Abstract
Introduction
Chronic pain is a frequent and notable complication after inguinal hernia repair, it has been extensively studied, but its management and diagnosis are still difficult. The cause of chronic pain following inguinal hernia surgery is usually multifactorial. This case series highlights the utility of MRI neurography (MRN) in evaluating the damage to inguinal nerves after a hernia repair, with surgical confirmation of the preoperative imaging findings.
Materials and Methods
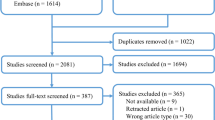
A retrospective review was performed on patients who underwent inguinal mesh removal and triple denervation of the groin. Inclusion criteria included MRI neurography. All patients underwent surgical exploration of the inguinal canal for partial or complete mesh removal and triple denervation of the groin by the same senior surgeon.
Results
A total of nine patients who underwent triple denervation were included in this case series. MRN was then performed on 100% of patients. The postoperative mean VAS score adjusted for all patients was 1.6 (SD p), resulting in a 7.5 score difference compared to the preoperative VAS score (p). Since chronic groin pain can be a severely debilitating condition, diagnosis, and treatment become imperative.
Conclusion
MRN can detect direct and indirect signs of neuropathy even in the absence of a detectable compressive cause aids in management and diagnosis by finding the precise site of injury, and grading nerve injury to aid pre-operative assessment for the nerve surgeon. Thus, it is a valuable diagnostic tool to help with the diagnosis of nerve injuries in the setting of post-inguinal hernia groin pain.




Similar content being viewed by others
Data Availability
Data is available upon request.
References
Andresen K, Rosenberg J (2018) Management of chronic pain after hernia repair. J Pain Res 11:675–681. https://doi.org/10.2147/JPR.S127820
Marcus DA (2005) Chronic pain: a primary care guide to practical management, vol 1. Humana Press, Inc, Totowa, NJ, pp 333–318
Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Kosek E, Lavand'homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH et al (2015) A classification of chronic pain for ICD-11. Pain 156(6):1003–1007. https://doi.org/10.1097/j.pain.0000000000000160
Alfieri S, Amid PK, Campanelli G et al (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249. https://doi.org/10.1007/s10029-011-0798-9
Morrison Z, Kashyap S, Nirujogi VL ( 2022) Adult inguinal hernia. StatPearls Publishing, Treasure Island (FL). https://www.ncbi.nlm.nih.gov/books/NBK537241/?report=classic
Nikkolo C, Lepner U (2016) Chronic pain after open inguinal hernia repair. Postgrad Med 128(1):69–75. https://doi.org/10.1080/00325481.2016.1121090
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92(7):795–801. https://doi.org/10.1002/bjs.5103
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Poobalan AS, Bruce J, King PM, Chambers WA, Krukowski ZH, Smith WC (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88(8):1122–1126. https://doi.org/10.1046/j.0007-1323.2001.01828.x
Song JW, Wolf JS Jr, McGillicuddy JE, Bhangoo S, Yang LJ (2011) Laparoscopic triple neurectomy for intractable groin pain: technical report of 3 cases. Neurosurgery. 68(2 Suppl Operative):339–346. https://doi.org/10.1227/NEU.0b013e3182114480
Amid PK (2002) A 1-stage surgical treatment for postherniorrhaphy neuropathic pain: triple neurectomy and proximal end implantation without mobilization of the cord. Arch Surg 137(1):100–104. https://doi.org/10.1001/archsurg.137.1.100
Lee P, Dorsi M, Belzberg A, Chhabra A (2011) Magnetic resonance neurography-surgical correlation of neurologic thoracic outlet syndrome. Microsurgery. 31(8):662–665. https://doi.org/10.1002/micr.20935
Hakeem A, Shanmugam V (2011) Current trends in the diagnosis and management of post-herniorraphy chronic groin pain. World J Gastrointest Surg 3(6):73–81. https://doi.org/10.4240/wjgs.v3.i6.73
Madura JA, Madura JA 2nd, Copper CM, Worth RM (2005) Inguinal neurectomy for inguinal nerve entrapment: an experience with 100 patients. Am J Surg 189(3):283–287. https://doi.org/10.1016/j.amjsurg.2004.11.015
Amid PK (2004) Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia 8:343–349. https://doi.org/10.1007/s10029-004-0247-0
Amid PK (2004) Radiologic images of meshoma: a new phenomenon causing chronic pain after prosthetic repair of abdominal wall hernias. Arch Surg 139(12):1297–1298. https://doi.org/10.1001/archsurg.139.12.1297
Seddon HJ (1943) Three types of nerve injury. Brain 66(4):237–288. https://doi.org/10.1093/brain/66.4.237
Robinson L (2000) Traumatic injury to peripheral nerves. American Association of Electrodiagnostic Medicine, Seattle, pp 1–3 https://www.aanem.org/mxonline/resources/downloads/Monograph/28_Traumatic%20Injury%20to%20Peripheral%20Nerves.pdf. Accessed July 31, 2022
Drake RL, Vogl W, Mitchell AWM (2005) Gray’s anatomy for students. Churchhill Livingstone (Elsevier Inc.), Philadelphia, PA, pp 253–254
Ariyasinghe C, Gajera J. Iliohypogastric nerve. Reference article, Radiopaedia.org. https://doi.org/10.53347/rID-38666. Accessed 30 Jul 2022
Delaney H, Bencardino J, Rosenberg ZS (2014) Magnetic resonance neurography of the pelvis and lumbosacral plexus. Neuroimaging Clin N Am 24(1):127–150. https://doi.org/10.1016/j.nic.2013.03.026
Gupton M, Varacallo M. Anatomy, abdomen and pelvis, genitofemoral nerve. StatPearls Publishing, Treasure Island (FL). https://www.ncbi.nlm.nih.gov/books/NBK430733/
Dessouky R, Xi Y, Scott KM et al (2018) Magnetic resonance neurography in chronic lumbosacral and pelvic pain: diagnostic and management impact-institutional audit. World Neurosurg 114:e77–e113. https://doi.org/10.1016/j.wneu.2018.02.072
Aggarwal A, Chhabra A (2022) Magnetic resonance neurography: is it so complicated that it needs a touch of genius? Eur Radiol 32:3912–3914. https://doi.org/10.1007/s00330-021-08525-1
Chhabra A, Belzberg A, Rosson G et al (2015) Impact of high resolution 3 Tesla MR neurography (MRN) on diagnostic thinking and therapeutic patient management. Eur Radiol 26(5):1235–1244. https://doi.org/10.1007/s00330-015-3958-y
Tagliafico A, Succio G, Serafini G, Martinoli C (2012) Diagnostic accuracy of MRI in adults with suspect brachial plexus lesions: a multicentre retrospective study with surgical findings and clinical follow-up as reference standard. Eur J Radiol 81(10):2666–2672. https://doi.org/10.1016/j.ejrad.2011.10.007
Chhabra A, Thawait GK, Soldatos T, Thakkar RS, Del Grande F, Chalian M, Carrino JA (2013) High-resolution 3T MR neurography of the brachial plexus and its branches, with emphasis on 3D imaging. AJNR Am J Neuroradiol 34(3):486–497. https://doi.org/10.3174/ajnr.A3287
Author information
Authors and Affiliations
Contributions
A. De la Fuente Hagopian: data curation, formal analysis, visualization, methodology, writing—original draft, writing—review, and editing, study conception, and design. S. Guadarrama-Sistos Vazquez: data curation, investigation, visualization, writing—original draft, writing—review editing, study conception, and design. S. Farhat: data curation, writing—review, and editing. N. Reddy: data curation, writing–review, and editing. M.A. Trakhtenbroit: conceptualization, resources, data curation, supervision, project administration, writing—review, and editing. A. Echo: conceptualization, resources, data curation, supervision, project administration, writing—review, and critical revision of manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors did not receive any funding for this study. They have no financial disclosures and report no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De la Fuente Hagopian, A., Guadarrama-Sistos Vazquez, S., Farhat, S. et al. The emerging role of MRI neurography in the diagnosis of chronic inguinal pain. Langenbecks Arch Surg 408, 319 (2023). https://doi.org/10.1007/s00423-023-03050-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03050-9