B, Kehlet H (2009) MRI and pathology in persistent postherniotomy pain. Am Coll Surg 208(6):1023–1028
Koehler RH (2002) Diagnosing the occult contralateral inguinal hernia. Surg Endosc 16(3):512–520
Crawford DL, Hiatt JR, Philips EH (1998) Laparoscopy identifies unexpected groin hernias. Am Surg 64(10):976–978
Bochkarev V, Ringley C, Vitamvas M, Oleynikov D (2007) Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc 21(5):734–736
Dulucq JL, Wintringer P, Mahajna A (2009) Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3100 hernia repairs over 15 years. Surg Endosc 23(3):482–486
Salati U, Mansour E, Torreggiani W (2013) True-FISP MRI in diagnosis of postoperative hernia recurrence: a brief report. Hernia [Epub ahead of print]
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367(9522):1618–1625
Lau H (2007) Recurrence following endoscopic extraperitoneal inguinal hernioplasty. Hernia 11:415–418
Lilly MC, Arregui ME (2002) Lipomas of the cord and round ligament. Ann Surg 235(4):586–590
Lau H, Patil NG, Yuen WK, Lee F (2003) Prevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc 17:1620–1623
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, Fortelny R, Heikkinen T, Jorgensen LN, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Simons MP (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18:151–163
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the above mentioned authors, certify that they have no commercial associations (e.g., consultancies, stock ownership, equity interests, patent-licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. Partial funding in support of the manuscript was provided in the form of a Research Grant from Johnson & Johnson.
Rights and permissions
About this article
Cite this article
Burgmans, J.P.J., Voorbrood, C.E.H., Van Dalen, T. et al. Chronic pain after TEP inguinal hernia repair, does MRI reveal a cause?. Hernia 20, 55–62 (2016). https://doi.org/10.1007/s10029-015-1448-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-015-1448-4