Abstract
Preschool screening of attention-deficit/hyperactivity disorder (ADHD) has been found too inaccurate to be clinically useful. This may be due to the known instability of ADHD symptoms from preschool onwards, and the use of a single screening only. We hypothesized that by identifying a group of children with persistent ADHD from preschool to school age and repeating the screening, the clinical usefulness of screening would increase. This study is part of the prospective longitudinal, population-based Norwegian Mother, Father and Child Cohort Study, with a diagnostic parent interview at 3.5 years and follow-up with parent questionnaires at ages 5 and 8 years (n = 707). We identified a group classified with ADHD at all three time points (persistent ADHD). We then used the Child Behavior Checklist ADHD DSM-oriented scale at ages 3.5 and 5 years to investigate the accuracies of single- and two-stage screening at different thresholds to identify children with persistent ADHD. About 30% of the children were classified with ADHD at least once across time (at ages 3.5, 5, and/or 8 years), but only 4% (n = 30) had persistent ADHD. At all thresholds, the two-stage screening identified children with persistent ADHD more accurately than single screening, mainly due to a substantial reduction in false positives. Only a small group of children were classified with persistent ADHD from preschool to school age, underlining that future screening studies should distinguish this group from those with fluctuating symptoms when estimating screening accuracies. We recommend a two-stage screening process to reduce false positives.
Similar content being viewed by others
Attention-deficit/hyperactivity disorder (ADHD) with persisting symptoms of hyperactivity–impulsivity and inattention often debuts in early childhood, yet is usually diagnosed after school entry [1, 2]. This is unfortunate, because early identification has been underlined as critical to the well-being of children and their families [3] and may alleviate the socioeconomic impact and burden of ADHD on society [4]. However, a recent meta-analysis concluded that future work is required to develop the most efficient strategy to identify young children with attention-deficit/hyperactivity disorder [5]. The reason for this recommendation was twofold: First, the early debut of ADHD symptoms is associated with negative consequences for the children and their families. Second, preschool intervention programs show promise in ameliorating symptoms [6, 7]. However, to date, a few pre-schoolers with ADHD symptoms have been offered interventions. One reason may be that hyperactive–impulsive symptoms are common in early childhood and have been found to decrease between the ages of 3 and 8 years in the general population [8], and inattentive symptoms may be difficult to detect [9]. Thus, early identification of ADHD through screening programs carries the inherent problem of misclassification, making it difficult to accurately separate children with persistent high levels of ADHD symptoms from those who will outgrow their problems. There is a need to investigate the screening of persistent high ADHD levels from preschool to school age.
A major challenge in ADHD screening at preschool age, with reasonable sensitivity (often set to ≥ 70% [10]), is the risk of also identifying many false-positive children. This would cause unnecessary concern for many families and increase the strain on healthcare services. Thus, repeated screening and multiple thresholds have been suggested [10, 11], but they need empirical support. A recent Chinese study of pupils aged 6–12 years found that a two-stage screening involving teachers (adding teacher interviews to traditional questionnaire-based screening) increased specificity from 80 to 93% while maintaining sensitivity at 83%, thus reducing the proportion of false positives and improving the clinical utility of school-based screening for ADHD [12]. That study recommended a two-stage screening process but concluded that further research is required to identify the optimal approach to screening for ADHD.
The present study aims to test a parent-reported two-stage-screening for ADHD at ages 3.5 and 5 years to identify children with persistent high levels of ADHD symptoms from preschool to school age. We hypothesized that this approach would be more accurate than a single screening at 3.5 years of age.
Method
Participants
The Norwegian Mother, Father, and Child Cohort Study (MoBa) is a population-based cohort study conducted by the Norwegian Institute of Public Health. From 1999 to 2008, pregnant Norwegian-speaking women having their first ultrasound were enrolled from all over Norway (n ~ 114.500 children; 41% participation rate) [13]. Nested within the MoBa is the ADHD substudy, which oversampled for children at risk using 11 items about ADHD from the MoBa questionnaire when the child was 3 years old. This study has previously been described in detail [14, 15]. About 80% of the invited participants (n = 2798) had scores ≥ 90th percentile on these 11 items. The rest were randomly selected children (n = 654) from MoBa. Thirty-five percent agreed to participate, and from 2007 to 2011, 1195 children (mean age 3.5 years) took part in a 1-day clinical assessment, including a diagnostic interview with their parents (mainly mothers). Fifteen mothers later withdrew from MoBa, leaving 1180 enrolled children who were followed up at 5 and 8 years of age. This study includes children with available screening data at 3.5 and 5 years of age, and information to define the ADHD outcome groups at 3.5, 5, and 8 years (n = 707).
Measures
Child sex was obtained from the Norwegian Medical Birth Registry.
Screening at 3.5 and 5 years of age
At 3.5 and 5 years, we used six items from the Child Behavior Checklist (CBCL)/1.5–5 Diagnostic and Statistical Manual of Mental Disorders (DSM)-oriented scale for ADHD (Can’t concentrate, Can’t sit still; Can’t stand waiting; Demands must be met immediately; Gets into everything; Quickly shifts activities) [16]. Mothers rated the CBCL items on a three-point Likert scale (not true, somewhat true, or very true; range 0–2).
A total of 707 children, 381 boys and 326 girls, had complete data. A bias test for attrition at 3.5, 5, and 8 years did not show any significant differences between included and lost children with respect to sex or percentage above ADHD threshold at any point in time. At 3.5 years of age, those lost to follow-up had a slightly higher mean CBCL score (5.49 vs 5.11; p < 0.05); while there was no significant difference at 5 years of age.
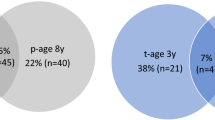
ADHD outcome at three time points (See Fig. 1)
At 3.5 years of age, the semi-structured Preschool Age Psychiatric Assessment (PAPA) interview [17] was developed for children from the ages of 2 to 5 years. The interviewer asks questions until they can decide whether the symptoms described meet the definitions provided in a glossary. A PAPA reliability study reported a test–retest intraclass correlation of 0.80 for classified ADHD [18]. In the present study, only ADHD symptoms persisting for ≥ 3 months were counted as present. In line with our earlier studies [14, 15], we used information from the PAPA, and defined ADHD by the DSM-IV-TR criteria, with at least six out of nine symptoms of hyperactivity–impulsivity and/or inattention [19]. A second blind rater rescored audiotapes of 79 randomly selected interviews, and the intraclass correlation was 0.98 for ADHD symptoms. Nineteen percent (222/1180) of the children met the symptom criteria for ADHD.
At 5 years of age, the mothers received the revised short form of the Conners’ Parent Rating Scale (CPRS-R: S) with 12 ADHD items comprising the ADHD index [20], as part of the 5-year MoBa questionnaire. The CPRS items were rated on a four-point Likert scale (not true, somewhat true, often true, or very true; range 0–3). The ADHD index has been found to have good validity for ADHD [21]. From all the responders to the 5-year MoBa questionnaire (n = 32,633, 49% girls), we created thresholds for ADHD to be present at the 95th percentile of the CPRS-R:S ADHD index scores: > 14.2 for boys and > 11 for girls. Using thresholds from the general population from which the children were drawn, reduced the problem of cross-cultural differences if using US cut-of scores, and is in line with a previous study [22]. Of the 1180 children, 966 (82%) participated at the age of 5 years, and 220 of these (23%) reached the ADHD classification based on these thresholds.
At 8 years of age, parents responded to the Child Symptom Inventory-4 (CSI-4), rated on a four-point Likert scale (never, sometimes, often, very often; range 0–3) [23]. We used the hyperactivity–impulsivity and inattention subscales, each with nine items, and dichotomized symptom counts where symptoms were scored as not present (never/sometimes = 0) or present (often/very often = 1). In line with the CSI-4 manual, children who reached the minimum number of symptoms necessary for the DSM-IV ADHD diagnosis with ≥ 6 on either subscale were classified with ADHD. Sixty-six percent (783/1180) of the participants at 3 years of age had data on the CSI-4 at 8 years of age. Of these children, 85 (11%) were classified with ADHD.
Ethics
MoBa and the initial data collection were based on a license from the Norwegian Data Protection Agency and approval from the Regional Committees for Medical and Health Research Ethics. The MoBa cohort is currently regulated by the Norwegian Health Registry Act. The current study was approved by the Regional Committees for Medical and Health Research Ethics (2017/1276).
Analytic plan
We divided the children into four groups based on the number of times (0, 1, 2, or 3) they had been classified with ADHD. We compared the mean ADHD scores for the groups with an analysis of variance with pairwise post hoc comparisons using Scheffe’s test. Because there were different ADHD outcome measures at ages 3.5, 5, and 8 years, we used z-transformation to obtain comparable scores. We then tested the ability of the CBCL DSM-oriented scale for ADHD to discriminate the ADHD persistent group (above threshold at all three time points) from the rest. With receiver-operating characteristic (ROC) analyses, we estimated the areas under the curves (AUCs) to quantify the overall accuracies of the single- and two-stage screening. The ROC curve graphically represents the probability of true positive results of ADHD as a function of the probability of false-positive results. For interpreting AUC values, the following guideline is recommended: < 0.70 = poor, 0.70–0.79 = fair, 0.80–0.89 = good, and 0.90–1.00 = excellent [24]. We estimated the CBCL scales’ sensitivity (Se; the probability that a measure correctly classifies a case as positive) and specificity (Sp; the probability that a measure correctly identifies non-cases as negative) for thresholds 6, 7, 8, and 9. Children who scored at or above a given threshold score were categorized as screen positive. We calculated the positive predictive values (PPVs, the probability of a true case given a positive test), negative predictive values (NPVs, the probability of a true non-case given a negative test), the positive-likelihood ratios (LRs, the probability of a child who has the disorder testing positive divided by the probability of a child who does not have the disorder testing positive), and negative LRs (the probability of a child who has the disorder testing negative divided by the probability of a child who does not have the disorder testing negative). LRs greater than 1 suggest the presence of the disorder being present, whereas LRs between 0 and 1 indicate its absence. LRs equal to 1 lack diagnostic value [25]. LRs are derived from the Se and Sp values and are independent of the proportion of the disorder in the sample, thereby increasing the likelihood of generalizability to other samples [26]. We checked whether sex altered the proportion with ADHD correctly classified.
Results
Of the 707 children, 126 (18%) were classified with ADHD at 3.5 years of age, 154 (22%) at 5 years, and 78 (11%) at 8 years. Thirty (4%; 19 males) were classified with ADHD at all three time points, 74 (11%) twice, and 120 (17%) only once. Pairwise comparisons showed significant differences between ADHD scores of the groups shown in Fig. 2 (p < 0.001 for all).
Figure 3 shows the percentages of screen positives for the ADHD groups by two-stage CBCL screening at different thresholds.
For both the single- and two-stage screening, the CBCL discriminated the children classified with persistent ADHD from the negative cases significantly better than chance (p < 0.001), both performing excellently (AUCs = 0.90 and 0.94, respectively).
Two-stage screening with a threshold of 6 identified all 30 children within the persistent ADHD group, but also 150 children within the other groups (specifically, 62%, 46%, and 11% of the children classified with ADHD twice, once, and never (Fig. 2)). Increasing the screening threshold to 9 identified half of the children within the persistent ADHD group (n = 15), but also reduced false positives considerably (n = 24), improving PPV (from 0.17 to 0.38) (Table 1).
Table 1 shows the discrimination for each CBCL threshold for single- and two-stage screenings. At a threshold of 6, both single- and two-stage screenings gave perfect sensitivity (100%). However, the two-stage screening lowered the number of false positives by 113 children, and thus increased specificity. When requiring sensitivity values of at least 70%, the single screening with a threshold of 9 gave a high probability of correctly identifying children within the persistent ADHD group (+ LR = 7.29) but missed 9 of the 30 children and identification 65 false positives (PPV = 0.24). Two-stage screening with a threshold of 8 seemed to give the best overall trade-off, with an acceptable sensitivity of 73% (Sp = 94%), loss of eight true positives, and identifying of 41 false positives (PPV = 0.35). In comparison, the PPV at a threshold of 8 from a single screening (3.5 years of age) was 0.19. At this threshold, we also checked the single screen values at 5 years and found similar values to those at 3.5 years (PPV = 0.19). There were only marginal and nonsignificant sex differences in screening accuracies (statistics not shown).
Discussion
In the present study, we showed that even though a considerable proportion of the children were classified with ADHD at least once across time, only a small minority were classified with ADHD at all three time points (ages 3.5, 5, and 8 years), comprising the persistent ADHD group. For population-based studies, having persistent ADHD as an outcome should be a requirement when evaluating screening accuracies in young children because ADHD-like behavior is normal in this developmental period. With persistent ADHD as the outcome, we showed that both screening at 3.5 years of age (single) and at 3.5 and 5 years (two-stage screening) with the CBCL had excellent overall accuracies. However, the two-stage screening was more accurate than single screening at all thresholds, mainly due to a substantial reduction in false-positive rates. This knowledge may be useful to limit unnecessary concern for families and to avoid placing strain on healthcare services.
Nearly 20 years ago, a review underlined that defining the boundaries between normal and clinically significant hyperactivity–impulsivity and inattention is challenging in pre-schoolers as inhibiting behavior and sustaining attention is under development [27]. This may explain the finding that only a small proportion of children in the study sample were persistently classified with ADHD at 3.5, 5, and 8 years of age. Previously, instability of ADHD symptoms from preschool to school age has been found most pronounced in population studies [8, 9, 28,29,30] but also in clinical studies [31,32,33]. One German study reported low-to-moderate ADHD stability during 1 year in kindergarten [30]. Similarly, we previously reported that only 47% (45/97) of the 3 years old classified with ADHD by a diagnostic interview, reached the threshold for ADHD at 8 years of age [9]. Together, these studies support the need to focus on persistent ADHD when evaluating screening tools during preschool. Previous cross-sectional preschool studies have been promising in reporting good psychometric properties of different ADHD screening measures [34,35,36], including acceptable screening accuracies [14, 15, 37,38,39]. The present study used the well-validated and clinically much used CBCL DSM-oriented scale for ADHD [16] in line with one study (n = 616) showing good-to-excellent discriminative capacities of the CBCL to identify ADHD measured with a diagnostic interview between 3 and 5 years of age [40]. However, none of the above-mentioned studies followed the children over time. In addition, a recent meta-analysis of ADHD screening tools concluded that although most have excellent overall diagnostic accuracy, a single measure is unlikely to have sufficient sensitivity and specificity for clinical use or population screening [11]. Assuming that the correct ADHD prevalence rate during preschool years lies between 1.9 and 5.7% [27, 41], these tools will identify an overwhelming number of false-positive children, which could cause strain to many families and be costly to society.
We found that two-stage screening reduced the false-positive rates considerably at all thresholds. This finding was in line with the only previous study using two-stage screening involving teachers to identify ADHD in school children [12]. In clinical practice, it is essential to reach as many at-risk pre-schoolers as possible (highest possible sensitivity) to ameliorate symptoms and improve outcomes, but without unduly raising concern. In the present study, a threshold of 6 in both the single- and two-stage CBCL screening identified all children in the persistent ADHD group (100% Se). However, the two approaches differed in the crude number of false positives and thus in specificity (61% and 78%, respectively). To illustrate, the single screening with a threshold of 6 identified 239 (263—24) more false-positive pre-schoolers than the two-stage screening with a threshold of 9. For most clinics, unnecessary follow-up of many healthy children (with extensive assessments and perhaps treatment) is unacceptable. Repeating the screening at 5 years of age, and raising the thresholds, appears to be the way forward to reduce false positives. This is in line with a review on screening, which pointed out that it would not be costly to refer all children if thresholds are set extremely high, because very few would be identified [10]. However, in the present study, we showed that a single screening with the highest threshold would not be strict enough to avoid several false positives (n = 65), perhaps bringing psychological harm without reason [42]. Depending on resources and on how children are followed up (e.g., interview with parents before school entry), the optimal screening approach in our study was the two-stage screening with a threshold of 8, with the loss of eight at-risk children, and only 41 false positives.
Strengths and limitations
The strengths of the present population-based cohort study were the large sample, the longitudinal design, and the clear definition of a group of children with persistent ADHD with valid and reliable measures [18, 20, 43]. There were also several limitations. Although there were selection biases due to attrition [13], one MoBa-study reporting on ADHD found small differences and assumed limited effects on generalizability [44]. The sampling procedure at 3 years of age, increased the ADHD occurrence rates compared with the general population, possibly inflating the predictive values. There were few children in the persistent group, raising the concern that we may have excluded children with ADHD onset after the age of 3 years. However, our screening procedure at ages 3.5 and 5 years was not designed for detecting such a group with later onset, which would also have required a longer follow-up time to be more certain of stability. Different measures for ADHD at different time points made it impossible to directly compare scores across time, but by calculating z-scores, we were able to follow the children’s deviations from the mean across time points. We only had parent information available in the present study. While a recent review recommends the use of parent-reported measures for screening in young children [11], because we only had clinician assessments of the parent information at 3.5 years of age (PAPA), and otherwise relied on parent questionnaires (from mothers), we may have overestimated the screening accuracies compared with using the outcome of clinically diagnosed ADHD.
Conclusions and future directions
To conclude, this study shows that preschool two-stage screening is more accurate than single screening in identifying children classified with persistent ADHD, mainly by substantially reducing the number of false-positive children. Clinicians who identify pre-schoolers with high symptom scores on ADHD screeners should repeat the screening after some time to see if the symptoms persist before referring children to time-consuming and costly assessments. Future studies should use persistent ADHD as the outcome when estimating the accuracies of ADHD screening tools in young children and should investigate the cost–benefit of such screening. Two-stage screening is recommended to identify pre-schoolers most accurately with ADHD, mainly due to the reduction in the number of false-positive children. This approach may reduce concern for many families and the strain on to healthcare services.
Data availability
The data that support the findings of this study were available from MoBa at the Norwegian Institute of Public Health, but restrictions apply to the availability of these data, used under license for the current study, and so are not publicly available.
References
Oerbeck B, Overgaard KR, Pripp AH, Reichborn-Kjennerud T, Aase H, Zeiner P (2020) Early predictors of ADHD: evidence from a prospective birth cohort. J Atten Disord 24:1685–1692. https://doi.org/10.1177/1087054717696765
Coghill D, Banaschewski T, Cortese S, Asherson P, Brandeis D, Buitelaar J et al (2023) The management of ADHD in children and adolescents: bringing evidence to the clinic: perspective from the European ADHD Guidelines Group (EAGG). Eur Child Adolesc Psychiatry 32:1337–1361. https://doi.org/10.1007/s00787-021-01871-x
Sampaio F, Feldman I, Lavelle TA, Skokauskas N (2022) The cost-effectiveness of treatments for attention deficit-hyperactivity disorder and autism spectrum disorder in children and adolescents: a systematic review. Eur Child Adolesc Psychiatry 31:1655–1670. https://doi.org/10.1007/s00787-021-01748-z
Sciberras E, Streatfeild J, Ceccato T, Pezzullo L, Scott JG, Middeldorp CM et al (2022) Social and economic costs of attention-deficit/hyperactivity disorder across the lifespan. J Atten Disord 26:72–87. https://doi.org/10.1177/1087054720961828
Shephard E, Zuccolo PF, Idrees I, Godoy PBG, Salomone E, Ferrante C et al (2022) Systematic review and meta-analysis: the science of early-life precursors and interventions for attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 61:187–226. https://doi.org/10.1016/j.jaac.2021.03.016
Halperin JM, Marks DJ, Bedard AC, Chacko A, Curchack JT, Yoon CA et al (2013) Training executive, attention, and motor skills: a proof-of-concept study in preschool children with ADHD. J Atten Disord 17:711–721. https://doi.org/10.1177/1087054711435681
Sonuga-Barke EJS, Barton J, Daley D, Hutchings J, Maishman T, Raftery J et al (2018) A comparison of the clinical effectiveness and cost of specialised individually delivered parent training for preschool attention-deficit/hyperactivity disorder and a generic, group-based programme: a multi-centre, randomised controlled trial of the New Forest Parenting Programme versus Incredible Years. Eur Child Adolesc Psychiatry 27:797–809. https://doi.org/10.1007/s00787-017-1054-3
Wootton RE, Riglin L, Blakey R, Agnew-Blais J, Caye A, Cadman T et al (2022) Decline in attention-deficit hyperactivity disorder traits over the life course in the general population: trajectories across five population birth cohorts spanning ages 3 to 45 years. Int J Epidemiol 51:919–930. https://doi.org/10.1093/ije/dyac049
Overgaard KR, Oerbeck B, Friis S, Pripp AH, Aase H, Biele G et al (2022) Attention-deficit/hyperactivity disorder from preschool to school age: change and stability of parent and teacher reports. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-022-02019-1
Sheldrick RC, Garfinkel D (2017) Is a positive developmental-behavioral screening score sufficient to justify referral? a review of evidence and theory. Acad Pediatr 17:464–470. https://doi.org/10.1016/j.acap.2017.01.016
Mulraney M, Arrondo G, Musullulu H, Iturmendi-Sabater I, Cortese S, Westwood SJ et al (2022) Systematic review and meta-analysis: screening tools for attention-deficit/hyperactivity disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry 61:982–996. https://doi.org/10.1016/j.jaac.2021.11.031
Coghill D, Du Y, Jiang W, Xian LuD, Qian Y et al (2022) A novel school-based approach to screening for attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 31:909–917. https://doi.org/10.1007/s00787-021-01721-w
Magnus P, Birke C, Vejrup K, Haugan A, Alsaker E, Daltveit AK et al (2016) Cohort profile update: the Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol 45:382–388. https://doi.org/10.1093/ije/dyw029
Overgaard KR, Oerbeck B, Friis S, Pripp AH, Biele G, Aase H et al (2018) Attention-deficit/hyperactivity disorder in preschoolers: the accuracy of a short screener. J Am Acad Child Adolesc Psychiatry 57:428–435. https://doi.org/10.1016/j.jaac.2018.03.008
Overgaard KR, Oerbeck B, Friis S, Biele G, Pripp AH, Aase H et al (2019) Screening with an ADHD-specific rating scale in preschoolers: a cross-cultural comparison of the early childhood inventory-4. Psychol Assess 31:985–994. https://doi.org/10.1037/pas0000722
Achenbach TM, Rescorla L. Manual for the ASEBA preschool forms & profiles: child behavior checklist for ages 1 1/2–5, language development survey, caregiver - teacher report form : an integrated system of multi-informant assessment. Burlington: ASEBA; 2000. XI, 178 s. p.
Egger HL, Angold AC (2004) The preschool age psychiatric assessment (PAPA): A structured parent interview for diagnosing psychiatric disorders in preschool children. In: DelCarmen-Wiggins R, Carter A (eds) Handbook of infant, toddler, and preschool mental health assessment. Oxford University Press, Oxford, pp 223–243
Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A (2006) Test-retest reliability of the preschool age psychiatric assessment (PAPA). J Am Acad Child Adolesc Psychiatry 45:538–549. https://doi.org/10.1097/01.chi.0000205705.71194.b8
American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. XXXVII, 943 s. p.
Conners CK, Sitarenios G, Parker JD, Epstein JN (1998) The revised conners’ parent rating scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 26:257–268
Kumar G, Steer RA (2003) Factorial validity of the conners’ parent rating scale-revised: short form with psychiatric outpatients. J Pers Assess 80:252–259. https://doi.org/10.1207/S15327752JPA8003_04
Overgaard KR, Oerbeck B, Friis S, Pripp AH, Aase H, Zeiner P (2022) Predictive validity of attention-deficit/hyperactivity disorder from ages 3 to 5 Years. Eur Child Adolesc Psychiatry 31:1–10. https://doi.org/10.1007/s00787-021-01750-5
Gadow KD, Sprafkin J (2000) Early childhood inventory-4: screening manual. Checkmate Plus, Stony Brook, NY
Swets JA (1988) Measuring the accuracy of diagnostic systems. Science 240:1285–1293. https://doi.org/10.1126/science.3287615
McGee S (2002) Simplifying likelihood ratios. J Gen Intern Med 17:646–649. https://doi.org/10.1046/j.1525-1497.2002.10750.x
Youngstrom EA (2014) A primer on receiver operating characteristic analysis and diagnostic efficiency statistics for pediatric psychology: we are ready to ROC. J Pediatr Psychol 39:204–221. https://doi.org/10.1093/jpepsy/jst062
Egger HL, Angold A (2006) Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J Child Psychol Psychiatry 47:313–337. https://doi.org/10.1111/j.1469-7610.2006.01618.x
Finsaas MC, Bufferd SJ, Dougherty LR, Carlson GA, Klein DN (2018) Preschool psychiatric disorders: homotypic and heterotypic continuity through middle childhood and early adolescence. Psychol Med 48:2159–2168. https://doi.org/10.1017/S0033291717003646
Wichstrom L, Belsky J, Steinsbekk S (2017) Homotypic and heterotypic continuity of symptoms of psychiatric disorders from age 4 to 10 years: a dynamic panel model. J Child Psychol Psychiatry 58:1239–1247. https://doi.org/10.1111/jcpp.12754
Schmid G, Wolke D (2014) Preschool regulatory problems and attention-deficit/hyperactivity and cognitive deficits at school age in children born at risk: different phenotypes of dysregulation? Early Hum Dev 90:399–405. https://doi.org/10.1016/j.earlhumdev.2014.05.001
Riddle MA, Yershova K, Lazzaretto D, Paykina N, Yenokyan G, Greenhill L et al (2013) The preschool attention-deficit/hyperactivity disorder treatment study (PATS) 6-year follow-up. J Am Acad Child Adolesc Psychiatry 52(264–78):e2. https://doi.org/10.1016/j.jaac.2012.12.007
Curchack-Lichtin JT, Chacko A, Halperin JM (2014) Changes in ADHD symptom endorsement: preschool to school age. J Abnorm Child Psychol 42:993–1004. https://doi.org/10.1007/s10802-013-9834-9
Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E (2005) Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Arch Gen Psychiatry 62:896–902. https://doi.org/10.1001/archpsyc.62.8.896
McGoey KE, DuPaul GJ, Haley E, Shelton TL (2007) Parent and teacher ratings of attention-deficit/hyperactivity disorder in preschool: the ADHD rating scale-IV preschool version. J Psychopathol Behav Assess 29:269–276. https://doi.org/10.1007/s10862-007-9048-y
Turk S, Harbarth S, Bergold S, Steinmayr R, Neidhardt E, Kamp-Becker I et al (2021) Do German children differ? a validation of conners early childhood. J Atten Disord 25:1441–1454. https://doi.org/10.1177/1087054720907955
Phillips PL, Greenson JN, Collett BR, Gimpel GA (2002) Assessing ADHD symptoms in preschool children: use of the ADHD symptoms rating scale. Early Educ Dev 13:283–300. https://doi.org/10.1207/s15566935eed1303_3
Sveen TH, Berg-Nielsen TS, Lydersen S, Wichstrom L (2013) Detecting psychiatric disorders in preschoolers: screening with the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 52:728–736. https://doi.org/10.1016/j.jaac.2013.04.010
Algorta GP, Dodd AL, Stringaris A, Youngstrom EA (2016) Diagnostic efficiency of the SDQ for parents to identify ADHD in the UK: a ROC analysis. Eur Child Adolesc Psychiatry 25:949–957. https://doi.org/10.1007/s00787-015-0815-0
Hong N, Comer JS (2019) High-end specificity of the attention-deficit/hyperactivity problems scale of the child behavior checklist for ages 1.5-5 in a sample of young children with disruptive behavior disorders. Child Psychiatry Hum Dev 50:222–229. https://doi.org/10.1007/s10578-018-0834-4
de la Osa N, Granero R, Trepat E, Domenech JM, Ezpeleta L (2016) The discriminative capacity of CBCL/1(1/2)-5-DSM5 scales to identify disruptive and internalizing disorders in preschool children. Eur Child Adolesc Psychiatry 25:17–23. https://doi.org/10.1007/s00787-015-0694-4
Wichstrom L, Berg-Nielsen TS, Angold A, Egger HL, Solheim E, Sveen TH (2012) Prevalence of psychiatric disorders in preschoolers. J Child Psychol Psychiatry 53:695–705. https://doi.org/10.1111/j.1469-7610.2011.02514.x
Thomas R, Mitchell GK, Batstra L (2013) Attention-deficit/hyperactivity disorder: are we helping or harming? BMJ 347:6172. https://doi.org/10.1136/bmj.f6172
Sprafkin J, Gadow KD, Salisbury H, Schneider J, Loney J (2002) Further evidence of reliability and validity of the child symptom inventory-4: parent checklist in clinically referred boys. J Clin Child Adolesc Psychol 31:513–524. https://doi.org/10.1207/S15374424JCCP3104_10
Oerbeck B, Overgaard KR, Aspenes ST, Pripp AH, Mordre M, Aase H et al (2017) ADHD, comorbid disorders and psychosocial functioning: how representative is a child cohort study? findings from a national patient registry. BMC Psychiatry 17:23. https://doi.org/10.1186/s12888-017-1204-7
Acknowledgements
We are grateful to all the participating families taking part in this on-going cohort study.
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital). The Norwegian Mother and Child Cohort Study is supported by the Norwegian Ministry of Health and Care Services and the Ministry of Education and Research. The ADHD study is supported by funds and grants from the Norwegian Ministry of Health, the Norwegian Health Directorate, the South Eastern Health Region, G & PJ Sorenson Fund for Scientific Research, and the Norwegian Centre of Expertise for Neurodevelopmental Disorders and Hypersomnias.
Author information
Authors and Affiliations
Contributions
KRO conceptualized and designed the study, acquired the data, drafted the initial manuscript, and critically reviewed and revised the manuscript. BO and GVP interpreted data, critically reviewed, and revised the manuscript. SF performed the main analyses, interpreted data, and critically reviewed and revised the manuscript. AHP, the study statistician, performed the analyses, interpreted data, and critically reviewed the manuscript. GB and CBI interpreted data, and critically reviewed the manuscript. HA and PZ designed the ADHD study, coordinated, and supervised data collection, and critically reviewed the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Polanczyk has served as a consultant/speaker to Abbott, Aché, Medice, Novo Nordisk, and Takeda, and has received royalties from Editora Manole. He receives research support from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) (Grant No. 16/22455–8). All other authors have no conflicts of interest to disclose.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Overgaard, K.R., Oerbeck, B., Friis, S. et al. Early and repeated screening detects children with persistent attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry (2023). https://doi.org/10.1007/s00787-023-02284-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-023-02284-8