Abstract
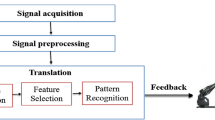
Pain monitoring is crucial to provide proper healthcare for patients during general anesthesia (GA). In this study, photoplethysmographic waveform amplitude (PPGA), heartbeat interval (HBI), and surgical pleth index (SPI) are utilized for predicting pain scores during GA based on expert medical doctors’ assessments (EMDAs). Time series features are fed into different long short-term memory (LSTM) models, with different hyperparameters. The models’ performance is evaluated using mean absolute error (MAE), standard deviation (SD), and correlation (Corr). Three different models are used, the first model resulted in 6.9271 ± 1.913, 9.4635 ± 2.456, and 0.5955 0.069 for an overall MAE, SD, and Corr, respectively. The second model resulted in 3.418 ± 0.715, 3.847 ± 0.557, and 0.634 ± 0.068 for an overall MAE, SD, and Corr, respectively. In contrast, the third model resulted in 3.4009 ± 0.648, 3.909 ± 0.548, and 0.6197 ± 0.0625 for an overall MAE, SD, and Corr, respectively. The second model is selected as the best model based on its performance and applied 5-fold cross-validation for verification. Statistical results are quite similar: 4.722 ± 0.742, 3.922 ± 0.672, and 0.597 ± 0.053 for MAE, SD, and Corr, respectively. In conclusion, the SPI effectively predicted pain score based on EMDA, not only on good evaluation performance, but the trend of EMDA is replicated, which can be interpreted as a relation between SPI and EMDA; however, further improvements on data consistency are also needed to validate the results and obtain better performance. Furthermore, the usage of further signal features could be considered along with SPI.












Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due state restrictions such as privacy and ethical restrictions.
References
Dodds C (1999) General anaesthesia. Drugs 58(3):453–467. https://doi.org/10.2165/00003495-199958030-00006
Gruenewald M et al (2009) Influence of different remifentanil concentrations on the performance of the surgical stress index to detect a standardized painful stimulus during sevoflurane anaesthesia. Br J Anaesth 103(4):586–593. https://doi.org/10.1093/bja/aep206
Huiku M et al (2007) Assessment of surgical stress during general anaesthesia. Br J Anaesth 98(4):447–455. https://doi.org/10.1093/bja/aem004
Wennervirta J, Hynyneh M, Koivusalo A-M, Uutela K, Huiku M, Vakkuri A (2008) Surgical stress index as a measure of nociception/antinociception balance during general anesthesia. Acta Anaesthesiol Scand 52(8):1038–1045. https://doi.org/10.1111/j.1399-6576.2008.01687.x
Chen X et al (2010) Comparison of surgical stress index-guided analgesia with standard clinical practice during routine general anesthesia. Anesthesiology 112(5):1175–1183. https://doi.org/10.1097/aln.0b013e3181d3d641
Struys MMRF, Vanpeteghem C, Huiku M, Uutela K, Blyaert NBK, Mortier EP (2007) Changes in a surgical stress index in response to standardized pain stimuli during propofol–remifentanil infusion. Br J Anaesth 99(3):359–367. https://doi.org/10.1093/bja/aem173
Ahonen J, Jokela R, Uutela K, Huiku M (2007) Surgical stress index reflects surgical stress in gynaecological laparoscopic day-case surgery. Br J Anaesth 98(4):456–461. https://doi.org/10.1093/bja/aem035
Won YJ, Lim BG, Kim YS, Lee M, Kim H (2018) Usefulness of surgical pleth index-guided analgesia during general anesthesia: a systematic review and meta-analysis of randomized controlled trials. J Int Med Res 46(11):4386–4398. https://doi.org/10.1177/0300060518796749
M. Roy Chowdhury, R. Madanu, M. F. Abbod, S.-Z. Fan, and J.-S. Shieh, “Deep learning via ECG and PPG signals for prediction of depth of anesthesia,” Biomedical Signal Processing and Control, vol. 68, p. 102663, Jul. 2021, https://doi.org/10.1016/j.bspc.2021.102663.
Jean W-H, Sutikno P, Fan S-Z, Abbod MF, Shieh J-S (2022) Comparison of deep learning algorithms in predicting expert assessments of pain scores during surgical operations using analgesia nociception index. Sensors 22(15):5496. https://doi.org/10.3390/s22155496
Jeanne M, Logier R, De Jonckheere J, Tavernier B, “Validation of a graphic measurement of heart rate variability to assess analgesia/nociception balance during general anesthesia,” Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual International Conference, vol. 2009, pp. 1840–1843, 2009, https://doi.org/10.1109/IEMBS.2009.5332598.
Logier R, Jeanne M, Tavernier B (2004) Method and device for assessing pain in human being, University Hospital of Lille, vol. University of Lille II.
Liu Q et al (2019) Spectrum analysis of EEG signals using CNN to model patient’s consciousness level based on anesthesiologists’ experience. IEEE Access 7(99):53731–53742. https://doi.org/10.1109/access.2019.2912273
Liu Q, Ma L, Chiu R-C, Fan S-Z, Abbod MF, Shieh J-S (2017) HRV-derived data similarity and distribution index based on ensemble neural network for measuring depth of anaesthesia. PeerJ, 5: e4067 https://doi.org/10.7717/peerj.4067.
Jiang GJA et al (2015) Sample entropy analysis of EEG signals via artificial neural networks to model patients’ consciousness level based on anesthesiologists experience. Biomed Res Int 2015:1–8. https://doi.org/10.1155/2015/343478
Bonhomme V et al (2011) Comparison of the surgical pleth index TM with haemodynamic variables to assess nociception–anti-nociception balance during general anaesthesia. Br J Anaesth 106(1):101–111. https://doi.org/10.1093/bja/aeq291
Cicchetti DV (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 6(4):284–290. https://doi.org/10.1037/1040-3590.6.4.284
Liang Y, Elgendi M, Chen Z, Ward R (2018) An optimal filter for short photoplethysmogram signals. Sci Data 5(1): https://doi.org/10.1038/sdata.2018.76
Huiku M et al. (2005) Assessment of surgical stress using heart rate and plethysmographic pulse wave amplitude variability. cris.vtt.fi.
Ledowski T, Schneider M, Gruenewald M, Goya RK, Teo SR, Hruby J (2019) Surgical pleth index: prospective validation of the score to predict moderate-to-severe postoperative pain. Br J Anaesth 123(2):e328–e332
Liu J, Tang W, Chen G, Lu Y, Feng C, Tu XM (2016) Correlation and agreement: overview and clarification of competing concepts and measures. Shanghai Arch Psychiatry, 28(2): 115–120. Doi: https://doi.org/10.11919/j.issn.1002-0829.216045.
Acknowledgements
This research is supported by Ministry of Science and Technology (Grant number: MOST 110-2221-E-155 -004—MY2).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was presented in part at the joint symposium of the 28th International Symposium on Artificial Life and Robotics, the 8th International Symposium on BioComplexity, and the 6th International Symposium on Swarm Behavior and Bio-Inspired Robotics (Beppu, Oita, and Online, January 25–27, 2023).
About this article
Cite this article
Abdel Deen, O.M.T., Jean, WH., Fan, SZ. et al. Pain scores estimation using surgical pleth index and long short-term memory neural networks. Artif Life Robotics 28, 600–608 (2023). https://doi.org/10.1007/s10015-023-00880-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10015-023-00880-0