Abstract
Purpose
The purpose of this study is to evaluate the histologic response to fibrin sealant (FS) as an alternative fixation method for laparoscopic ventral hernia repair.
Methods
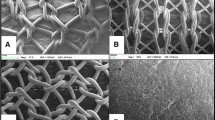
One non-absorbable barrier mesh (Composix™) and three absorbable barrier meshes (Sepramesh™, Proceed™, and Parietex™ Composite) were used for the study, with uncoated macroporous polypropylene mesh (ProLite Ultra™) as the control. Three methods of fixation were used: #0-polypropylene suture + FS (ARTISS™, Baxter Healthcare Corp.), FS alone (ARTISS™), or tacks alone (n = 10 for each group). Two pieces of mesh (of dimensions 4 × 4-cm) were secured intraperitoneally in 75 New Zealand white rabbits. After 8 weeks, hematoxylin and eosin (H&E)-stained specimens were evaluated for host tissue response. Statistical significance (P < 0.05) was determined using a one-way analysis of variance (ANOVA) with Fisher’s least significant difference (LSD) post hoc test.
Results
Composix™ with FS only showed significantly greater cellular infiltration than with suture + FS (P = 0.0007), Proceed™ with FS only had significantly greater neovascularization than with suture + FS (P = 0.0172), and ProLite Ultra™ with suture + FS had significantly greater neovascularization than with tacks only (P = 0.046). Differences due to mesh type showed that Composix™ exhibited less extensive cellular infiltration (P ≤ 0.0032), extracellular matrix (ECM) deposition, and neovascularization, and demonstrated less inflammatory cells and more fibroblasts compared to the other meshes (P < 0.05).
Conclusions
FS did not have a significant histologic effect compared to tacks when utilized for the fixation of mesh to the peritoneum of New Zealand White rabbits. However, the mesh type did have a significant histologic effect. The permanent barrier mesh (Composix™) was associated with less histologic incorporation than absorbable barrier and macroporous meshes, as evidenced by lower levels of cellular infiltration, ECM deposition, and neovascularization, independent of the fixation method used.



Similar content being viewed by others
References
Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW (1992) Laparoscopic cholecystectomy. The new ‘gold standard’? Arch Surg 127(8):917–923
Smith CD, Weber CJ, Amerson JR (1999) Laparoscopic adrenalectomy: new gold standard. World J Surg 23(4):389–396
Katkhouda N, Mavor E (2000) Laparoscopic splenectomy. Surg Clin North Am 80(4):1285–1297
Heniford BT, Ramshaw BJ (2000) Laparoscopic ventral hernia repair: a report of 100 consecutive cases. Surg Endosc 14(5):419–423
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21(3):378–386
Carbonell AM, Harold KL, Mahmutovic AJ, Hassan R, Matthews BD, Kercher KW, Sing RF, Heniford BT (2003) Local injection for the treatment of suture site pain after laparoscopic ventral hernia repair. Am Surg 69(8):688–691
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238(3):391–399
Karakousis CP, Volpe C, Tanski J, Colby ED, Winston J, Driscoll DL (1995) Use of a mesh for musculoaponeurotic defects of the abdominal wall in cancer surgery and the risk of bowel fistulas. J Am Coll Surg 181(1):11–16
Katkhouda N, Mavor E, Friedlander MH, Mason RJ, Kiyabu M, Grant SW, Achanta K, Kirkman EL, Narayanan K, Essani R (2001) Use of fibrin sealant for prosthetic mesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg 233(1):18–25
Joels CS, Matthews BD, Kercher KW, Austin C, Norton HJ, Williams TC, Heniford BT (2005) Evaluation of adhesion formation, mesh fixation strength, and hydroxyproline content after intraabdominal placement of polytetrafluoroethylene mesh secured using titanium spiral tacks, nitinol anchors, and polypropylene suture or polyglactin 910 suture. Surg Endosc 19(6):780–785
Ceccarelli G, Casciola L, Pisanelli MC, Bartoli A, Di Zitti L, Spaziani A, Biancafarina A, Stefanoni M, Patriti A (2008) Comparing fibrin sealant with staples for mesh fixation in laparoscopic transabdominal hernia repair: a case control-study. Surg Endosc 22(3):668–673
Hickerson WL, Nur I, Meidler R (2011) A comparison of the mechanical, kinetic, and biochemical properties of fibrin clots formed with two different fibrin sealants. Blood Coagul Fibrinolysis 22(1):19–23
Goldenberg MM (2008) Pharmaceutical approval update. Pharm Ther 33(5):299–302
Jenkins ED, Melman L, Frisella MM, Deeken CR, Matthews BD (2010) Evaluation of acute fixation strength of absorbable and nonabsorbable barrier coated mesh secured with fibrin sealant. Hernia 14(5):505–509
Jenkins ED, Melman L, Desai S, Brown SR, Frisella MM, Deeken CR, Matthews BD (2011) Evaluation of intraperitoneal placement of absorbable and nonabsorbable barrier coated mesh secured with fibrin sealant in a New Zealand white rabbit model. Surg Endosc 25(2):604–612
Valentin JE, Badylak JS, McCabe GP, Badylak SF (2006) Extracellular matrix bioscaffolds for orthopaedic applications. A comparative histologic study. J Bone Joint Surg Am 88(12):2673–2686
Acknowledgments
This study was supported by a research grant from Baxter Healthcare Corp., Deerfield, IL, USA.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below are the links to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jenkins, E.D., Melman, L., Desai, S. et al. Histologic evaluation of absorbable and non-absorbable barrier coated mesh secured to the peritoneum with fibrin sealant in a New Zealand white rabbit model. Hernia 15, 677–684 (2011). https://doi.org/10.1007/s10029-011-0834-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-011-0834-9