Abstract
Objective
To systematically review the literature for mid-sagittal plane establishment approaches to identify the most effective method for constructing the mid-sagittal plane for the evaluation of facial asymmetry.
Materials and methods
Six electronic databases (PubMed, Medline (via Ovid), EMBASE (via Ovid), Cochrane Library, Web of Science, and Scopus) and grey literature were searched for the studies that computed the mid-sagittal reference plane three-dimensionally, using a combination of MeSH terms and keywords. The methodological quality and the level of evidence for the included studies were analyzed using QUADAS-2 and GRADE, respectively.
Results
The preliminary search yielded 6746 records, of which 42 articles that met the predefined inclusion criteria were included in the final analysis. All the included articles reported the construction of the mid-sagittal reference plane (MSP) using varied methods. The risk of bias and concerns regarding the applicability of the included studies were judged to be ‘low’. The level of evidence was determined to be ‘low’ for the effectiveness of the technique and ‘moderate’ for the ease of clinical applicability.
Conclusion
Despite methodological heterogeneity, this review substantiates the comparable efficacy of cephalometric and morphometric MSP construction methods. A fully automated morphometric MSP holds promise as a viable option for routine clinical use. Nevertheless, future prospective studies with an emphasis on the impact, accuracy, and clinical applicability of MSP construction techniques in cases of facial asymmetry are required.
Clinical relevance
The present review will assist clinicians in selecting the most suitable method for MSP construction, leading to improved treatment planning and ultimately more favorable treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Facial asymmetry has a markedly detrimental psychosocial, aesthetic, and functional effect on an individual’s quality of life [1]. Consequently, patients with true skeletal facial asymmetry often seek surgical correction [2]. This is commonly achieved by complex three-dimensional (3D) surgical movements aimed at restoring their facial symmetry in line with their peers. The key to an aesthetic symmetrical outcome relies on determining the site and severity of the facial disharmony, which in turn is determined by the accuracy of the estimated sagittal plane.
Two-dimensional (2D) postero-anterior cephalography and full-face photographs [3, 4] have historically been used to evaluate facial asymmetry. However, the information provided is limited because they cannot accurately depict the true three-dimensional nature of the facial skeleton [5, 6]. The advent of 3D imaging and its routine use in various fields, such as orthodontics and oral and maxillofacial surgery, has revolutionized the process of diagnosing, planning, and predicting the outcomes of surgery [7,8,9,10]. Regardless of the imaging modality, determining the mid-sagittal plane (MSP) is fundamental to the process [4, 11,12,13]. Several approaches for establishing a plane of symmetry have been used, depending on the image type being analysed. These have included simple landmarks for 2D cephalograms and form, shape, or landmark configuration for 3D images. In addition, an array of nomenclature has been documented for the plane of symmetry [1, 3, 14, 15]. These include ‘Best Symmetry Plane [16], Symmetry Plane, or Primal Sagittal Plane [17]. However, there is no agreement as to which method defines a clinically valid MSP in patients presenting with facial disharmony [15], and to date, no paper has systematically reviewed all the published methods that are currently available. Therefore, the aim of this paper was to systematically review the literature for different approaches utilized to establish the mid-sagittal plane in order to choose the most effective method for constructing the mid-sagittal plane for the evaluation of facial asymmetry.
Materials and methods
Protocol & registration
The systematic review reported follows the PRISMA guidelines: Preferred Reporting Items for Systematic Reviews and Meta-Analyses [18]. The review protocol was registered with the PROSPERO database (registration number: CRD42020218963; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020218963).
Eligibility criteria
The following focused topic that matched the Population-Intervention-Control-Outcome (PICO) criteria was the subject of a literature search: “What is the best technique to construct a mid-sagittal reference plane for the estimation of facial asymmetry?” For this review, studies that addressed the aforementioned question were judged appropriate. The elements for PICO criteria have been listed in Table 1. Studies were considered if they met the following inclusion criteria: 1) utilized a 3D technology-based tool, device, or software or conducted any intervention for the estimation of MSP; 2) conducted on humans and had the proper analytical design, such as case–control studies, cross-sectional studies, prospective studies, and retrospective studies, including pilot studies; 3) study data did not duplicate or overlap with those of other articles; 4) studies had full text availability and were published in English. Studies performed on animals, non-human models, non-pertinent data, not involving facial asymmetry subjects or focused on 2D analysis, letters to editors, conference papers, and review articles were excluded from the current systematic review.
Information sources and literature search
All the relevant studies were identified systematically and independently by two authors (DA and PS) through a comprehensive search in the electronic databases:PubMed, EMBASE (via Ovid), Medline (via Ovid), Cochrane Library, Scopus, and Web of Science (until June 2023) with the combination of Medical Subject Headings (MeSH) terms as keywords. Moreover, vocabulary and syntax were adjusted across the databases. The literature search was not constrained by publication date or status. In addition, manual and OpenGrey database (http://www.opengrey.eu/) searches were carried out.
Study selection
After conducting a comprehensive literature search, two authors (DA and PS) independently conducted an initial evaluation of the titles and abstracts of potential to ensure their eligibility according to the predetermined inclusion and exclusion criteria. Disagreements over the inclusion of the studies at this stage were solved by discussion. Next, the full-text studies that conformed to the inclusion criteria were retrieved. The Cohen’s kappa statistic (κ) was used to determine the inter-reviewer agreement level. Any disagreement in study selection between the two authors was resolved by an independent third author (GM). Collation, management of potentially eligible records, and bibliographic citations obtained from the literature search were conducted using Endnote™, version X9 (Clarivate Analytics, Philadelphia, USA).
Data extraction and outcomes of interest
Data extraction was performed independently by the two reviewers (DA and PS) according to the standardized and predefined data format, recording the following outcomes: 1) effectiveness of the technique; and 2) ease of clinical applicability. Accordingly, the following data were extracted from the full text articles:
-
1)
Demographic data (age, gender, ethnicity, sample size, and skeletal discrepancy).
-
2)
Characteristics of the study (study design, asymmetry criteria, and comparison groups).
-
3)
Features of MSP construction (3D technique, software used, MSP type, nomenclature used, construction technique, and reference points).
-
4)
Features of the analysis (landmark digitization, asymmetry assessment, reliability assessment, and measurement type).
Quality analysis
The methodological quality of each paper for the risk of bias and applicability was assessed using customized assessment criteria based on the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) [19] (Supplementary Appendix 1). Two reviewers (DA and PS) rated each study independently and assigned a score of low, high, or unclear based on the information presented in the study.
Level of evidence
The strength of the evidence for the included articles was determined using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) scale [20]. The level of evidence was categorized as high, moderate, low, or very low. The ratings were downgraded for the studies exhibiting serious or very serious concerns pertaining to publication bias, inconsistency, imprecision, indirectness, or risk of bias.
Results
Study selection
The PRISMA flowchart presented in Fig. 1 shows the study selection process. Initially, 6746 records were identified through a comprehensive search across six databases, and 8 records were identified from additional sources. After excluding 66 duplicates, the titles and abstracts of 6680 articles were screened. Of those, 6640 articles were excluded due to their irrelevance to the topic. Following initial screening, a total of 48 articles (40 from the database search and 8 from additional sources) were sought for full text retrieval; however, only 47 potentially eligible articles were assessed for full text review as the full text for one article was unavailable. Following a detailed review of the full text articles, an additional 5 studies were eliminated, and finally, 42 studies that met the inclusion criteria were considered suitable for qualitative analysis. A list of the excluded full text articles along with their justifications is presented in Supplementary Appendix 2. There was excellent inter-reviewer agreement for the study selection process, with Cohen’s κ values of 0.89.
Study characteristics
The demographic and methodological characteristics of all the included studies are summarized in Tables 2 and 3. Between 2005 and 2023, a total of 42 studies were identified, focusing on estimating the mid-sagittal plane in patients with facial asymmetry. Out of the selected 42 studies, eight were computational studies [1, 3, 21,22,23,24,25,26]; six were observational [14, 15, 27,28,29,30]; 21 studies used retrospective analytical design [4, 9, 9, 12, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]; three were experimental studies [17, 48, 49], and one study was ambispective in nature [50]. The age range of the patients in all the included studies was 7–57 years. Further, the included studies revealed diverse asymmetry criteria, such as a deviation of 1 mm to 4 mm in soft tissue chin position based on menton (Me), pogonion (Pog), or Gonion (Gn) [4, 12, 15, 24, 28, 30, 32, 9, 33,34,35, 38,39,40,41,42,43,44,45, 47,48,49,50,51,52,53].
Study quality assessment
The results for the methodological quality and risk of bias assessment have been presented in Fig. 2. All the included studies were representative of the target population; nevertheless, owing to the retrospective, observational, experimental, or computational nature of the included studies, concerns regarding the risk of bias were rated to be relatively ‘high’ in the subject/model selection domain. Within the index test domain, seven studies failed to explicitly define facial asymmetry [3, 16, 17, 22, 31, 9, 46] and four studies inadequately described the process for MSP construction [16, 21, 9, 33]. As a result, these studies were considered to have a ‘high’ risk of bias. However, the overall risk of bias in the index test domain was assessed as ‘low’. Concerning the risk of bias in the reference standard domain, most of the studies were considered to have a ‘low’ risk. With regard to the risk of bias in the domain of workflow, the validity and reliability of MSP construction were questionable in 13 of the included studies [9, 16, 17, 21,22,23,24,25,26, 32, 41, 46, 52], and therefore considered to have an ‘unclear/high’ risk of concern. In addition, 19 of the included studies [4, 15,16,17, 22,23,24,25, 28, 29, 31, 9, 33, 39, 43, 44, 49, 50] either did not report the specific skeletal discrepancy or focused solely on a particular type, such as Class III malocclusion, juvenile idiopathic arthritis, or craniofacial dysplasia. As a result, the MSP construction methodology described in those 19 studies may not be applicable to all types of facial asymmetry conditions and therefore, they were rated as having a ‘high’ risk of bias. In general, concerns regarding the risk of bias in the domain of workflow were relatively ‘low’.
Concerns about applicability were deemed to be ‘unclear’ in the subject/model selection domain since 19 of the included studies [4, 14, 15, 22, 23, 9, 24, 25, 28, 32,33,34, 36,37,38,39, 41, 46, 49, 52] lacked a detailed description of the sampling unit, including the type of skeletal discrepancy, asymmetry criteria, or the patient’s age and gender. The reproducibility of the constructed MSP was found to be questionable in 13 of the included studies [16, 17, 21,22,23,24,25,26, 32, 9, 41, 46, 52] as they failed to report the reliability assessment, which led to a rating of ‘high’ risk of concern; however, the overall risk was judged to be ‘low’ in the index test domain. Regarding the reference standard domain, nine studies with ambiguous reference standards were considered to have ‘unclear’ risk [17, 26, 31, 38, 39, 41, 49, 50, 52], while the majority of the studies were deemed to have ‘low’ risk. The Supplementary Figure includes a detailed presentation of the study quality and risk of bias assessment.
Table 4 provides the evidence profile for the outcomes examined in this study. The evidence quality was ‘low’ for the effectiveness of the technique and ‘moderate’ for the ease of clinical applicability.
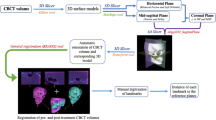
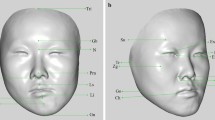
Effectiveness of the technique
The majority of the included studies [12, 14, 27,28,29,30,31, 9, 32, 36, 37, 39,40,41,42,43,44,45,46,47,48,49, 51,52,53] constructed a cephalometric MSP, while eight studies computed a morphometric MSP [3, 17, 21,22,23,24, 34, 38] for the assessment of asymmetry (Table 3). In addition, five studies employed both cephalometric and morphometric MSP construction methods [4, 15, 25, 35, 50], while four studies assessed asymmetry using a symmetry plane [1, 26, 9, 33]. For the cephalometric MSP construction, N-S was the most consistently used landmark combination [12, 28, 35, 39, 40, 43, 47, 48]. Whilst morphometric MSP was determined using modified Procrustes Analysis [35], and Global Registration [34, 38]. The use of the morphometric MSP was found to be accurate and suitable for the evaluation of facial asymmetry in six studies [3, 4, 15, 34, 35, 38]. In particular, based morphometric MSPs showed extremely stable and reliable results (ICC > 0.9) for the estimation of facial asymmetry.
Ease of clinical applicability
A semi-automatic technique that involves digital landmarking was employed for cephalometric and morphometric MSP construction in nine studies [23, 24, 28, 31, 32, 40, 47,48,49], whereas a fully automated and landmark-independent technique for morphometric MSP and symmetry plane construction was reported in seven studies [3, 16, 21, 25, 9, 33, 50]. The fully automated MSP construction method was reported to accurately measure the degree of asymmetry and achieve satisfactory skeletal symmetry, as asserted by the authors in their respective studies (Table 3).
Discussion
Symmetry is a fundamental aspect of a face’s ability to be regarded as socially alluring [54] and in order to achieve optimal function and facial esthetics, orthognathic surgery is performed to correct the underlying maxillomandibular deformity through osteotomies and repositioning of the maxilla-mandibular complex [10, 55, 56]. Management of a three-dimensional compound problem like facial asymmetry requires a realistic and composite approach, which entails modifying the roll, yaw, and pitch of the maxillo-facial structures [28]. Since patients are critical to any changes in their facial appearance following orthognathic surgery, a precise surgical outcome prediction is crucial. Considering the heterogeneity in the aetiology, pathology, and site of facial asymmetry, clinicians are compelled to follow a multifactorial, stepwise decision-making process. The first stage in this process is the establishment of an accurate MSP. Previous studies have substantiated that if MSP does not correspond to the external facial structure (facial morphology) and internal structures (skeletal structures), it provides fallacious information, thus affecting treatment planning [15, 49]. Therefore, the construction of an accurate MSP is essential not only for quantifying the degree of symmetry between the right and left sides of the face but also for arriving at the correct diagnosis.
A comprehensive systemic review of the literature revealed that the construction of the MSP is most commonly based on three techniques: cephalometric MSP, morphometric MSP, and a symmetry plane. Cephalometric MSP is a technique for constructing a mid-sagittal plane (MSP) that relies on anatomical landmarks and involves digitizing these landmarks manually or digitally. The morphometric MSP technique can be undertaken semi-automatically using landmarks or fully automatically without relying on landmarks. The symmetry plane, on the other hand, is a landmark-independent technique for constructing an MSP that can be done semi-automatically or automatically. In the semi-automatic approach, clinicians manually select a seed point in the CT image for segmentation using the "region growing" method. This is followed by extracting the "initial symmetry plane", which is then used with algorithms to calculate the "optimal symmetry plane" [26]. In contrast, the fully automatic technique of the symmetry plane relies solely on algorithms. It involves voxel pairing and mathematical optimization to determine the "optimal symmetry plane", eliminating the need for landmark identification [33]. Where landmark-dependent approaches utilized various paired or unpaired landmark combinations such as Nasion (N), Sella (S), Anterior Nasal Spine (ANS), Basion, and Crista Galli for the MSP construction, landmark-independent methods employed different mathematical algorithms, including the Iterative Closest Point (ICP) algorithm, the LAGER (Landmark Geometric Routine) algorithm, the Oriented Bounding Box (OBB) algorithm, Procrustes Analysis (PA), modified Procrustes Analysis, Weighted Procrustes Analysis (WPA), Principal Component Analysis (PCA), Global Registration method, Clinically derived midline, and Voxel-based method. Despite the fact that a myriad of nomenclatures have been used to represent various MSP construction methods (Table 3), a detailed analysis of the included studies revealed that all the MSPs fell into one of the three MSP construction approaches. Representing MSPs with multiple names in different studies can be misleading not only to the readers but also to the clinicians. Therefore, systematic reporting of various MSP types and nomenclatures becomes indispensable.
Effectiveness of the technique
The cephalometric method has been evidenced to be reliable, highly familiar, and a simple technique, as head orientation has no influence on the landmark placement and is therefore convenient in the clinical setting [4, 28]. The present review demonstrated that cephalometric MSP based on N-ANS-PNS was consistent with the symmetric mid-sagittal reference plane [4]. However, a plane passing through the stable landmarks N-S [12] and perpendicular to the horizontal reference plane would be a more appropriate approach if damage or deviation of the ANS were suspected. Ajmera et.al, in their study, utilized N-S based cephalometric MSP and reported it to be equally effective as a clinically derived midline for facial asymmetry estimation [35]. Despite its several advantages, the cephalometric method may seem challenging due to the inherent limitations associated with its landmark digitization step. For instance, midline structures may tip from the true plane of symmetry; stable landmarks need to be identified that are unaffected by asymmetry; errors associated with manual or digital landmark annotation; and the reproducibility of the identified landmarks [4, 15]. The morphometric technique, on the other hand, was developed to overcome some of the shortcomings of the cephalometric method [15]. The strength of the morphometric method is its capacity to use the external face characteristics, which serve as a framework of perceptiveness for asymmetry, to ascertain the true plane of symmetry [15, 57]. Damstra et al. compared cephalometric and morphometric MSPs and suggested using a morphometric approach based on intact regions of the skull, unaffected by asymmetry, to determine MSP [15]. Likewise, Hsiao et al. reported voxel-based morphometric MSP as a more reliable approach compared to the cephalometric method, due to the latter’s dependence on the operator’s skill in identifying landmarks, whereas the former is less prone to deviation even in cases of severe asymmetry [25]. In contrast, a recent study by Ajmera et al. found cephalometric and morphometric approaches (clinically derived midline and modified Procrustes analysis) to be equally effective [35]. The authors further reported that the modified Procrustes method is a practical alternative to conventional Procrustes analysis for evaluating asymmetry. Conventional Procrustes analysis considers all landmarks to achieve an optimal fit, whereas the modified Procrustes method only utilizes four stable landmarks in the upper facial region (bilateral porions and orbitales) that are minimally influenced by asymmetry to achieve the best fit. This was in agreement with Shin et al.’s findings, who reported analogous results for asymmetry measurements (p > 0.05) using morphometric and cephalometric MSP construction approaches [4]. Zhu et al. in their study, compared three different algorithms for morphometric MSP construction and reported that weighted PA-based MSP was a promising approach for cases of severe mandibular deviation [24]. Assessing the various morphometric approaches previously employed, Global registration [34, 38] and modified PA [35] methods were found to be more robust approaches for asymmetry estimation. This is because the Global registration method utilizes a stable anterior cranial base for registration, preventing the influence of other asymmetric regions of the skull, whereas modified PA utilizes four stable landmarks (bilateral porion and orbitale) that are least affected by asymmetry to achieve the ‘best fit’. Interestingly, PA, which has been used in numerous prior investigations, was found to exhibit a masking effect that reduces asymmetry characteristics and may not accurately reflect the true clinical situation [35].
The reliability of the approach is critical for the clinical effectiveness of the MSP construction technique. In the present review, the reliability of the technique was critically analyzed, which revealed that several studies [1, 9, 17, 21,22,23,24, 32] failed to report the reliability assessment despite concluding with encouraging results. For instance, Wong et al. [16, 9, 33] advocated a novel automated and landmark-independent method of MSP construction referred to as the “Symmetry Plane”. Nevertheless, the effectiveness of their technique can be deemed questionable because the information regarding the software used was only briefly described and a reliability assessment was not performed.
Ease of applicability
For routine clinical use, MSP construction needs to be simple, user-friendly, and ideally fully automatic. Current landmark-dependent methods are simple and user-friendly, but at the same time, they are also technique-sensitive, as they rely on manual or automatic landmarking. While manual digitization is subjective and time-consuming, automatic landmarking may not locate the landmarks precisely and may introduce further errors during asymmetry evaluation. When employing a morphometric approach, the cost of the software and hardware and the need for additional training should not be overlooked [4, 15, 58]. Although the morphometric approach may be quicker to implement, it may not be cost-effective. On the other hand, as the technique is less landmark-dependent and more reliable, it may improve diagnosis and reduce treatment planning time. In this regard, voxel-based morphometric MSP [25] could be a viable option for asymmetry assessment. Another fully automated approach, based on a ‘Symmetry plane’ [9, 16, 33] although showed promising results for routine clinical use, may not be applicable in a routine clinical context owing to the inaccessibility of the in-house developed software.
Limitations and future outlook
Despite a comprehensive search and selection of specific studies, this review was limited due to the methodological heterogeneity observed across the included studies, which precluded performing a meta-analysis. Additionally, a lack of standardized assessment of facial asymmetry was noted, which may have had an impact on the findings. In addition, many of the included studies did not adequately demonstrate the accuracy of the constructed MSP. Future prospective studies with an emphasis on the impact, accuracy, and clinical applicability of MSP construction techniques in cases of facial asymmetry are required.
Conclusion
Achieving favorable treatment outcomes and patient satisfaction in cases of facial asymmetry relies on accurate pre-operative planning. This systematic review highlights the importance of precisely determining the MSP during diagnosis and treatment planning. Despite significant methodological variations across the included studies, the following conclusions can be drawn:
-
1.
Provided that stable landmarks are used, both cephalometric and morphometric methods for MSP construction are equally effective and offer the closest approximation to the true symmetrical MSP.
-
2.
Among the various cephalometric and morphometric methods, a cephalometric MSP constructed using stable landmarks such as N-S and perpendicular to the FH plane provides optimal estimation of facial asymmetry. In terms of morphometric approaches, both global registration and modified PA methods are robust approaches for estimating asymmetry.
-
3.
From a clinical applicability perspective, a fully automated voxel-based morphometric MSP holds promise as a viable option for routine clinical use.
The findings presented in this review will assist clinicians in selecting the most suitable method for MSP construction, leading to improved treatment planning and ultimately more favorable treatment outcomes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tung-Yiu W, Jing-Jing F, Tung-Chin W (2005) A novel method of quantifying facial asymmetry. Int Congr Ser 1281:1223–1226. https://doi.org/10.1016/j.ics.2005.03.174
Nur RB, Cakan DG, Arun T (2016) Evaluation of facial hard and soft tissue asymmetry using cone-beam computed tomography. Am J Orthod Dentofacial Orthop 149:225–237. https://doi.org/10.1016/j.ajodo.2015.07.038
Hartmann J, Meyer-Marcotty P, Benz M, Häusler G, Stellzig-Eisenhauer A (2007) Reliability of a Method for Computing Facial Symmetry Plane and Degree of Asymmetry Based on 3D-data. J Orofac Orthop 68:477–490. https://doi.org/10.1007/s00056-007-0652-y
Shin SM, Kim YM, Kim NR, Choi YS, Park SB, Kim YI (2016) Statistical shape analysis-based determination of optimal midsagittal reference plane for evaluation of facial asymmetry. Am J Orthod Dentofacial Orthop 150:252–260. https://doi.org/10.1016/j.ajodo.2016.01.017
Gateno J, Xia JJ, Teichgraeber JF (2011) Effect of facial asymmetry on 2-dimensional and 3-dimensional cephalometric measurements. J Oral Maxillofac Surg 69:655–662. https://doi.org/10.1016/j.joms.2010.10.046
Eng ZHD, Yick YY, Guo Y, Xu H, Reiner M, Cham TJ, Chen SHA (2017) 3D faces are recognized more accurately and faster than 2D faces, but with similar inversion effects. Vision Res 138:78–85. https://doi.org/10.1016/j.visres.2017.06.004
Schmidt JC, Gutekunst CJ, Dagassan-Berndt D, Schmidlin PR and Walter C (2019) Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters. Dent J (Basel) 7. https://doi.org/10.3390/dj7020050
Hsu PJ, Denadai R, Pai BCJ, Lin HH, Lo LJ (2020) Outcome of facial contour asymmetry after conventional two-dimensional versus computer-assisted three-dimensional planning in cleft orthognathic surgery. Sci Rep 10:2346. https://doi.org/10.1038/s41598-020-58682-4
Kim TY, Baik JS, Park JY, Chae HS, Huh KH, Choi SC (2011) Determination of midsagittal plane for evaluation of facial asymmetry using three-dimensional computed tomography. Imaging Sci Dent 41:79–84. https://doi.org/10.5624/isd.2011.41.2.79
Ajmera DH, Singh P, Leung YY, Gu M (2021) Three-dimensional evaluation of soft-tissue response to osseous movement after orthognathic surgery in patients with facial asymmetry: A systematic review. J Craniomaxillofac Surg 49:763–774. https://doi.org/10.1016/j.jcms.2021.04.010
De Momi E, Chapuis J, Pappas I, Ferrigno G, Hallermann W, Schramm A, Caversaccio M (2006) Automatic extraction of the mid-facial plane for cranio-maxillofacial surgery planning. Int J Oral Maxillofac Surg 35:636–642. https://doi.org/10.1016/j.ijom.2006.01.028
Ajmera DH, Hsung RT, Singh P, Wong NSM, Yeung AWK, Lam WYH, Khambay BS, Leung YY and Gu M (2022) Three-dimensional assessment of facial asymmetry in Class III subjects. Part 1: a retrospective study evaluating postsurgical outcomes. Clin Oral Investig. https://doi.org/10.1007/s00784-022-04463-4
Huang L, Wang Z, Shan Z, Yeung AWK, Yang Y, Liang Z, Gu M (2022) Nasal asymmetry changes during growth and development in 6- to 12-year-old children with repaired unilateral cleft lip and palate: A 3D computed tomography analysis. J Anat 240:155–165. https://doi.org/10.1111/joa.13538
AlHadidi A, Cevidanes LHS, Mol A, Ludlow J, Styner M (2011) Comparison of two methods for quantitative assessment of mandibular asymmetry using cone beam computed tomography image volumes. Dentomaxillofac Radiol 40:351–357. https://doi.org/10.1259/dmfr/13993523
Damstra J, Fourie Z, De Wit M, Ren Y (2012) A three-dimensional comparison of a morphometric and conventional cephalometric midsagittal planes for craniofacial asymmetry. Clin Oral Investig 16:285–294. https://doi.org/10.1007/s00784-011-0512-4
Wong T-Y, Fang J-J, Chung C-H, Huang J-S, Lee J-W (2005) Comparison of 2 methods of making surgical models for correction of facial asymmetry. J Oral Maxillofac Surg 63:200–208
Gateno J, Jajoo A, Nicol M, Xia JJ (2016) The primal sagittal plane of the head: a new concept. Int J Oral Maxillofac Surg 45:399–405. https://doi.org/10.1016/j.ijom.2015.11.013
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Ryan R, Hill S (2016) How to GRADE the quality of the evidence. Cochrane consumers and communication group, Version 3.0, available at http://cccrg.cochrane.org/author-resources.
Berssenbrugge P, Berlin NF, Kebeck G, Runte C, Jung S, Kleinheinz J, Dirksen D (2014) 2D and 3D analysis methods of facial asymmetry in comparison. J Craniomaxillofac Surg 42:e327–e334. https://doi.org/10.1016/j.jcms.2014.01.028
Jajoo A, Nicol M, Gateno J, Chen K-C, Tang Z, Chowdhury T, Li J, Shen S, Xia J (2018) Calculating the Midsagittal Plane for Symmetrical Bilateral Shapes: Applications to Clinical Facial Surgical Planning. ArXiv/abs/180305853. https://doi.org/10.48550/arXiv.1803.05853
Ortún-Terrazas J, Fagan MJ, Cegoñino J, Illipronti-Filho E and Pérez del Palomar A (2020) Towards an early 3D-diagnosis of craniofacial asymmetry by computing the accurate midplane: A PCA-based method. Methods Programs Biomed. Update. 191. https://doi.org/10.1016/j.cmpb.2020.105397
Zhu Y, Zheng S, Yang G, Fu X, Xiao N, Wen A, Wang Y and Zhao Y (2020) A novel method for 3D face symmetry reference plane based on weighted Procrustes analysis algorithm. BMC Oral Health 20. https://doi.org/10.1186/s12903-020-01311-3
Hsiao YC and Fang JJ (2022) An Automatic Voxel-Based Method for Optimal Symmetry Plane Generation for the Maxillofacial Region in Severe Asymmetry Cases. J Clin Med 11. https://doi.org/10.3390/jcm11195689
Tan WJ, Kang Y, Dong ZW, Chen C, Yin XX, Su Y, Zhang YC, Zhang L, Xu LS (2019) An Approach to Extraction Midsagittal Plane of Skull From Brain CT Images for Oral and Maxillofacial Surgery. IEEE Access 7:118203–118217. https://doi.org/10.1109/access.2019.2920862
An S, Lee J-Y, Chung CJ, Kim K-H (2017) Comparison of different midsagittal plane configurations for evaluating craniofacial asymmetry by expert preference. Am J Orthod Dentofacial Orthop 152:788–797. https://doi.org/10.1016/j.ajodo.2017.04.024
Lee EH, Yu HS, Lee KJ, Han SS, Jung HD, Hwang CJ (2020) Comparison of three midsagittal planes for three-dimensional cone beam computed tomography head reorientation. Korean J Orthod 50:3–12. https://doi.org/10.4041/kjod.2020.50.1.3
Economou S, Stoustrup P, Kristensen KD, Dalstra M, Küseler A, Herlin T, Pedersen TK (2018) Evaluation of facial asymmetry in patients with juvenile idiopathic arthritis: Correlation between hard tissue and soft tissue landmarks. Am J Orthod Dentofacial Orthop 153:662-672.e1. https://doi.org/10.1016/j.ajodo.2017.08.022
Ryu HS, An KY, Kang KH (2015) Cone-beam computed tomography based evaluation of rotational patterns of dentofacial structures in skeletal Class III deformity with mandibular asymmetry. Korean J Orthod 45:153–163. https://doi.org/10.4041/kjod.2015.45.4.153
Dobai A, Markella Z, Vizkelety T, Fouquet C, Rosta A, Barabas J (2018) Landmark-based midsagittal plane analysis in patients with facial symmetry and asymmetry based on CBCT analysis tomography. J Orofac Orthop 79:371–379. https://doi.org/10.1007/s00056-018-0151-3
Kim MS, Lee EJ, Song IJ, Lee JS, Kang BC, Yoon SJ (2015) The location of midfacial landmarks according to the method of establishing the midsagittal reference plane in three-dimensional computed tomography analysis of facial asymmetry. Imaging Sci Dent 45:227–232. https://doi.org/10.5624/isd.2015.45.4.227
Wong T-Y, Liu J-K, Fang J-J, Wu T-C, Tu Y-H (2014) Use of the matching optimal symmetry plane method in planning surgical correction of facial asymmetry–a preliminary report of 20 patients. J Oral Maxillofac Surg 72:1180.e1–13. https://doi.org/10.1016/j.joms.2014.02.020
Wong TY, Liu JK, Wu TC, Tu YH, Chen KC, Fang JJ, Cheng KH, Lee JW (2018) Plane-to-plane analysis of mandibular misalignment in patients with facial asymmetry. Am J Orthod Dentofacial Orthop 153:70–80. https://doi.org/10.1016/j.ajodo.2017.05.032
Zhang D, Wang S, Li J, Zhou YH (2018) Novel method of constructing a stable reference frame for 3-dimensional cephalometric analysis. Am J Orthod Dentofacial Orthop 154:397–404. https://doi.org/10.1016/j.ajodo.2017.11.038
Ajmera DH, Zhang C, Ng JHH, Hsung RT, Lam WYH, Wang W, Leung YY, Khambay BS, Gu M (2023) Three-dimensional assessment of facial asymmetry in class III subjects, part 2: evaluating asymmetry index and asymmetry scores. Clin Oral Investig 27:5813–5826. https://doi.org/10.1007/s00784-023-05193-x
Baek C, Paeng JY, Lee JS, Hong J (2012) Morphologic evaluation and classification of facial asymmetry using 3-dimensional computed tomography. J Oral Maxillofac 70:1161–1169. https://doi.org/10.1016/j.joms.2011.02.135
Choi HW, Kim B, Kim JY, Huh JK and Park KH (2019) Three-dimensional computed tomography evaluation of craniofacial characteristics according to lateral deviation of chin. Maxillofac. Plast. Reconstr. Surg. 41. https://doi.org/10.1186/s40902-019-0241-1
Feng B, Wang Y, Ouyang W, Yu M, Wang H (2021) Construction and validity of a midsagittal plane based on the symmetry of a 3-dimensional model of the relevant cranial base. Am J Orthod Dentofacial Orthop 159:e49–e58. https://doi.org/10.1016/j.ajodo.2020.09.008
Jo H, Ohe JY, Lee JW, Lee BS, Jung J (2021) Posterior bending osteotomy: An effective measure to secure facial symmetry in orthognathic surgery. J Craniomaxillofac Surg 49:538–544. https://doi.org/10.1016/j.jcms.2021.01.021
Kwon SM, Hwang JJ, Jung YH, Cho BH, Lee KJ, Hwang CJ, Choi SH (2019) Similarity index for intuitive assessment of three-dimensional facial asymmetry. Sci Rep 9:10959. https://doi.org/10.1038/s41598-019-47477-x
Lee HJ, Lee S, Lee EJ, Song IJ, Kang BC, Lee JS, Lim HJ, Yoon SJ (2016) A comparative study of the deviation of the menton on posteroanterior cephalograms and three-dimensional computed tomography. Imaging Sci Dent 46:33–38. https://doi.org/10.5624/isd.2016.46.1.33
Oh MH, Kang SJ, Cho JH (2018) Comparison of the three-dimensional structures of mandibular condyles between adults with and without facial asymmetry: A retrospective study. Korean J Orthod 48:73–80. https://doi.org/10.4041/kjod.2018.48.2.73
Song HS, Choi SH, Cha JY, Lee KJ, Yu HS (2017) Comparison of changes in the transverse dental axis between patients with skeletal Class III malocclusion and facial asymmetry treated by orthognathic surgery with and without presurgical orthodontic treatment. Korean J Orthod 47:256–267. https://doi.org/10.4041/kjod.2017.47.4.256
Thiesen G (2016) Determining the midsagittal reference plane for evaluating facial asymmetries. Am J Orthod Dentofacial Orthop 150:908–909. https://doi.org/10.1016/j.ajodo.2016.08.016
Udomlarptham N, Lin CH, Wang YC, Ko EWC (2018) Does two-dimensional vs. three-dimensional surgical simulation produce better surgical outcomes among patients with class III facial asymmetry? Int J Oral Maxillofac Surg 47:1022–1031. https://doi.org/10.1016/j.ijom.2018.02.014
Vernucci RA, Aghazada H, Gardini K, Fegatelli DA, Barbato E, Galluccio G, Silvestri A (2019) Use of an anatomical mid-sagittal plane for 3-dimensional cephalometry: A preliminary study. Imaging Sci Dent 49:159–169. https://doi.org/10.5624/isd.2019.49.2.159
Mangal U, Arum H, Huisoo K, Jung YH, Lee KJ, Yu HS, Hwang JJ and Choi SH (2021) Tomographic similarity scan with a computed modified absolute mandibular midsagittal plane for precise and objective localization of mandibular asymmetry. Comput. Biol. Med. 134. https://doi.org/10.1016/j.compbiomed.2021.104465
Han WJ, Hwang JJ, Jung YH, Cho BH, Lee KJ, Yu HS and Choi SH (2020) A New Approach to Set the Absolute Midsagittal Plane of the Mandible Using a Similarity Index in Skeletal Class III Patients with Facial Asymmetry. Appl. Sci.10. https://doi.org/10.3390/app10238550
Zheng X, Wang L, Zhang B, Bai X, Qin K, Tian Y, Zhao R, Liu S, Wang J, Zhao Z (2018) Accuracy of two midsagittal planes in three-dimensional analysis and their measurement in patients with skeletal mandibular deviation: a comparative study. Br J Oral Maxillofac Surg 56:600–606. https://doi.org/10.1016/j.bjoms.2018.06.009
Grissom MK, Gateno J, English JD, Jacob HB, Kuang T, Gonzalez CE, Yuan P, Deng HH, Frick CJ, Kim D, Hassan A, Xia JJ (2022) Midsagittal Plane First: Building a Strong Facial Reference Frame for Computer-Aided Surgical Simulation. J Oral Maxillofac Surg 80:641–650. https://doi.org/10.1016/j.joms.2021.11.016
Teng C, Liu C, Yu Q and Liu S (2021) Cone-beam Computed Tomography-based three-dimensional cephalometric analysis of mandible symmetry and the occlusal plane of adult patients with high-angle skeletal class III malocclusion and jaw deformity. Arch. Oral Biol. 127. https://doi.org/10.1016/j.archoralbio.2021.105157
Teng C, Zhong T, Yu Q (2022) Relationships between jaw deformity and the occlusal plane in cone beam computed tomography scans. J Prosthet Dent 128:49–54. https://doi.org/10.1016/j.prosdent.2020.12.006
Lv WX, Nie Q, Gu Y (2021) Three-dimensional analysis of mandibular characteristics in patients with skeletal Class II malocclusion and chin deviation. Am J Orthod Dentofacial Orthop 160:392–400. https://doi.org/10.1016/j.ajodo.2020.04.037
Lee JK, Jung PK, Moon CH (2014) Three-dimensional cone beam computed tomographic image reorientation using soft tissues as reference for facial asymmetry diagnosis. Angle Orthod 84:38–47. https://doi.org/10.2319/112112-890.1
Chang YJ, Ruellas ACO, Yatabe MS, Westgate PM, Cevidanes LHS, Huja SS (2017) Soft Tissue Changes Measured With Three-Dimensional Software Provides New Insights for Surgical Predictions. J Oral Maxillofac Surg 75:2191–2201. https://doi.org/10.1016/j.joms.2017.05.010
Lo LJ, Weng JL, Ho CT, Lin HH (2018) Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognathic surgery in patients with prognathism. PLoS ONE 13:e0200589. https://doi.org/10.1371/journal.pone.0200589
Hajeer MY, Ayoub AF, Millett DT (2004) Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br J Oral Maxillofac Surg 42:396–404. https://doi.org/10.1016/j.bjoms.2004.05.006
Kwon TG, Park HS, Ryoo HM, Lee SH (2006) A comparison of craniofacial morphology in patients with and without facial asymmetry–a three-dimensional analysis with computed tomography. Int J Oral Maxillofac Surg 35:43–48. https://doi.org/10.1016/j.ijom.2005.04.006
Acknowledgements
None
Funding
The authors received no financial support for the research.
Author information
Authors and Affiliations
Contributions
D.H.A., P.S. and M.G. conceptualized the methodology, D.H.A. and P.S. performed data curation, investigation, formal analysis, and wrote reviewed and edited the original draft, M.G., Y.Y.L., and B.S.K. supervised the methodology, reviewed and edited the original draft, and M.G. also administered the project and resources and validation. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
Ethics approval was obtained from the local institutional review board (IRB) of the University/Hospital Authority (approval number UW 19–377) before the commencement of this study.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ajmera, D.H., Singh, P., Leung, Y.Y. et al. Establishment of the mid-sagittal reference plane for three-dimensional assessment of facial asymmetry: a systematic review. Clin Oral Invest 28, 242 (2024). https://doi.org/10.1007/s00784-024-05620-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05620-7