Abstract
This paper addresses the development of a dementia screening tool using a character-input-type brain–computer Interface (BCI). A blinking letter board is presented to the subject for each matrix by the character-input-type BCI, and by keeping an eye on one character, the character-gazing is estimated based on the event-related potential P300 of the subject. In this experiment, the subject is instructed to specify and subsequently watch a task character. Four sets are made, each consisting of five or six task letters per subject. The subjects include 53 elderly people in their 60 s and 90 s who were diagnosed with specific symptoms of dementia. The dementia types of the subjects include the Alzheimer’s type of dementia (AD), the Lewy body type of dementia, as well as the mild cognitive impairment (MCI). The relationship between the types of dementia and the four BCI features is explained by the Kruskal–Wallis test and multiple comparisons. Also, dementia types are classified using the BCI features that are closely related to each specific type. The results were obtained using four BCI features as inputs to the classifier and three dementia types as outputs. The classification rate for the three groups was about 60%. Since the classification rate of dementia with the Lewy body (DLB) is low, the classification was performed in two groups, MCI and AD. Furthermore, the classification rate of about 80% was confirmed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In Japan, the number of patients with dementia is increasing, and by 2025, 1 in 5 persons over the age of 65 years is expected to have dementia [1]. The progress of the Alzheimer’s type of dementia (AD) can be suppressed by medication. Therefore, the early detection of dementia is important [2].
However, the average time from noticing the first changes that contribute to the development of dementia to conducting diagnosis is 7.4 ± 6.9 months. Additionally, it takes 2.9 ± 11.0 months on average from the first examination to the final diagnosis [3]. Therefore, the period from suspected dementia to a medical diagnosis tends to be rather long in Japan. The reasons vary from “I do not want to go to the hospital” (38.7%) to “I think the change is due to aging” (33.6%) [4]. Furthermore, the shortage of medical personnel specialized in dementia is a major problem, and the Ministry of Health, Labor, and Welfare is promoting measures to improve and encourage family doctors to respond to dementia as well as the training of dementia support doctors who are consultants of these family doctors [1]. As a solution, even a tool supporting the diagnosis by healthcare workers can be considered.
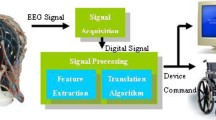
In this study, we developed a tool for the portable screening of easy cognitive functions using a character-input-type. Brain–computer interface (BCI). The character-input-type BCI can be implemented in ~ 20–30 min. Previous studies explained the relationship between neuropsychological tests and BCI measurement items, such as the spelling-error distance value (SEDV) [5]. The association among the SEDV, a unique index, as well as the score of the Mini-Mental State Examination (MMSE), a neuropsychological test, was confirmed (Fig. 1) [5], 5]. In Fig. 1, the original index SEDV is used on the vertical axis and the cognitive decline level related to the score of the neuropsychological test MMSE is used on the horizontal axis. The relative distance considering the characteristics of the character-input-type BCI is shown by the original index SEDV. Details will be explained in Chapter 3. The level of cognitive decline is divided into levels based on the score of the neuropsychological test MMSE [5]. However, these studies were only focused on the relationship between the BCI measurement items and the neuropsychological test scores and the relationship with actual physician diagnosis was not considered. A neuropsychological test is one of the elements that are used for the diagnosis, and the diagnosis of an actual physician is associated with a higher-order index.
There are several types of dementia. In this study, on the focus was placed on the AD, the dementia with the Lewy body (DLB), and the mild cognitive impairment (MCI) that is closely related to dementia. The largest number of patients with cognitive impairment, such as forgetfulness and memory impairment, as well as behavioral and psychological symptoms, such as indifference and depression, is believed to be related to the AD. The DLB has been recently discovered, and its prevalence is gradually increasing. The related symptoms include temporal changes in the cognitive function, hallucinations, and concurrent Parkinson’s disease. MCI is not dementia, however, symptoms that are similar to AD, such as cognitive decline, appear. These symptoms are milder in comparison with dementia, however, 10%–15% of MCI patients are expected to progress to dementia annually [7].
The classification of dementia is important because symptoms, speed of progression, and therapies vary depending on the type of dementia. In this study, we investigated whether BCI cognitive screening is possible by classifying the relationship between a physician’s diagnosis and the BCI measurement items. Using these results, we further investigated whether dementia can be classified using BCI measurement items.
2 Outline of the experiment
2.1 Character-input-type BCI
The character-input-type BCI is a communication aid device that uses event-related potential (ERP) P300 and is applied as a measurement device for attention concentration. Collaborators do not need to have a mental model of the BCI as they are only asked to gaze and utter specific characters present on the letter board. P300 is a positive brain action potential that occurs ~ 300 ms after the presentation of a stimulus when attention is paid to an infrequent stimulus for two or more stimuli [8].
2.2 Contents of experiment
During the experiment, a 6-row × 10-column letter board is presented to each subject. Subjects are given a specific character and asked to gaze at it. Figure 2 shows the landscape of the experiment and Fig. 3 shows the used letter board. While the subject is gazing at the character, the rows or columns of the letter board blink randomly one by to act as a stimulus. The P300 component of the subject is average in each row and column, and the character at the intersection of the row and column where the P300 component is detected the most is estimated to be the character that the subject is gazing at. Characters that are prompted by the subject are defined as task characters, while characters estimated by the BCI are defined as estimated characters. After the instructions were given to the subjects, five or six characters were showed as an input alternately for 1 or 2 min, and a total of 4 inputs were made.
The first was treated as learning data for the linear discriminant analysis (LDA), while the remaining three inputs were used as the target data for the analysis.
2.3 Subject information
The subjects were dementia patients who were somewhere in between their sixties to their nineties and visited the Tokyo Medical University outpatient department. The study began in 2016, and 53 patients who had no data deficits in their measurement and who suffered from AD (n = 23), DLB (n = 12), and MCI (n = 18) were included. The average age was 80.1 ± 0.57 years. A neuropsychological examination and the character-input-type BCI measurement were performed on the same day. The subjects were diagnosed by specialists as AD, DLB, or MCI based on neuropsychological and brain imaging.
The study was conducted with the approval of the Tokyo Medical University ethics review board (early diagnosis of dementia using BCI 2016-083). All the subjects provided written informed consent.
3 Measurement items
Usually, an abbreviation needs to be spelled out once in the Abstract, again in the main text, and used consistently thereafter.
Four BCI parameters were measured, including the SEDV (character), the P300 latency (ms), the P300 linear discrimination rate (%), and the correct answer rate (%). The SEDV is the relative distance between the task character and the estimated character that is created considering the characteristics of the character-input-type BCI. The higher the SEDV is, the lower the input accuracy to the computer and the attention concentration become. The SEDV can be calculated using Eq. (1) when the estimated character is shifted by character A horizontally from the task character and by character B vertically. The match of the character estimated by the BCI with one rows/columns of the task character is indicated by D1, whereas the difference between both the characters estimated by the BCI and the task character row/column is indicated by D2. In BCI character estimation, correct characters can be input only after the matching of the task character and the row/column of the BCI estimated character. However, the fact that there is a match between one of the rows and columns describes the character estimation of the BCI as half correct. Therefore, the processing was performed in this study with half the weight.
P300 latency is the time from the presentation of the stimulus until the appearance of the P300 vertex. The stimulus is presented at 0 ms, and the time when the P300 vertex is confirmed is treated as the latency (ms).
The correct answer rate for each trial of the test subject is represented by the P300 linear discriminant rate, while the ratio of the matching of the task characters to the estimated characters is described by the correct answer rate.
The correct answer rate is a rate at which the assignment character and the estimated character match.
4 Dementia types and measurement items
The nonparametric Kruskal–Wallis test was performed on the AD, DLB, and MCI groups. Multiple comparisons were made after the conduction of the Kruskal–Wallis test to verify the significance of the measurement items.
4.1 SEDV and dementia type
The Kruskal–Wallis test was performed to determine the relationship between the SEDV and the AD, DLB, and MCI groups. The main effect was confirmed as p < 0.001. Multiple comparisons were performed to verify the differences between the groups. A significant difference was identified between the MCI and the DLB groups (p < 0.01), the MCI and the AD groups (p < 0.001), as well as the DLB and the AD groups (p < 0.05). Figure 4 shows the relationship between the SEDV and the various types of dementia. The results indicate that the SEDV is effective in the classification of dementia into AD, DLB, and MCI.
4.2 P300 latency and dementia types
The Kruskal–Wallis test was performed to examine the relationship between the three groups of dementia types (MCI, AD, DLB) and the P300 latency. Consequently, p < 0.10 indicated a significant tendency. Figure 5 shows the relationship between the P300 latency and the dementia types. It is suggested that the P300 latency is effective in the classification of the DLB and the AD.
4.3 P300 linear discrimination rate and dementia types
A Kruskal–Wallis test was performed to examine the relationship between the three groups with different types of dementia (MCI, AD, DLB) as well as the linear discrimination rate of P300. As a result, p < 0.10 indicated a significant tendency. Multiple comparisons were subsequently performed to verify the differences between the groups. As a result, a significant trend of p < 0.10 was confirmed between the MCI group and the AD group. Figure 6 shows the relationship between the P300 linear discrimination rate and the various types of dementia. It is suggested that the P300 linear discrimination rate is effective in the classification of the MCI group and the DLB:AD group.
4.4 Correct answer rate and dementia types
The Kruskal–Wallis test was performed to examine the relationship between the three groups with different types of dementia (MCI, AD, DLB) and the correct answer rate. As a result, p < 0.001 and the main effect were confirmed. The multiple comparisons were subsequently performed to verify the differences between the groups. The results showed a significant difference of p < 0.005 between the MCI and the DLB groups, and a significant difference of p < 0.0005 was observed between the MCI and the DLB groups. Figure 7 shows that the correct answer rate is effective for the classification of the MCI group and the DLB:AD group. Figure 7 shows the relationship between the correct answer rate and the type of dementia.
5 Classification of dementia types
5.1 Classification of dementia by machine learning
In this study, the possibility of the classification of dementia using the BCI measurement items associated with the different types of dementia was investigated. The MATLAB2019 classification learning machine was used for the classification. The subjects were classified according to the dementia type; the inputs were the SEDV, the P300 latency, the P300 linear discrimination rate, and the average of each correct answer rate; as well as the outputs were the AD, the DLB, and the MCI. The used classification methods included the LDA, the support vector machine (SVM), and the k-nearest neighbor (knn) (n = 5) method. In the analysis, cross-validation was used and the test was divided into five parts.
5.2 Classification results
The accuracy for each classification method and the F value for each class are shown in Table 1. Accuracy indicates the accuracy of the entire classifier, and the classification accuracy of each class is indicated by the F value. Both values range from 0 to 1, and the closer the value is to 1, the higher the evaluation of the classification model becomes. As the accuracy did not reach 70%, the classification accuracy should be considered far from good. Additionally, the classification of the DLB was found to be difficult because the F value of the DLB was low in case of all classification methods. The DLB differs from te AD in that early movements, such as falls and the appearance of the Parkinson's disease, are can be identified from the early stage. Therefore, it is difficult to be classified by the BCI.
5.3 Classification of the two groups
In the previous section, the output of the classifier was obtained as three groups, but the classification of the MCI and the AD without the DLB was also examined. Many people think that the MCI means the precursor state of the AD, therefore, the classification of the MCI and the AD interval has great significance. Table 2 shows the accuracy and the F value for the MCI and the AD groups. The accuracy and the F value exceeded 0.8 for both the LDA and the SVM, indicating that both the MCI and the AD could be classified with a high accuracy. It is suggested that the BCI can be used to classify the MCI and the AD.
5.4 Comparison with existing methods
The classification results based on the MMSE score are shown for comparison with existing methods. The same 53 people were targeted as a subject for this experiment. The classification was performed in three groups and two groups using the score of the neuropsychological test MMSE as the input. The classification method was the same as in Chapter 5.1. Table 3 shows the results of the classification in the three groups, and Table 4 shows the results of the classification in the two groups. Tables 1 and 3 as well as Tables 2 and 4 were the comparison targets. There was no big difference identified during the comparison, suggesting the possibility of classification by BCI.
Also, Qing Li et al. used sMRI (Structural magnetic resonance imaging), FDG-PET (fluorodeoxyglucose positron emission tomography), and florbetapir-PET in a single module as well as in a combined module of the three to classify the MCI and the AD groups [9]. Only a minimal difference was observed during the comparison of the classification accuracy by the BCI and the classification accuracy by the brain imaging test, suggesting that the classification by the BCI may be performed at the same level as the existing method (Table 5).
6 Conclusion
This study investigated the measurement items and the classification of dementia to develop a cognitive screening tool using the BCI. Previous studies have revealed the relationship between the SEDV and various neuropsychological tests, however, the cognitive function type could not be classified. Firstly, we investigated the relationship between the BCI measurement items (the SEDV, the P300 latency, the P300 linear discrimination rate, and the correct answer rate) and the various types of dementia. Secondly, we verified the three-group classification of the AD, the DLB, and the MCI. The accuracy and the F value were used as evaluation indexes of the classification model, and in the three-group classification, a low accuracy was confirmed as a cognitive screening tool. The classification of the DLB was difficult, and a high classification accuracy was confirmed with the two-group classifications of the AD and the MCI, which, in turn, confirmed the possibility of classifying dementia into the AD and the MCI types with the use of the BCI. Besides, there was no significant difference observed between the classification results using the neuropsychological test MMSE and the BCI classification results as well as the classification results using the brain imaging test and the BCI classification results, suggesting the possibility of testing and classification by the BCI.
In this report, the results are shown in regard of a limited number of subjects. Although the 53 subjects that were included in this report are not sufficient for benchmarking, this paper can be considered as a basic study which showed the possibility of classifying dementia types by the BCI.
References
Ministry of Health, Labor and Welfare (2019) https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/kaigo_koureisha/ninchi/index.html. Accessed 12 oct 2020
Wu J, Syuusaku T (2009) Department of Neurology Fusion of science, engineering, and information science. Ohmsha, Tokyo
Black CM, Baishali MA, Pike J et al (2019) The diagnostic pathway from cognitive impairment to dementia in Japan: quantification using real-world data. Alzheimer Dis Assoc Disord 33:346–353
Katayama S (2014) Questionnaire survey on diagnosis and treatment of dementia. Eli Lilly Japan Co Ltd, London, pp 12–17
Kurihara R, Tanaka H, Umahara T et al (2017) BCI character input characteristics in patients with mild dementia. In: Human Interface Symposium, 2017, 6C1-1
Morooka R, Fukushima A et al (2019) Early diagnosis method of dementia using BCI and frontal lobe function test. Hum Interface Symp 22(2):211–218
Japan Society for Dementia Research (2008) Dementia textbook. Chugai-Igakusha, Tokyo
Irino H (2005) Event-related potential guides for psychology Cook. Kitaohjishobo, Tokyo
Li Q, Wu X et al (2017) Classification of alzheimer's disease, mild cognitive impairment, and cognitively unimpaired individuals using multi-feature kernel discriminant dictionary learning. Front Comput Neurosci 1:117
Acknowledgements
This work was supported by JSPS KAKENHI Grant Number JP19K12880 and the Subsidy for research expenses related to the development of minimally invasive treatments ・diagnosis devices, a joint research project between the Tokyo Medical University and the Kogakuin University. I would like to express my deep appreciation to all those who participated in the experiment. I would like to express my sincere appreciation to the Tokyo Medical University in the field of geriatrics for their cooperation and opinions regarding the experiment.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Fukushima, A., Morooka, R., Tanaka, H. et al. Classification of dementia type using the brain-computer interface. Artif Life Robotics 26, 216–221 (2021). https://doi.org/10.1007/s10015-020-00673-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10015-020-00673-9