Abstract
Sexual minority adolescents (SMA) have a disproportionately high prevalence of victimisation, self-harm, and depressed mood, relative to the general population. Yet, the contributing and mechanistic factors are unclear. We aim to explore the directional relationship between victimisation and self-harm and depressed mood, with poor sleep quality as a possible mediator. A secondary data analysis was conducted using a nationally representative birth cohort in the United Kingdom, where participants self-identified as sexual minority (N = 1922, aged 11–13, 67.1% female) and their parents completed questionnaires and interviews when the participants were aged 11, 14 and 17. Logistic and linear regression were used to test whether victimisation prospectively predicted self-harm and depressed mood with mediation analyses conducted to assess if sleep onset latency and nocturnal awakening mediated their relationships. After adjusting for demographic factors and baseline self-harm and depressed mood, victimisation at age 11 significantly predicted self-harm (OR = 1.40, p < .01) and depressed mood (B = 0.024, SE = 0.01, p < .05) at age 17. In the mediation analyses, frequent nocturnal awakening at age 14, but not sleep onset latency, significantly mediated the effect of victimisation at age 11 on self-harm (indirect effect B = 0.008, SE = 0.004, 95%CI = 0.001-0.017) and depressed mood (indirect effect B = 0.005, SE = 0.002 95%CI = 0.001-0.010) at age 17. Our findings supported that victimisation contributed to negative mental health among SMA. Poor sleep quality could be an indicator of maladjustment with victimisation, which further increased vulnerability to negative mental health. Victimisation and sleep quality could be important assessment targets in mental health campaign among sexual minority adolescents.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Sexual minority adolescents (SMA) were noted to have increased risk of developing many negative health outcomes [1–2]. A recently published Just Like Us report [3] including 2,934 U.K. students aged 11–18, found that 42% of SMA experienced bullying, compared to 21% of non-SMA. The report also found SMA to have tripled the prevalence of self-injury behaviours, compared to non-SMA. While these evidence converged to indicate a higher prevalence of negative mental health outcomes among SMA, the underlying contributors and mechanistic factors were unclear and needed to be studied to facilitate the design of prevention and intervention for mental health problems of SMA.
Victimisation, self-harm, and depressed mood
Victimisation was one of the main risk factors discussed in the literature for negative health outcomes among SMA. Victimisation was found to be about three times more common among SMA than non-SMA (see [4] for a meta-analytic review). Based on the Minority Stress Theory [5], sexual minority faced social stressors as a minority, e.g., prejudice, micro-aggression, homophobic victimisation, in addition to other stressors faced by non-sexual minority, increasing their vulnerability to mental health problems [6–7]. Therefore, conceivably, it might not be the sexual minority status per se, but the associated minority stressors contributing to negative mental health outcomes.
While existing research showed a significant association between victimisation and self-harm among the general adolescent population [8–9], relatively fewer studies focused on self-harm among SMA. Meta-analytical data [10] showed that 40.5% of the sexual minority population experienced self-harm, versus 24.4% of non-sexual minority. Another recent meta-analysis [4] stated that there was no conclusive indication regarding the causal relationship and mechanistic factors between victimisation and self-harm, since most existing studies were cross-sectional. Existing cross-sectional data showed that there were interrelations among victimisation and self-harm with other social factors, such as sense of connection with the social circle [11], internalised homophobia [12], as well as distress in hiding their sexual identity [13]. Among the limited studies with longitudinal designs, Burton and colleagues [6] found that sexual minority status at Time 1 prospectively predicted suicidal thoughts and behaviours at Time 2 (6 months later) and their association was mediated by sexual minority specific victimisation at Time 2. Such results suggested that victimisation was related to suicidal thoughts and behaviours, yet their directional relationship could be better inferred if these three factors were measured at different time-points [14]. Liu and Mustanski [15] assessed the prospective relationship between victimisation and self-harm among youths (aged 16–20) and found that victimisation due to sexual or gender minority status was one of the strongest predictors of self-harm apart from history of suicide. In addition, using a nationally representative USA youth sample (mean age = 15.9), Teasdale & Bradley-Engen [16] found that same-sex attraction and victimisation prospectively predicted suicidal attempts. Using a co-twin control design, O’Reilly and colleagues [2] recently reported that SMA were around 2 times more likely to self-harm or attempt suicide, relative to non-SMA, after adjusting for genetic and shared environmental factors. While these findings appeared to suggest victimisation as a predictor of self-harm, participants’ baseline self-harm behaviours were not controlled, limiting the inference of the individual contribution of victimisation.
Apart from self-harm, depressed mood was also found to be more prevalent among SMA than non-SMA [17]. For example, Burton and colleagues [6] included 197 students aged 14 to 19 and found that victimisation was associated with sexual minority status and depressed mood. la Roi and colleagues [18] found that among SMA (N = 153), victimisation mediated the relationship between sexual identity and later depression. However, in their study, self-reported victimisation was measured before sexual orientation was measured, which limited the inference on their temporal relationship. Another study using an England prospective cohort [19] found that victimisation mediated the difference in levels of depression between SMA (N = 187) and non-SMA (N = 3948). However, the sample did not include individuals born in other nations in the UK. In addition, all the aforementioned studies had less than 250 SMA participants [6, 18, 19] and studies with a larger number of SMA participants were needed to further verify the temporal association among victimisation and negative mental health outcomes.
The role of sleep in mental health outcomes
Sleep problems were found to be more prevalent among SMA than non-SMA [20,21,22,23]. This could possibly be due to SMA’s increased exposure to victimisation, which heightened cognitive and emotional arousal, disrupting one’s sleep experience [24]. Research conducted among the general adolescent population showed that sleep problems prospectively predicted negative mood and self-harm [25,26,27], and sleep problems mediated the effect of victimisation on depressive symptoms [28, 29]. The link between sleep problems and negative mental health outcomes could be explained by sleep’s role in emotional regulation, which potentially affected individuals’ impulsivity and tendency towards self-injury behaviours (see [30] for a review). Despite the higher prevalence of victimisation and negative mental health in SMA, to the best knowledge of the authors, no existing study investigated the mediating role of sleep problems on victimisation and depressive symptoms and self-harm among the sexual minority population [31].
The current study
This study investigated if victimisation prospectively predicted self-harm and depressed mood in SMA and whether poor sleep quality mediated the relationship, since sleep quality was (1) relatively less stigmatised, (2) easier to measure when compared to victimisation and (3) found to predict diverse negative mental health outcomes [20, 27]. We examined the difference in the types of victimisation experience and self-harm between SMA and non-SMA among our sample. We aimed to build on the limited existing longitudinal studies on victimisation and self-harm in SMA, e.g [6, 15, 16], by (1) measuring the predictor (victimisation), mediator (sleep quality) and outcome (self-harm and depressed mood) at three different time-points, allowing inference regarding temporal relationships [14]; (2) including the baseline measure of depressed mood and self-harm as covariates in the prospective analyses to more clearly gauge the contributions of victimisation and poor sleep quality; and (3) investigating the research questions using a nationally representative U.K. cohort which included participants across the four nations in the country. We hypothesized that the prevalence of victimisation and self-harm was higher for SMA than non-SMA. We also hypothesized that among SMA, victimisation at age 11 was a predictor for self-harm and depressed mood at age 17 after adjusting for the corresponding baseline measures. The relationship between victimisation and self-harm/depressed mood was hypothesized to be mediated by poor sleep quality at age 14.
Methods
Design
To investigate the research questions, we conducted a secondary data analysis using the Millennium Cohort Study (MCS), a nationally representative birth cohort of about 18,818 participants born in the years 2000–2002 across the nations in the UK [32]. Participants and their parents in the MCS provided informed consent before the data collection commenced and the current study received ethical approval for secondary data analysis. We extracted the data from the MCS when participants were at age 11, 14, and 17. The predictor was participants’ experience of age-11 victimisation, mediator was age-14 sleep quality and outcomes were age-17 self-harm and depressed mood (Sweep 7) (see Measures for details).
Participants
In the MCS, 13,469 adolescents participated at age 11, with 11,872 at age 14, and 10,757 at age 17. Participants were included in this study if they have participated in these three time-points and completed the measures on victimisation and sexual identity (Supplementary Fig. 1). The final sample included 1922 SMA and 6900 non-SMA and their descriptive information was described in Table 1.
Measures
Sexual identity
Participants were asked to select one of the following options to best describe how they currently think of themselves, “Completely heterosexual/straight; Mainly heterosexual/straight; Bisexual; Mainly gay or lesbian; Completely gay or lesbian; Other; Do not know; not applicable; Prefer not to say”. Similar to other cohort studies, e.g [19, 33, 34], we coded those describing themselves as “Completely heterosexual/straight” as non-SMA, while those selecting “Not applicable or Prefer not to say” were excluded from the analysis with the rest, who were not exclusively heterosexual or SMA.
Victimisation
At age 11, the adolescent participants reported the frequency of being hurt or picked on by other children with the following options, “most days”, “about once a week”, “about once a month”, “every few months”, “less often”, or “Never”. The responses were on a 1–6 scale where a smaller number represented more frequent experiences of victimisation. Participant’s parents were also asked if the participant has been picked on or bullied by other children and they responded “not true”, “somewhat true”, or “certainly true”. Given our primary interests on SMA’s self-reported depressed mood and self-harm behaviours, we used participants’ self-reported victimisation as the predictor in the analyses and reported descriptive data on self-reported and parent-reported victimisation (see Results). We also included the data of victimisation at age 14 for comparison analyses with non-SMA. At age 14, participants self-reported whether they had been exposed to a range of victimisation experiences, as yes/no binary items (See Table 2 for the types of victimisation experiences assessed). We coded victimisation at both ages as binary variables (Yes/No), where participants endorsing at least one victimisation experience were coded as having been victimised. For these items, there was an option of “Don’t know/Don’t wish to answer/No answer” and those selecting these responses were not included for analyses in this study.
Self-harm
At age 17, self-harm was measured based on the Edinburgh Study of Youth Transitions [35], where participants completed 5 binary items (Yes/No) regarding whether they had self-harmed by different means, including cutting or stabbing, burning, bruising or pinching, taking an overdose of tablets or pulling out hair, in the past year (Supplementary Table 3). They were also asked to state if they had used any other ways to hurt themselves in the past year. Participants endorsing any self-harm behaviour were coded as having performed self-harm. At age 14, participants were asked if they had hurt themselves on purpose in any way and they provided a response of yes or no.
Depressed mood
At age 17, depressed mood was measured by the following item in the Kessler 6 scale [36], “During the last 30 days, how often did you feel so depressed that nothing could cheer you up?” At age 14, depressed mood was measured by the short version of the Mood and Feeling Questionnaire [37], where there were 13 statements regarding participants’ recent mood and feeling, e.g. “I hated myself” or “I did everything wrong”. For each item, the response options were “not true”, “sometimes”, or “true”. The total score ranged from 13 to 39 and the scale had good internal consistency (α = 0.94). A higher score indicated higher level of depressive symptoms in both time-points.
Sleep quality
Sleep quality was measured by participants’ sleep onset latency (SOL), and nocturnal awakening at age 14, where they reported how long they usually took to fall asleep and how frequency they awakened during sleep at the last 4 weeks (See Table 1 for details). Participants were also asked about their typical bedtime and wake time during school days for descriptive information regarding sleep patterns (Table 1).
Demographic variables
Participants’ age, gender, ethnicity, and weekly family income were measured at age 14 (Table 1). The response options and details were reported in Supplementary Table 1.
Data analysis plan
SPSS version 28 was used for all data analysis. Group differences were analysed using Chi-square or Mann-Whitney U test, given unequal variance. Correlational analyses were conducted to assess the cross-sectional relationship among victimisation, sleep quality, depressed mood, and self-harm at age 14. Binary logistic and linear regression were used to analyse the temporal relationship between victimisation, poor sleep quality with self-harm and depressed mood. The variables were tested for multi-collinearity and their variance inflation factor were lower than 10, indicating no significant concern of multi-collinearity. The regression analyses were conducted by entering demographic variables and baseline (age-14) of the outcome measure at step 1, victimisation at step 2 and SOL and nocturnal awakening at step 3. In view of multiple comparison and risk of inflated type-1 error, all p-values were adjusted following the Benjamini-Hochberg procedure with a false discovery rate (FDR) of 5%. Statistical significance was determined by an adjusted p-value, pfdr <0.05. For the mediation hypotheses, a series of regression analyses were performed using the PROCESS Macro [38]. The regression analyses included Age-11 victimisation as the predictor, either age-14 SOL or nocturnal awakening as the mediator, and either age-17 self-harm or depressed mood as the outcome, with the corresponding measure at age 14 as the covariate (Fig. 1 and Fig. 2a and b). The model with self-harm as outcome was tested using logistic regression given that self-harm was coded as a binary (Yes/No) variable (Fig. 2a), while the model with depressed mood as outcome was tested using linear regression model given depressed mood was coded as a continuous variable (Fig. 2b). A bootstrap re-sample of 5000 was used to estimate the standard error. Significant mediation effect was inferred by a 95% confidence interval (95%CI) not containing 0.
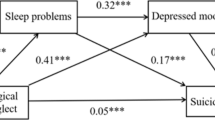
Nocturnal awakening’s mediation effect on victimisation and self-harm. Note Age 11 Victimisation has a significant indirect effect on Age 17 Self-harm through nocturnal awakening, B = 0.008, SE = 0.004, 95% CI: 0.001 − 0.017. Reported values are unstandardized regression coefficients and standard error. *95% CI do not include 0
Mediation results for Depressed Mood. Note Age 11 Victimisation has a significant indirect effect on Age 17 Depressed Mood through nocturnal awakening, B = 0.005, SE = 0.002, 95% CI: 0.001 − 0.010. Reported values are unstandardized regression coefficients and standard error. * 95% CI do not include 0
Results
Results from Mann-Whitney U test indicated that SMA had a higher level of depressive symptoms (pfdr<0.001), later bedtime (pfdr<0.001), later wake time (pfdr<0.001), longer SOL (pfdr<0.001), and more frequent nocturnal awakening (pfdr<0.001) than non-SMA. We conducted chi-square tests between SMA and non-SMA on victimisation and self-harm. The results showed that at age 11, both self-reported [x2(1) = 50.10, pfdr<0.001] and parent-reported victimisation [x2(1) = 31.71, pfdr<0.001], has a higher prevalence among SMA than non-SMA. In general, there was a higher rate of victimisation noted in self-reported data than parent-reported data for both SMA (64.8% versus 28.8%) and non-SMA (55.8 versus 22.6%) (Table 2). At age 14, SMA had a higher prevalence of all victimisation experiences, except for “having been hit/used weapon against”, than non-SMA. Of note, the prevalence of victimisation among SMA ranged from 3.5% (for being hit/used weapon against) to 53.8% (being insulted/threatened/shouted at) depending on types (Table 2). Regarding self-harm, at both time-points, SMA had a higher prevalence on all self-harm means than non-SMA. The prevalence of self-harm ranged from 6.6% (overdose of tablets) to 32.8% (self-bruising or pinching) among SMA, depending on the means (Supplementary Table 3).
Cross-sectional relationship among Victimisation, sleep quality, self-harm, and depressed mood
Results from the Spearman Rank test showed significant cross-sectional associations among victimisation (all types considered) with poor sleep quality, self-harm, and depressed mood (pfdr<0.001). the individual correlation between each type of victimisation experience with sleep, self-harm and depressed mood were reported in Supplementary Table 2.
Prospective analyses on victimisation, sleep quality, self-harm & depressed mood
Results from the logistic regression model showed that victimisation (OR = 1.40, 95%CI: 1.13–1.74, pfdr =0.002), and nocturnal awakening (OR = 1.18, 95%CI: 1.09–1.28, pfdr<0.001) significantly predicted self-harm [x2(8) = 248.37, pfdr<0.001] after adjusting for the effects of demographic factors and self-harm at baseline (OR = 3.70, 95%CI: 2.89–4.75, pfdr<0.001) (Table 3). The results of mediation model showed that victimisation had a significant direct (B = 0.073, SE = 0.020, OR = 1.08, 95% CI = 0.033 − 0.11) and indirect effect on self-harm through nocturnal awakening (B = 0.008, SE = 0.004, OR = 1.008, 95% CI = 0.001 – 0.017) (Fig. 1). For the model with SOL as mediator, the indirect effect of victimisation on self-harm was not statistically significant (B = 0.001, SE = 0.003, OR = 1.001, 95% CI=-0.004 – 0.007) (Supplementary Fig. 2).
Regarding depressed mood, results from linear regression analysis showed that victimisation (B = 0.024, SE = 0.010, pfdr=0.016), SOL (B=-0.041, SE = 0.019, pfdr=0.035), and nocturnal awakening (B = 0.048, SE = 0.019, pfdr=0.012) significantly predicted depressed mood (R2 = 0.395, F8,1770=40.65, pfdr<0.001) after adjusting for the effect of demographic factors and depressed mood at baseline (B = 0.046, SE = 0.004, pfdr<0.001) (Table 3). In the mediation model with victimisation as the predictor, nocturnal awakening as the mediator, and depressed mood as the outcome, victimisation had a significantly direct (B = 0.034, SE = 0.010, 95% CI = 0.014 – 0.054) and indirect effect through nocturnal awakening (B = 0.005, SE = 0.002, 95% CI = 0.0006 – 0.0096) on depressed mood (Fig. 1). For the model with SOL as a mediator, the indirect effect of victimisation on depressed mood was not statistically significant (B = 0.001, SE = 0.002, 95% CI = − 0.003 – 0.005) (Supplementary Fig. 2).
Discussion
The primary aim of this study was to investigate the role of victimisation in the development of self-harm and depressed mood among SMA and the results indicated that victimisation prospectively predicted self-harm and depressed mood after adjusting for demographic factors and baseline self-harm and depressed mood. Frequent nocturnal awakening, as a measure of poor sleep quality, further mediated the effect of victimisation on self-harm and depressed mood. The interpretation of the findings is discussed in detail as follows,
Victimisation and self-harm in SMA
In line with existing studies using samples from China [21], Sweden [38], Canada [39] and another UK birth cohort [34], our findings showed that SMA were generally more likely to experience victimisation, compared to non-SMA. In addition, while the prevalence of victimisation among SMA was estimated to be about three times more common than non-SMA [4], our data showed that the discrepancy on victimisation between SMA and non-SMA depended on the type of victimisation experience. For instance, while the prevalence of sexual assault was lower than most other victimisation experiences assessed, its prevalence among SMA (5.7%) was about 2–3 times higher than non-SMA (2.1%). However, the difference on other victimisation experiences, e.g., physical violence, between SMA (26.2%) and non-SMA (20.6%) might appear not as big as sexual assault, potentially due to its higher prevalence among both SMA and non-SMA. Also, similar to other studies [2, 34], our SMA sample had a greater prevalence of self-harm than non-SMA and we further found the extent of discrepancy depended on the means of self-harm, with greatest discrepancy noted among more life-threatening self-injury behaviours, e.g., overdose of tablets, self-cutting or stabbing. These findings collectively highlighted the importance of comprehensive assessment on victimisation types and self-harm means in understanding their prevalence among adolescents.
Victimisation as an early predictor for later development of self-harm and depressed mood
Our findings showed that victimisation prospectively predicted negative mental health outcomes in SMA. Regarding self-harm, our results were consistent with existing studies conducted among older adolescents [15], where there was a prospective relationship between victimisation and self-harm in SMA populations. We also included more comprehensive measures of self-harm, as well as setting its baseline as covariate in the statistical analyses. The enhanced methodology quality provided further support for the predictive role of victimisation of self-harm and depressed mood among SMA. Our findings were also consistent with the result patterns found in the general adolescent population [40] that victimisation could prospectively predict later development of self-harm among SMA. For depressed mood, we found a prospective relationship between victimisation and depressed mood among the SMA population after adjusting for baseline depressed mood and other demographic factors. Our results were consistent with existing studies [18] which also found victimisation to predict depression among SMA, and we further verified the pattern of associations by using a nationally representative UK sample with a considerable number of SMA participants (N = 1922). These findings were in line with the Minority Stress Theory that the experience of victimisation and other minority stressors, contributed to the development of negative mental health outcomes among SMA.
The role of poor sleep quality in victimisation, self-harm and depressed mood in SMA
Our results were in line with existing cross-sectional data between victimisation and sleep quality among the SMA [21] and prospective data among general adolescent population [40]. To the best knowledge of the authors, our findings were among the first to show that poor sleep quality, particularly frequent nocturnal awakening, prospectively predicted self-harm and depressed mood, after adjusting for baseline self-harm and depressed mood, among SMA. The significant relationship between poor sleep quality and negative mental health outcomes could be understood with existing cognitive neuroscience literatures which showed that sleep health was essential for optimal brain functioning in affect regulation [30]). While sleep quality was fairly direct to assess and a less stigmatised issue than victimisation, our findings potentially indicated that sleep quality and frequency of nocturnal awakening could be good assessment targets to help identify the vulnerable population at risk of developing negative mental health outcomes.
Inconsistent with our hypothesis, SOL did not significantly mediate the effect of victimisation on self-harm or depressed mood, which appeared inconsistent with some studies [41]. While longer SOL generally represented poorer sleep quality, among adolescents, short SOL could also reflect sleep debt because of insufficient sleep. Indeed, existing studies have found that adolescents with insufficient sleep had shorter SOL than those with sufficient sleep [42]. Future studies which investigate both sleep duration and SOL, using both subjective and objective data could further address the role of SOL in SMA’s wellbeing.
On the other hand, our data showed that nocturnal awakening prospectively predicted depressed mood and self-harm and mediated the effect of victimisation on them. Frequent nocturnal awakening conceivably represented a higher level of nocturnal arousal and difficulty to relax, which could be a behavioural manifestation of unsatisfactory adjustment to victimisation, ultimately increasing individual’s vulnerability to negative mental health outcomes. Though we had no measure regarding the reasons for nocturnal awakening, frequent nocturnal awakening could also be due to nightmare or insomnia which could be triggered by victimisation or unpleasant experience. Despite the different interpretations of the findings, our results added to a recent that sleep health had an important contributing to wellbeing among SMA [25].
Limitations
Notwithstanding, this study had some limitations as follows. Firstly, we studied sexual minority as a homogenous group as other cohort studies [19, 33, 34], though a recent review stated that some specific sexual identities, e.g., bisexual, were at higher risk of developing negative mental health outcomes and were worth further investigation [23]. Secondly, the victimisation measure in this study did not capture the motivation/victim’s account of the victimisation experience, while some studies [6] showed that victimisation due to sexual orientation might have a stronger impact on mental health than due to other reasons. Thirdly, most of the measures were self-reported and future studies which include both self-reported and parent-reported and teacher-reported measures could more comprehensively address the role of victimisation on negative mental health outcomes. Fourthly, apart from victimisation and sleep problem, there were other unexplored factors, e.g. social connectedness, internalised homophobia/biphobia, which could be involved in the directional relationship among victimisation with self-harm and depressed mood [11,12,13].
Conclusion
To conclude, while existing studies consistently reported a higher prevalence of depressed mood and self-harm among SMA when compared to non-SMA, this study showed that victimisation experience, as a minority stressor, prospectively predicted these negative mental health outcomes. We additionally found that frequent nocturnal awakening among SMA, was a potential indicator of later development of negative mental health in SMA. Intervention studies which target sleep problems and victimisation experience among SMA will be helpful to further verify the directional relationship among these factors. Also, further longitudinal, and experimental data are needed to identify early indicators, or protective factors against self-harm and depressed mood, since if left untreated, their impact on wellbeing could persist into early adulthood [32] or have long-reaching implications on healthy development.
Data availability
This is a secondary data analysis and the details in accessing the data can be referred to the UK data service, https://ukdataservice.ac.uk/.
References
Amos R, Manalastas EJ, White R et al (2020) Mental health, social adversity, and health-related outcomes in sexual minority adolescents: a contemporary national cohort study. Lancet Child Adolesc Health 4:36–45. https://doi.org/10.1016/S2352-4642(19)30339-6
O’Reilly LM, Pettersson E, Donahue K et al (2021) Sexual orientation and adolescent suicide attempt and self-harm: a co-twin control study. J Child Adoles Psychiatr 62:834–841. https://doi.org/10.1111/jcpp.13325
Just Like Us. Growing up LGBT+: The impact of school, home and coronavirus on LGBT + young people (2021) https://www.justlikeus.org/wp-content/uploads/2021/11/Just-Like-Us-2021-report-Growing-Up-LGBT.pdf Accessed 20th February, 2023
Williams AJ, Jones C, Arcelus J et al (2021) A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ + young people with experiences of self-harm and suicide. PLoS ONE 16:e0245268. https://doi.org/10.1371/journal.pone.0245268
Meyer IH (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 129:674–697. https://doi.org/10.1037/0033-2909.129.5.674
Burton CM, Marshal MP, Chisolm DJ et al (2013) Sexual minority-related victimization as a mediator of mental health disparities in sexual minority youth: a longitudinal analysis. J Youth Adolesc 42:394–402. https://doi.org/10.1007/s10964-012-9901-5
Muehlenkamp JJ, Hilt LM, Ehlinger PP, McMillan T Nonsuicidal self-injury in sexual minority college students: a test of theoretical integration (2015). Child Adolesc Psychiat Ment Health 9:1–8. https://doi.org/10.1186/s13034-015-0050-y
Tucker JS, Ewing BA, Espelage DL et al (2016) Longitudinal associations of homophobic name-calling victimization with psychological distress and alcohol use during adolescence. J Adolesc Health 59:110–115. https://doi.org/10.1016/j.jadohealth.2016.03.018
Valencia-Agudo F, Burcher GC, Ezpeleta L, Kramer T (2018) Nonsuicidal self-injury in community adolescents: a systematic review of prospective predictors, mediators and moderators. J Adolesc 65:25–38. https://doi.org/10.1016/j.adolescence.2018.02.012
Batejan KL, Jarvi SM, Swenson LP (2015) Sexual orientation and non-suicidal self-injury: a meta-analytic review. Arch Suicide Res 19:131–150. https://doi.org/10.1080/13811118.2014.957450
Taliaferro LA, Muehlenkamp JJ (2017) Nonsuicidal self-injury and suicidality among sexual minority youth: risk factors and protective connectedness factors. Acad Pediatr 17:715–722. https://doi.org/10.1016/j.acap.2016.11.002
Rogers ML, Hom MA, Janakiraman R et al (2021) Examination of minority stress pathways to suicidal ideation among sexual minority adults: the moderating role of LGBT community connectedness. Psychol Sex Orientat Gend Diver 8:38–47. https://doi.org/10.1037/sgd0000409
McDermott E, Hughes E, Rawlings V (2018) The social determinants of lesbian, gay, bisexual and transgender youth suicidality in England: a mixed methods study. J Public Health 40:e244–e251. https://doi.org/10.1093/pubmed/fdx135
Maxwell SE, Cole DA (2007) Bias in cross-sectional analyses of longitudinal mediation. Psychol Methods 12:23–44
Liu RT, Mustanski B (2012) Suicidal ideation and self-harm in lesbian, gay, bisexual, and transgender youth. Am J Prev Med 42:221–228. https://doi.org/10.1016/j.amepre.2011.10.023
Teasdale B, Bradley-Engen MS (2010) Adolescent same-sex attraction and mental health: the role of stress and support. J Homosex 57:287–309. https://doi.org/10.1080/00918360903489127
Guz S, Kattari SK, Atteberry-Ash B et al (2021) Depression and suicide risk at the cross-section of sexual orientation and gender identity for youth. J Adolesc Health 68:317–323. https://doi.org/10.1016/j.jadohealth.2020.06.008
la Roi C, Kretschmer T, Dijkstra JK et al (2016) Disparities in depressive symptoms between heterosexual and lesbian, gay, and bisexual youth in a Dutch cohort: the TRAILS Study. J Youth Adolesc 5:440–456. https://doi.org/10.1007/s10964-015-0403-0
Robinson JP, Espelage DL, Rivers I (2013) Developmental trends in peer victimization and emotional distress in LGB and heterosexual youth. Pediatr 131:423–430. https://doi.org/10.1542/peds.2012-2595
Wong ML, Nagata JM, Barreto M (2024) Sleep and socioemotional outcomes among sexual and gender minority adolescents: a longitudinal Study. Arch Sex Behav 53:543–553. https://doi.org/10.1007/s10508-023-02732-1
Li P, Huang Y, Guo L et al (2017) Is sexual minority status associated with poor sleep quality among adolescents? Analysis of a national cross-sectional survey in Chinese adolescents. BMJ open 7:e017067. https://doi.org/10.1136/bmjopen-2017-017067
Patterson CJ, Tate DP, Sumontha J, Xu R (2018) Sleep difficulties among sexual minority adults: associations with family relationship problems. Psychol Sex Orientat Gend Divers 5:109–116. https://doi.org/10.1037/sgd0000264
Butler ES, McGlinchey E, Juster R-P (2019) Sexual and gender minority sleep: a narrative review and suggestions for future research. J Sleep Res 29:1–21. https://doi.org/10.1111/jsr.12928
van Geel M, Goemans A, Vedder PH (2016) The relation between peer victimization and sleeping problems: a meta-analysis. Sleep Med Rev 27:89–95. https://doi.org/10.1016/j.smrv.2015.05.004
Fang J, Wan Y, Zhang X et al (2022) Sleep duration trajectory during the transition to adolescence and subsequent risk of non-suicidal self-harm. Eur Child Adolesc Psychiatry 31:1–9. https://doi.org/10.1007/s00787-021-01768-9
Wong ML, Lau EYY, Wan JHY et al (2013) The interplay between sleep and mood in predicting academic functioning, physical health and psychological health: a longitudinal study. J Psychosom Res 74:271–277. https://doi.org/10.1016/j.jpsychores.2012.08.014
Matamura M, Tochigi M, Usami S et al (2014) Associations between sleep habits and mental health status and suicidality in a longitudinal survey of monozygotic twin adolescents. J Sleep Res 23:290–294. https://doi.org/10.1111/jsr.12127
Chang LY, Chang HY, Wu WC et al (2017) Body mass index and depressive symptoms in adolescents in Taiwan: testing mediation effects of peer victimization and sleep problems. Int J Obes 41:1510–1517. https://doi.org/10.1038/ijo.2017.111
Kwon M, Seo YS, Nickerson AB et al (2020) Sleep quality as a mediator of the relationship between cyber victimization and depression. J Nurs Scholarsh 52:416–425. https://doi.org/10.1111/jnu.12569
Porras-Segovia A, Perez-Rodriguez MM, López-Esteban P et al (2019) Contribution of sleep deprivation to suicidal behaviour: a systematic review. Sleep Med Rev 44:37–47. https://doi.org/10.1016/j.smrv.2018.12.005
Argyriou A, Goldsmith KA, Rimes KA (2021) Mediators of the disparities in depression between sexual minority and heterosexual individuals: a systematic review. Arch Sex Behav 50:925–959. https://doi.org/10.1007/s10508-020-01862-0
Centre for Longitudinal Studies. Millennium Cohort Study (2017) https://cls.ucl.ac.uk/cls-studies/millennium-cohort-study/ Accessed on 20th February, 2023
Jones A, Robinson E, Oginni O et al (2017) Anxiety disorders, gender nonconformity, bullying and self-esteem in sexual minority adolescents: prospective birth cohort study. J Child Psychol Psychiatr 58:1201–1209. https://doi.org/10.1111/jcpp.12757
Irish M, Solmi F, Mars B et al (2019) Depression and self-harm from adolescence to young adulthood in sexual minorities compared with heterosexuals in the UK: a population-based cohort study. Lancet Child Adolesc Health 3:91–98. https://doi.org/10.1016/S2352-4642(18)30343-2
McAra L, McVie S (2010) Youth crime and justice: key messages from the Edinburgh Study of Youth Transitions and Crime. Criminol Crim Justice 10:179–209. https://doi.org/10.1177/1748895809360971
Kessler RC, Barker PR, Colpe LJ et al (2003) Screening for serious mental illness in the general population. Arch Gen Psychiat 60:184–189. https://doi.org/10.1001/archpsyc.60.2.184
Thapar A, McGuffin P (1998) Validity of the shortened Mood and feelings Questionnaire in a community sample of children and adolescents: a preliminary research note. Psychiat Res 81:259–268. https://doi.org/10.1016/s0165-1781(98)00073-0
Hayes AF (2022) Introduction to mediation, moderation, and conditional process analysis: a regression-based approach (Third edition.). The Guilford Press
Priebe G, Svedin CG (2012) Online or off-line victimisation and psychological well-being: a comparison of sexual-minority and heterosexual youth. Eur Child Adolesc Psychiat 21:569–582. https://doi.org/10.1007/s00787-012-0294-5
Wong MM, Brower KJ, Zucker RA (2011) Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J Psychiatr Res 45:505–511. https://doi.org/10.1016/j.jpsychires.2010.09.005
Zhou Y, Guo L, Lu CY et al (2015) Bullying as a risk for poor sleep quality among high school students in China. PLoS ONE 10:e0121602
Reid A, Maldonado CC, Baker FC (2002) Sleep behavior of South African adolescents. Sleep 25:417–421
Acknowledgements
We sincerely thank the participants and the carers for participating in the Millennium Cohort Study.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Open access publishing enabled by City University of Hong Kong Library’s agreement with Springer Nature
Open access publishing enabled by City University of Hong Kong Library's agreement with Springer Nature
Author information
Authors and Affiliations
Contributions
AT and MLW conceptualized and designed the study. AT and MLW conducted the data analysis. AT drafted the initial manuscript. AT and MLW reviewed and revised the manuscript. MLW provided critical evaluation of manuscript drafts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tepman, A., Wong, M.L. The role of victimisation and sleep quality in self-harm and depression among sexual minority adolescents. A prospective cohort study. Eur Child Adolesc Psychiatry (2024). https://doi.org/10.1007/s00787-024-02444-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-024-02444-4