Abstract
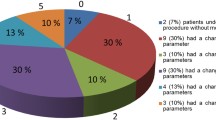
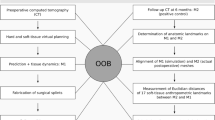
The 3D prediction of post-operative changes is an inevitable tool for the surgical correction of facial asymmetry. The objective is to execute an evidence-based review answering the following question. Does the 3D virtual prediction planning draw reliable and accurate results in the surgical outcome related to the soft tissues of the face in facial asymmetry? This systematic review of the literature is based on the 3D soft tissue prediction planning of facial asymmetry correction to draw conclusions on the reliability and accuracy of these methods in the surgical outcome related to the soft tissues of the face. PubMed, Web of Science, Cochrane, and Ovid databases were adopted for the literature search. Studies published between years 2000 and 2020, aimed at the assessment of soft tissue predictions using software prediction packages for facial asymmetry, were selected. The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) was applied. Quadas-2 tool was used for the qualitative evaluation of selected studies. Initial search yielded 248 articles. Twenty articles fulfilled the inclusion and exclusion criteria and selected for qualitative analysis. Finally, 12 articles were selected for quantitative analysis. The results indicate 3D imaging prediction methods provided more accurate information with less distortion for soft tissue prediction regardless of various softwares currently available. The prediction of soft tissue accuracy in facial asymmetry was less accurate in lower face regardless of the type of surgery for facial asymmetry. The mean prediction error was less than 2 mm.




Similar content being viewed by others
References
Kim SC, Kwon JG, Jeong WS, Lee JY, Kwon SM, Choi JW (2018) Three-dimensional photogrammetric analysis of facial soft-to-hard tissue ratios after bimaxillary surgery in facial asymmetry patients with and without sturge-weber syndrome. Ann Plast Surg 81(2):178–185
Proffit W, Turvey T, Phillip C (2007) The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med 3:21
Severt TR, Proffit WR (1997) Post-surgical stability following correction of facial asymmetry. Int J Adult Orthod Orthogn Surg 12:251–262
Swennen GR, Mollemans W, De Clercq C, Abeloos J, Lamoral P, Lippens F et al (2009) A cone-beam computed tomography triple scan procedure to obtain a three-dimensional augmented virtual skull model appropriate for orthognathic surgery planning. J Craniofac Surg 20:297–307
Sun Y, Luebbers HT, Agbaje JO, Schepers S, Vrielinck L, Lambrichts I et al (2013) Accuracy of upper jaw positioning with intermediate splint fabrication after virtual planning in bimaxillary orthognathic surgery. J Craniofac Surg 24:1871–1876
Zinser MJ, Mischkowski RA, Dreiseidler T, Thamm OC, Rothamel D, Zoller JE (2013) Computer-assisted orthognathic surgery: waferless maxillary positioning, versatility, and accuracy of an image-guided visualisation display. Br J Oral Maxillofac Surg 51:827–833
Ho CT, Lin HH, Liou EJ, Lo LJ (2017) Three-dimensional surgical simulation improves the planning for correction of facial prognathism and asymmetry: a qualitative and quantitative study. Sci Rep 7:40423
Wu TY, Lin HH, Lo LJ, Ho CT (2017) Postoperative outcomes of two- and three-dimensional planning in orthognathic surgery: a comparative study. J Plast Reconstr Aesthet Surg 70:1101–1111
Farrell BB, Franco PB, Tucker MR (2014) Virtual surgical planning in orthognathic surgery. Oral Maxillofac Surg Clin North Am 26:459–473
Polley JW, Figueroa AA (2013) Orthognathic positioning system: intraoperative system to transfer virtual surgical plan to operating field during orthognathic surgery. J Oral Maxillofac Surg 71:911–920
Li B, Zhang L, Sun H, Yuan J, Shen SG, Wang X (2013) A novel method of computer aided orthognathic surgery using individual CAD/CAM templates: a combination of osteotomy and repositioning guides. Br J Oral Maxillofac Surg 51:e239–e244
Eckardt C Cunningham S (2004) How predictable is orthognathic surgery? Eur. J. Orthod, 26, 303–309. [CrossRef] [PubMed]
Olivetti EC, Nicotera S, Marcolin F, Vezzetti E, Sotong JPA, Zavattero E, Ramieri G (2019) 3D soft-tissue prediction methodologies for orthognathic surgery—a literature review. Appl Sci 9(21):4550
Demétrio MS, Marlière DAA, Barbosa SM et al (2021) Different modalities to record and transfer natural head position to virtual planning in Orthognathic surgery: Case reports of Asymmetric patients. J. Maxillofac Oral Surg 20:443–454. https://doi.org/10.1007/s12663-020-01376-1
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011 Oct 18;155(8):529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009. PMID: 22007046.
Elshebiny T, Morcos S, Mohammad A, Quereshy F, Valiathan M (2019) Accuracy of three-dimensional soft tissue prediction in orthognathic cases using dolphin three-dimensional software. [Evaluation Study]. J Craniofac Surg 30(2):525–528
Lo LJ, Yamaguchi K, Niu LS, Liao CH, Lin HH (2020) Fat grafting in patients with extensive unilateral facial deficiency: three-dimensional computer-assisted planning, implementation and outcome assessment. Ann Plast Surg 84(1S Suppl 1):S94–S99
Jayaratne YS, Lo J, Zwahlen RA, Cheung LK (2010) Three-dimensional photogrammetry for surgical planning of tissue expansion in hemifacial microsomia [Case Reports]. Head Neck 32(12):1728–1735
Arias E, Huang YH, Zhao L, Seelaus R, Patel P, Cohen M (2019) Virtual surgical planning and three-dimensional printed guide for soft tissue correction in facial asymmetry. J Craniofac Surg 30(3):846–850
Mundluru T, Almukhtar A, Ju X, Ayoub A (2017) The accuracy of three-dimensional prediction of soft tissue changes following the surgical correction of facial asymmetry: An innovative concept. Int J Oral Maxillofac Surg 46(11):1517–1524
Christou T, Kau CH, Waite PD, Kheir NA, Mouritsen D (2013) Modified method of analysis for surgical correction of facial asymmetry. Annals of maxillofacial surgery 3(2):185–191. https://doi.org/10.4103/2231-0746.119218
Tiwari R, Chakravarthi PS, Kattimani VS, Lingamaneni KP (2018) A perioral soft tissue evaluation after orthognathic surgery using three-dimensional computed tomography scan. Open Dentistry Journal 12:366–376. https://doi.org/10.2174/1874210601812010366
Hajeer MY, Ayoub AF, Millett DT (2004) Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br J Oral Maxillofac Surg 42(5):396–404
Suzuki-Okamura E, Higashihori N, Kawamoto T, Moriyama K (2015) Three-dimensional analysis of hard and soft tissue changes in patients with facial asymmetry undergoing 2-jaw surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 120(3):299–306
Jung YJ, Kim MJ, Baek SH (2009) Hard and soft tissue changes after correction of mandibular prognathism and facial asymmetry by mandibular setback surgery: three-dimensional analysis using computerized tomography [Comparative Study]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107(6):763–771
Choi JW, Lee JY, Oh TS, Kwon SM, Yang SJ, Koh KS (2014) Frontal soft tissue analysis using a 3 dimensional camera following two-jaw rotational orthognathic surgery in skeletal class III patients. J Craniomaxillofac Surg 42(3):220–226
Igelbrink S, Zanettini LMS, Bohner L, Kleinheinz J, Jung S (2020) Three-dimensional planning of the mandibular margin in hemifacial microsomia using a printed patient-specific implant. J Craniofac Surg 31(8):2297–2301
Alkhayer A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020 Dec 4;16(1):34. https://doi.org/10.1186/s13005-020-00250-2. PMID: 33272289; PMCID: PMC7716456
Chabanas M, Marrecaux C, Chouly F, Boutault F, Payan Y (2004) Evaluating soft tissue simulation in maxillofacial surgery using preoperative and postoperative CT scans. In Proc of CARS 2004:419e424
Liebregts JHF, Timmermans M, De Koning MJJ, Bergé SJ, Maal TJJ (2015) Three-dimensional facial simulation in bilateral sagittal split osteotomy: a validation study of 100 patients. J Oral Maxillofac Surg 73(5):961–970. https://doi.org/10.1016/j.joms.2014.11.006
Kaipatur NR, Flores-Mir C (2009) Accuracy of computer programs in predicting orthognathic surgery soft tissue response. J Oral Maxillofac Surg 67(4):751–759. https://doi.org/10.1016/j.joms.2008.11.006
Wermker K, Kleinheinz J, Jung S, Dirksen D. Soft tissue response and facial symmetry after orthognathic surgery. J Craniomaxillofac Surg. 2014 Sep;42(6):e339-45 https://doi.org/10.1016/j.jcms.2014.01.032. Epub 2014 Jan 15. PMID: 24529350
Joss CU, Joss-Vassalli IM, Kiliaridis S, Kuijpers-Jagtman AM (2010) Soft tissue profile changes after bilateral sagittal split osteotomy for mandibular advancement: a systematic review. J Oral Maxillofac Surg 68(6):1260–9
Hsu SS, Gateno J, Bell RB, Hirsch DL, Markiewicz MR, Teichgraeber JF et al (2013) Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. [Multicenter Study Research Support N I H ,Extramural Research Support Non-U S Gov’t]. J Oral Maxillofac Surg 71(1):128–142
Cavalcanti M, Rocha S, Vannier M (2004) Craniofacial measurements based on 3D-CT volume rendering: implications for clinical applications. Dentomaxillofacial Radiol 33(3):170–176. https://doi.org/10.1259/dmfr/13603271
Lee D-Y, Bailey LJ, Proffit WR (1996) Soft tissue changes after superior repositioning of the maxilla with Le Fort I osteotomy: 5-year follow-up. Int J Adult Orthodon Orthognath Surg 11(4):301–311
Ullah R, Turner PJ, Khambay BS (2015) Accuracy of three-dimensional soft tissue predictions in orthognathic surgery after Le Fort I ad-vancement osteotomies. Br J Oral Maxillo-fac Surg 53(153–7):1
Alkhayer A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020 Dec 4;16(1):34 https://doi.org/10.1186/s13005-020-00250-2. PMID: 33272289; PMCID: PMC7716456
van Hemelen G, van Genechten M, Renier L, Desmedt M, Verbruggen E, Nadjmi N (2015) Three-dimensional virtual planning in orthognathic surgery enhances the accuracy of soft tissue prediction. [Comparative Study Randomized Controlled Trial]. J Craniomaxillofac Surg 43(6):918–925
Xia JJ, Shevchenko L, Gateno J, Teichgraeber JF, Taylor TD, Lasky RE, McGrory KR (2011) Outcome study of computer-aided surgical simulation in the treatment of patients with craniomaxillofacial deformities. J Oral Maxillofac Surg 69(7):2014–2024. https://doi.org/10.1016/j.joms.2011.02.018
Hertanto M, Ayoub AF, Benington PCM, Naudi K, and McKenzie P. (2021). Orthognathic patient perception of 3D facial soft tissue prediction planning.Journal of Cranio-Maxillofacial Surgeryhttps://doi.org/10.1016/j.jcms.2021.03.009
Acknowledgements
The authors are grateful to the Deanship of Scientific Research of King Saud University for the funding received through the Vice Deanship of Scientific research chairs no RG-1439-062. The authors would like to thank the faculty and staff of the department of maxillofacial surgery and CDRC (College of Dentistry Research Centre) of their respective institutions for their support and guidance in this study. We would like to express our gratitude and respect to Professor Dr A Ayoub, Head of Maxillofacial surgery, College of Dentistry, University of Glasgow for the guidance and support in this study.
Funding
The authors are grateful to the Deanship of Scientific Research, King Saud University for the funding received through the Vice-Deanship of Scientific Research Chairsno RG-1439–062.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This review is registered and approved by the International Prospective Register of Systematic Reviews (PROSPERO), CRD 42020219671.
Consent to participate
All participants have given their consent to participate in the study.
Consent for publication
All authors have given consent to publish the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Philip, M.R., AlFotawi, R. The accuracy of soft tissue movement using virtual planning for non-syndromic facial asymmetry cases—a systematic review. Oral Maxillofac Surg 27, 187–200 (2023). https://doi.org/10.1007/s10006-022-01059-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10006-022-01059-w