Abstract
The present study measured serum levels of vitamin A (VA) and vitamin D (VD) in children with chronic tic disorders (CTD) and investigated their potential association with CTD and comorbidity of attention deficit hyperactivity disorder (ADHD) and the association of their co-insufficiencies or deficiencies with CTD symptoms. A total of 176 children (131 boys and 45 girls, median age of 9 years) with CTD were recruited as the CTD group. During the same period, 154 healthy children were selected as the healthy control (HC) cohort. Circulating retinol and 25-hydroxyvitamin D (25[OH]D) levels were measured for all participants using high-performance liquid chromatography (HPLC) and tandem mass spectrometry. The Yale Global Tic Severity Scale (YGTSS) was employed for the assessment of tic status and CTD impairment. The Swanson, Nolan, and Pelham Rating Scale (SNAP-IV) and the Children’s Yale-Brown Obsessive–Compulsive Scale (CY-BOCS) were used to evaluate comorbidity symptoms. CTD pediatric participants exhibited markedly diminished circulating retinol and 25(OH)D levels compared to HCs. Moreover, VA and VD deficiencies and their co-insufficiencies/deficiencies were more prevalent in CTD participants than HCs. Circulating 25(OH)D levels were inversely proportional to the YGTSS motor tic scores. YGTSS scores in CTD children with only VA or VD insufficiency or deficiency or with VA and VD co-insufficiency/deficiency did not differ from those in CTD children with normal VA and VD. CTD children with comorbid ADHD displayed reduced circulating retinol and 25(OH)D concentrations and elevated prevalence of VD deficiency compared to CTD participants without comorbid ADHD. Lower serum retinol content was intricately linked to the presence of elevated CTD and comorbid ADHD. VA and VD deficiencies and their co-insufficiencies/deficiencies were markedly enhanced in CTD pediatric participants compared to HCs. Lower VA concentration was linked to the presence of enhanced CTD and comorbid ADHD. Therefore, children with CTD, especially with comorbid ADHD, may be at a higher risk of VA or VD deficiency, which may prompt the clinicians to consider whether blood tests for VA and VD in CTD children would be helpful for clinical care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic tic disorders (CTDs) are neurodevelopmental disorders that occur during the early years of human development, with motor and/or vocal tic symptoms for at least 1 year. CTD can be classified into three main categories: chronic motor tic disorder, chronic vocal tic disorder, and Tourette syndrome (TS) [1]. The first two categories do not necessarily include both motor and vocal tics. TS is the most drastic form of CTD, presenting as several motor tics with one or more vocal tics. In children and adolescents, the predicted incidence of CTD is 1–2%, and that of TS is 0.3–0.8%, with a male to female ratio of 3–4:1 [2, 3]. The majority of individuals with CTD (approximately 40–80%) have associated neuropsychiatric comorbidities, of which attention deficit hyperactivity disorder (ADHD) and obsessive–compulsive disorder (OCD) are the most prevalent [4, 5]. Persistent tic symptoms and their comorbidities, especially ADHD, seriously influence the quality of life and socioeconomic ranking of CTD individuals [6,7,8].
The exact etiology of CTD has not yet been fully clarified. Recent studies have suggested that CTD is caused by both polygenetic and environmental agents [9,10,11]. The heritability of CTD is between 0.25 and 0.77 [12, 13]. Susceptibility genes have been associated with several neurotransmitter and neuroimmune systems. Environmental factors, such as dietary composition, potentially pathogen infection, psychosocial stress, exercise, and sleep, may interact with susceptibility genes to increase CTD susceptibility and influence the severity of tic symptoms [14,15,16,17,18].
One environmental factor of interest is micronutrients, such as fat-soluble vitamins A and D. Vitamin D (VD) is a neurosteroid hormone that is mainly synthesized by subcutaneous 7-dehydrocholesterol under sunlight or from vitamin D2 in some foods. In addition to maintaining skeletal health, it plays an important role in neurodevelopment and immune function [19]. VD can regulate the expression of more than 200 genes [20]. Vitamin D receptor (VDR) and its activating enzyme 1α -hydroxylase exist widely in the human brain, and it is speculated to possess neurotrophic and neuroprotective properties, affecting neuroplasticity, neurotransmission, and neuroimmunity [19, 21].
Striatal dopaminergic dysregulation is regarded as a commonly discussed possible mechanism of CTD pathophysiology [22]. Pathophysiological study showed that the impaired cortico-basal ganglia network, whereby dopaminergic input from the substantia nigra pars compacta regulates function across the basal ganglia, is strongly correlated with CTD pathogenesis [23]. VD protects the dopamine system via gene expression regulation [24, 25], and it also modulates relevant enzymes: tyrosine hydroxylase and catechol aminotransferase, which are the rate-limiting enzymes for dopamine, norepinephrine, and adrenaline syntheses [26]. Hence, VD deficiency can result in dopaminergic dysregulation within CTD participants. Additionally, VD is closely related to brain development [19], and abnormal brain structure and maturation are also considered parts of the pathogenesis of CTD [27]. Therefore, VD deficiency might be related to the pathogenesis of CTD.
Vitamin A (VA) is also a crucial micronutrient, and its active form, retinoic acid (RA), is intricately involved in central nervous system-based cellular development and differentiation. Animal investigations have revealed that VA deficiency impairs synaptic plasticity in the hippocampus, which is modulated by retinoic acid nuclear receptor-α [28]. Moreover, VA and VD synergistically regulate gene expression [29]. VD and retinoic acid interact with VDR and retinoic acid receptor (RXR) complex in the nucleus for further gene regulation [30]. Therefore, VA deficiency might contribute to CTD pathogenesis.
Our previous studies demonstrated an association between VD deficiency and CTD [31, 32]. Recently, a large case–control study (n = 2960) in China reported reduced concentrations of 25-hydroxyvitamin D (25[OH]D) in children with tics versus healthy controls, but no association was observed between these levels and the degree of tic [33]. A multicenter study revealed no obvious differences between VD concentrations and an elevated prevalence or degree of tics; however, the study found that VD levels were intricately linked to the prevalence and degree of comorbid ADHD in children and adolescents with CTD [34]. Considering the mechanistic synergy of VA and VD and their possible association with neuropsychiatric disorders, our previous study also found a correlation between VA and VD levels with ADHD [35], although it did not explore the relationship between VA and CTD. To date, only one study (n = 59) has reported the relationship between VA levels and tics and found that VA deficiency was associated with tics in children [36].
Based on the inconsistencies of the above-mentioned results, those findings require further study. Here, we assessed VA and VD levels in CTD children aged 5–12 years and delineated their correlations with CTD symptoms and ADHD comorbidity.
Methods
Participants and procedures
From May 2017 to June 2020, we selected 176 CTD children aged 5–12 years who were evaluated for the first time in the Outpatient Department of the First Hospital of Jilin University. Initially, all children suspected of having CTD were examined by reviewing their current health, developmental and family history, along with a thorough physical evaluation and parental interviews by a developmental pediatrician referencing the CTD criteria based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [1]. A total of 176 children fulfilled the diagnostic criteria for CTD, including 131 boys and 45 girls, with a median age of 9 years (range: 5–12 years). During the same period, 154 healthy children without any somatic and behavioral abnormalities were recruited into the healthy control (HC) group from the same outpatient department, including 109 boys and 45 girls, with a median age of 9 years (range: 6–12 years). These participants did not present any signs of neurodevelopmental or other disorders that may influence micronutrient homeostasis.
Exclusion criteria comprised (1) children suffering from other neurological or neurodevelopmental disorders, such as neurodegenerative disorders, autism, epilepsy, and intellectual disorders; (2) children with severe picky eating, malnutrition, digestive diseases, etc., that may affect micronutrient absorption and metabolism; (3) children who had received VA, VD, or multivitamin supplements in the past 3 months; (4) abnormal liver and kidney function, or taking glucocorticoids, benzodiazepines, and other medication that may influence VA and VD metabolism. This study used a case–control design. The parents or guardians of the children signed documented informed consent before the initiation of the study. This work received ethical approval and registry from the First Hospital of Jilin University and the Chinese Clinical Trial Registry (registration number: CHICTR-OPC-17013502), respectively. The authors of the present study previously published results involving 46 cases, with 42 healthy controls enrolled in this study [31].
Initial clinical assessment
The parents or caregivers of all participants completed a survey developed by our research team regarding demographic characteristics, including sex, age, place of residence, sun exposure, physical activity, daily diets, and vitamin supplementation. An electronic scale and stadiometer were used to measure the children’s height and weight. Body mass index (BMI) was computed as follows: \(\mathrm{BMI }=\mathrm{ weight }(\mathrm{kg})/(\mathrm{height }(\mathrm{m})2\). Based on the age percentile of BMI, we divided the participants into three categories: normal weight (< 85th percentile), overweight (85–95th percentile), or obese (> 95th percentile) [37].
Behavioral assessments
The Yale Global Tic Severity Scale (YGTSS) was employed for tic degree assessment and impairment in children in the CTD group. The YGTSS is a semi-structured scale assigning scores based on frequency, intensity, quantity, interference, and complexity of tics [38]. The sum tic score includes motor and vocal tic scores, with a range from 0 to 50 points. The YGTSS impairment ranking subscale is designed to assess functional impairments related to tics, such as psychological and self-esteem impairment, with scores between 0 and 50 points. The total score of YGTSS is the sum of the total tic scores and the impairment rating subscale scores. The Chinese version of YGTSS with good psychometric properties was utilized in this study [39]. Additionally, the parent and teacher versions of the Swanson, Nolan, and Pelham Rating Scale (SNAP-IV) were employed to evaluate the presence of comorbid ADHD [40]. The Children’s Yale–Brown Obsessive–Compulsive Scale (CY-BOCS) evaluated the OCD symptoms [41]. A self-made behavior questionnaire was used to screen for anxiety, depression, and other emotional problems. Those who scored positive (meeting the symptom criteria for ADHD or OCD) on the SNAP-IV or CY-BOCS would be confirmed by the developmental pediatrician according to the criteria for ADHD and OCD in the DSM-5 to make the final diagnosis of whether the patient is comorbid with ADHD or OCD.
Laboratory measurements
After enrollment, CTD participants underwent a routine blood test, which included blood cell count, rheumatoid factor, anti-O antibody, liver and kidney function, serum calcium level, and zinc, iron, copper, and magnesium levels. Serum retinol and 25(OH)D content of both groups were measured at baseline by high-performance liquid chromatography and tandem mass spectrometry (HPLC-MS/MS) in Jilin Hehe Medical Center (Clinical Laboratory). Circulating retinol levels of > 1.05, 0.7–1.05, and < 0.7 μmol/L were judged as “normal VA”, “marginal VA”, and “VA deficiency”, respectively [42]. Serum 25(OH)D concentrations of 30–90, 21–29, and < 20 ng/mL were judged as “optimal VD”, “VD insufficiency” and “VD deficiency” respectively [43]. In the present study, we have defined the VA deficiency by a retinol level < 0.7 μmol/L and VA insufficiency 0.7–1.05 μmol/L. Similarly, we defined the VD deficiency by a 25(OH)D level < 20 ng/mL and VD insufficiency 21–29 ng/mL.
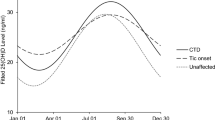
In the United States, Boston (MA) has the same latitude as Changchun, which is between 42° and 45° of North latitude. Thus, Summer (June–October) and winter seasons (November–May) were used for the division of the year in the present study, adopting the results presented by the Boston study [44] regarding the association between the seasonal variation of sunlight and serum 25(OH)D content.
Statistical analysis
All data were analysed by SPSS V23.0 statistical software. The Kolmogorov–Smirnov test was employed for the normality assessment of continuous variables. Continuous information was represented by P50 (P25, P75). Categorical data were expressed as frequencies with percentages. Using the nonparametric Mann–Whitney U test, the continuous or ordered categorical variables of both groups were compared. A chi-squared test was utilized to assess differences in the amount of unordered categorical variables of both groups. The Kruskal–Wallis H test was used to compare the differences in the total and subscale scores of YGTSS among the four groups, and the Mann–Whitney U test was further used to conduct a post-hoc test between the two groups. Spearman’s correlation coefficient was employed to examine the correlation between YGTSS total scores and subscale scores and serum retinol and 25(OH)D concentrations. Multivariate logistic regression analysis was employed to determine the association between circulating retinol and 25(OH)D concentrations and the presence of CTD and ADHD comorbidity. The odds ratio (OR) was reported in the result. The significance threshold was set to P of < 0.05, with two-sided tests for all analyses.
Results
Comparing the sociodemographic characteristics between CTD and HC participants
The present study enrolled 176 children with CTD. Eighty-one participants presented with a chronic motor tic disorder, 14 participants presented with a chronic vocal tic disorder, and 81 participants presented with TS. Seventy children were comorbid with ADHD, six children were comorbid with OCD, and 13 had anxiety symptoms.
Table 1 provides a detailed breakdown of sociodemographic data for these two groups. No discernible differences were observed between CTD and HC children in sex, age, BMI, parents’ education level, resident area, the season of blood collection, annual household income, and daily exposure to sunlight. Compared with HCs, the proportion of CTD children with a dairy intake of > 300 mL was significantly reduced.
Serum retinol and 25(OH)D levels in the CTD and HC participants
Table 2 exhibits the status of serum retinol and 25(OH)D in both groups. The median circulating concentration of retinol and 25(OH)D in CTD participants was markedly diminished compared to HCs. CTD participants were more likely than healthy control participants to be retinol marginal or deficient. Compared to HC participants, remarkably more CTD participants had 25(OH)D deficiency and serum retinol and 25(OH)D co-insufficiency/deficiency.
Association between circulating VA and VD levels with YGTSS scores
The association coefficients of circulating retinol and 25(OH)D with the sum YGTSS and subscale scores are provided in Table 3. The circulating 25(OH)D level was significantly and negatively associated with the motor score. No obvious correlation was observed between serum retinol level and YGTSS total score and subscale score.
Relationships between VA and VD co-insufficiency/deficiency and YGTSS scores
Among CTD participants, 69 (39%) exhibited VA and VD co-insufficiency/deficiency, 13 cases (7%) exhibited VA insufficiency or deficiency only, 76 cases (43%) exhibited VD insufficiency or deficiency only, and 18 cases (10%) exhibited normal VA and VD.
Marked differences were observed in the total tic and motor scores in YGTSS between the VA and VD co-insufficiency/deficiency, VA insufficiency or deficiency only, VD insufficiency or deficiency only, and VA and VD normal participants. The total tic score of VA and VD co-insufficiency/deficiency participants were markedly elevated compared to the VA insufficiency or deficiency only (Z = − 2.28, P = 0.02) and VD insufficiency or deficiency only participants (Z = − 3.04, P = 0.002). The motor score of VA and VD co-insufficiency/deficiency participants were markedly elevated compared to the VA insufficiency or deficiency only participants (Z = − 2.44, P = 0.015). However, there was no significant difference in the total tic and motor scores between the VA and VD co-insufficiency/deficiency group and the VA and VD normal group. Although the total tic and vocal scores in the VA insufficiency or deficiency only and VD insufficiency or deficiency only participants were lower than those in the VA and VD normal participants, these did not reach significance (Table 4).
Serum retinol and 25(OH)D levels in CTD-comorbid ADHD and CTD without comorbidity participants
In the CTD group, 70 children had ADHD comorbidity, 19 cases had anxiety and obsessive–compulsive symptoms, and the remaining 87 cases had no comorbidities.
Table 5 shows the serum VA and VD contents in CTD participants without comorbidity and children with comorbid ADHD. Median serum concentrations of retinol and 25(OH)D in the co-ADHD group were markedly diminished compared to CTD participants without comorbidity. The proportion of children with 25(OH)D deficiency in co-ADHD participants was markedly increased compared to non-comorbidity participants, and the proportion of children with optimal 25(OH)D in co-ADHD participants was drastically reduced compared to non-comorbidity participants. No obvious difference was seen in the proportion of circulating retinol normal and marginal levels and deficiency between the two groups.
Correlations between circulating VA and VD contents and CTD presence
Based on the multivariate analysis, circulating retinol concentration (adjusted OR 0.19; 95% confidence interval, 0.07–0.53; P = 0.002) and daily dairy intake (> 300 mL) (0.46; 0.27–0.79; 0.004) were significantly negatively correlated with the presence of CTD after adjusting for BMI and sunshine exposure (Table 6).
Correlations between circulating VA and VD contents and ADHD comorbidity presence
Based on the multivariate analysis, circulating retinol content (adjusted OR 0.11; 95% confidence interval, 0.02–0.71; P = 0.02) was significantly negatively correlated with the presence of ADHD comorbidity, and age (3.31; 2.09–5.25; < 0.001) was significantly positively correlated with the presence of ADHD comorbidity after adjusting for BMI, daily dairy product intake, and daily sunlight exposure (Table 7).
Discussion
This research presents four major findings. First, serum VA and VD contents in CTD participants were drastically reduced compared to HCs, and VA and VD deficiency and their co-insufficiency/deficiency prevalence was markedly elevated compared to HCs. Second, YGTSS scores in CTD children with only VA or VD insufficiency/deficiency or with VA and VD co-insufficiency/deficiency did not differ from those in CTD children with normal VA and VD. Third, CTD participants with comorbid ADHD had lower serum VA and VD contents and higher VD deficiency prevalence compared with CTD participants without comorbid ADHD. Fourth, lower serum VA contents were correlated with the presence of enhanced CTD and comorbid ADHD.
Our results found lower levels of VD and higher prevalence of VD deficiency in children with CTD, and the serum VD levels were negatively correlated with tic symptoms. These findings are consistent with our previous research [31, 32]. Recently, a large sample case–control study in China has also shown that serum VD levels of participants with tic disorders were drastically reduced compared to HC, and VD deficiency prevalence was markedly increased. However, no correlation was found between serum VD levels and tic symptoms [33]. The possible reasons for the inconsistent results compared to the current study are as follows: differences in sample size, geographical location of the population, and the classification of tic disorders. A key limitation of Wang et al. [33], as noted by the authors themselves, was that they did not analyze the possible effects of different types of tic disorders and comorbidities on VD levels. In contrast to our results, Bond et al. found that higher serum VD levels increased the risk of CTD presence and did not correlate with tic severity [34]. The present study found a negative correlation between serum VD levels and motor tic scores. These different findings may be related to ethnicity and genetic susceptibility. Another possible reason for the difference is that the control group of Bond et al. was a group of individuals who did not develop tics during up to 7 years of follow-up [34]. Diet, vitamin D supplementation, and outdoor activities during follow-up may influence the final outcome-tic onset. One limitation of the study of Bond et al. as mentioned by the authors themselves, was the lack of data on vitamin D supplementation and sun exposure [34]. In addition, the age range of the study population was 5–12 years old in the present study and 3–16 years old in the study conducted by Bond et al. [34]. Different nutrition, diets, and outdoor exercise at different ages may affect VD status. This suggests that future global multicenter studies should be conducted to elucidate the relationship between VD and CTD.
The mechanism of lower VD levels in children with CTD is unclear. VD is a neurosteroid hormone produced mainly by ultraviolet B (UVB) radiation to the skin and is also naturally found in some foods. Its formation was found to be modulated by season, latitude, air pollution, skin pigment, diet, and certain drugs that may affect the absorption or metabolism of VD [21]. The study also found that the daily intake of dairy products in children with CTD was significantly lower than that of HCs, which might indicate that CTD children might have abnormal diet structure. For example, children who are picky eaters may not like drinking dairy products, resulting in an insufficient intake of VD food sources (as dairy products in China usually contain VD). Therefore, decreased dairy intake is a possible influencing factor for lower VD levels in children with CTD. However, since the present study does not conduct a detailed investigation of dietary behavior problems among the participants, the relationship between dairy intake and VD levels needs to be further studied.
Although the current study could not establish a causal relationship between lower VD levels and CTD pathogenesis, it did suggest that VD was associated with CTD to some extent. VD is essential for the normal development of dopaminergic neurons. Cortico-basal ganglia circuit dopamine dysfunction is considered as a commonly discussed possible mechanism of CTD pathophysiology [22]. In vitro and in vivo studies have found that VD could regulate the genetic profile of dopamine rate-limiting enzyme–tyrosine hydroxylase [26, 45]. Moreover, VD modulates the levels of glial cell line neurotrophic factor (GDNF) and GDNF receptor C-Ret, which are essential for the survival and differentiation of dopaminergic neurons [46]. Therefore, as one of the environmental factors, VD deficiency might increase the genetic susceptibility to CTD during the critical period of brain development, thereby increasing the risk of CTD onset. Neuroinflammation caused by the immune mechanism is also believed to be involved in the pathophysiological process of CTD [47]. VD plays an anti-inflammatory role by regulating cellular and humoral immune responses, and levels of VD have been associated with elevated inflammatory markers in CTD participants [21, 47]. VD deficiency potentially affect the severity of neuroinflammation. A small sample of VD supplementation (n = 36) in our previous study has also suggested that VD supplementation was effective in improving tic symptoms and further indicated that lower levels of VD might contribute to CTD pathogenesis [31].
In this study, CTD participants had lower circulating retinol concentrations and a higher prevalence of VA insufficiency or deficiency (approximately 46%) compared to HCs. To date, only one case–control investigation [36] has reported the correlation between circulating VA concentration and TD in children. The study’s results showed that serum VA content in TD participants was markedly reduced compared to HCs, and lower VA level was associated with increased tic symptoms [36]. In contrast, our study found no association between circulating VA levels and symptoms in CTD participants. This difference might be related to different populations that were included. There were 59 cases in the observation group of the above-mentioned study, among which only 34 cases were CTD children.
RA, an active derivative of VA, is involved in cell differentiation, antioxidant activity, inflammation, and neuronal plasticity and critically modulates normal activities of the central nervous system. Many studies have demonstrated striatal dopaminergic dysfunction and striatal microstructural abnormalities in CTD participants [22, 48]. RA can affect the dopamine signaling pathway and its plasticity by regulating gene transcription [49, 50]. RA receptors are widely available in striatal neurons [51]. RA signaling also modulates neurogenesis and striatal neuron differentiation [52,53,54]. Animal investigations have shown that VA supplementation improved voluntary movements in 6-hydroxydopamine (6-OHDA) lesioned rats by increasing D2 and RXR receptor expressions within the striatum [55]. RA therapy alleviates L-DOPA-induced dyskinesia movements in mice by upregulating striatal MOR1 levels and signaling [52]. These symptoms are partly similar to tics. In addition, RA and its mediated signaling pathway are related to intestinal inflammation [56], and the changes in the RA pathway may be related to intestinal immune inflammation and microbial homeostasis imbalance [57, 58]. Particular gut microbiota changes could be observed in children with TS [59]. Fecal transplantation can alleviate tic severity in a TS mouse model [60], and the RA signaling pathway might play a mediating role in this process. Therefore, we speculate that VA may be involved in the pathophysiological mechanism of CTD.
The present study found that lower serum VD levels were associated with higher motor tic scores. Considering the synergistic effect of VA and VD in the nucleus (RA and VD must interact with the RXR and VDR complex to exert gene regulation) [30, 61], we explored the relationship between VA and VD co-insufficiency/deficiency and tic symptoms. However, contrary to our hypothesis, the subgroup analysis showed no difference in YGTSS scores among CTD children with only VA or VD insufficiency/deficiency or with VA and VD co-insufficiency/deficiency compared to CTD children with normal VA and VD. Conversely, CTD children with only VA or VD insufficiency/deficiency appear to have lower total tic and vocal tic scores than CTD children with normal VA and VD, although these did not reach significance. In summary, the present results suggest that VA or VD only insufficiency/deficiency or VA and VD co-insufficiency/deficiency are not associated with tic symptoms. Tic symptoms and their fluctuation are affected by sex, age, dietary factors, and exercise. However, due to the limitation of the sample size, we failed to match the four groups with sex, age, daily dairy intake, and daily exposure to sunlight. Therefore, future studies should expand the sample size and control for these factors to further explore the relationship between VA and VD co-insufficiency/deficiency and tic symptoms.
For comorbid ADHD in children with CTD, we found lower serum VA and VD levels and a higher prevalence of VD deficiency compared with that of non-ADHD comorbidity. ADHD is a common comorbidity of CTD, and the prevalence of comorbid ADHD in children with CTD is 40–80% [62]. Two recent meta-analyses, as well as one of our previous studies, have also found a reduced concentration of 25(OH)D in ADHD participants compared to HCs [35, 63, 64]. However, limited investigations have evaluated the role of 25(OH)D within the context of comorbid ADHD in CTD participants. Thus far, only one study has explored the relationship between VD and ADHD comorbidity in children with CTD and found that lower VD levels were linked to the presence and degree of comorbid ADHD in CTD participants [34]. Although our study found that the CTD comorbid with ADHD group had lower VD levels and a higher prevalence of VD deficiency, we observed no discernible association between lower VD contents and the presence of comorbid with ADHD in CTD children, which may be related to racial differences and dietary structure, needing to be further explored.
We assessed, for the first time, the relationship between VA and comorbidity of ADHD in CTD children and found that lower VA contents were correlated with the presence of CTD and ADHD comorbidity. Evidence of the genetic, neurophysiological, and neurobiological overlap between CTD and ADHD suggests that the two disorders are intricately intercorrelated [62]. Children with both CTD and ADHD have a greater functional impairment and lower quality of life [65]. Overall, we found that children with CTD had a higher risk of VA and VD deficiencies in our sample, which may prompt the clinicians to consider whether blood tests for VA and VD in children with tics would be helpful.
Although our investigation was based on a case–control design, and we matched the sex, age, blood collection time, BMI, and socioeconomic status of the two groups to circumvent the impact of confounding factors on VA and VD contents, there were still some limitations. First, VA is obtained mainly from food. Therefore, dietary behavior has a larger influence on participants’ VA content, and children with CTD may be more picky or partial eaters, thus, affecting the circulating VA level. However, we did not conduct a detailed investigation of eating behavior problems in the participants, nor did we analyze the possible influence of these factors on vitamin levels. Second, the daily intake of dairy products was not matched between the two groups, and the number of CTD children was significantly lower than HCs, which may also have led to biased results. The third limitation is that our cross-sectional study could only conclude that VA and VD levels were correlated with CTD and its comorbidities with ADHD—it could not infer a causal relationship between VA or VD deficiency and the presence of CTD and its comorbidities with ADHD. Prospective longitudinal investigations are warranted to establish whether reduced VA and VD contents predispose CTD to persistence or comorbidity of ADHD.
Conclusion
VA and VD deficiencies and their co-insufficiencies/deficiencies in CTD participants were markedly increased compared to HCs. Lower VA concentrations were linked to the increased presence of CTD and comorbid ADHD. Thus, CTD children, particularly those with comorbid ADHD, may be at a higher risk of VA or VD deficiency, which may prompt the clinicians to consider whether blood tests for VA and VD in CTD children would be helpful for clinical care. However, VA and VD mechanisms in CTD require further investigation.
Data availability
The datasets used and analysed during the current study are included in the supplementary material, further inquiries can be directed to the corresponding author.
Abbreviations
- VA:
-
Vitamin A
- VD:
-
Vitamin D
- CTD:
-
Chronic Tic Disorders
- ADHD:
-
Attention Deficit Hyperactivity Disorder
- HC:
-
Healthy Control
- 25[OH]D:
-
25-Hydroxyvitamin D
- HPLC:
-
High-performance Liquid Chromatography
- YGTSS:
-
Yale Global Tic Severity Scale
- SNAP-IV:
-
Swanson, Nolan, and Pelham Rating Scale
- CY-BOCS:
-
Children’s Yale-Brown Obsessive–Compulsive Scale
- TS:
-
Tourette Syndrome
- OCD:
-
Obsessive–compulsive Disorder
- VDR:
-
Vitamin D Receptor
- RA:
-
Retinoic acid
- RXR:
-
Retinoic Acid Receptor
- DSM-5:
-
Diagnostic and Statistical Manual of Mental Disorders
- BMI:
-
Body Mass Index
- 6-OHDA:
-
6-Hydroxydopamine
References
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edn. American Psychiatric Association, Washington, DC
Knight T, Steeves T, Day L, Lowerison M, Jette N, Pringsheim T (2012) Prevalence of tic disorders: a systematic review and meta-analysis. Pediatr Neurol 47:77–90. https://doi.org/10.1016/j.pediatrneurol.2012.05.002
Yang C, Zhang L, Zhu P, Zhu C, Guo Q (2016) The prevalence of tic disorders for children in China: a systematic review and meta-analysis. Medicine 95:e4354. https://doi.org/10.1097/md.0000000000004354
Hirschtritt ME, Lee PC, Pauls DL, Dion Y, Grados MA, Illmann C, King RA, Sandor P, McMahon WM, Lyon GJ et al (2015) Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiat 72:325–333. https://doi.org/10.1001/jamapsychiatry.2014.2650
Lebowitz ER, Motlagh MG, Katsovich L, King RA, Lombroso PJ, Grantz H, Lin H, Bentley MJ, Gilbert DL, Singer HS et al (2012) Tourette syndrome in youth with and without obsessive compulsive disorder and attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 21:451–457. https://doi.org/10.1007/s00787-012-0278-5
Aldred M, Cavanna AE (2015) Tourette syndrome and socioeconomic status. Neurol Sci 36:1643–1649. https://doi.org/10.1007/s10072-015-2223-0
Eapen V, Snedden C, Črnčec R, Pick A, Sachdev P (2016) Tourette syndrome, co-morbidities and quality of life. Aust N Z J Psychiatry 50:82–93. https://doi.org/10.1177/0004867415594429
Silvestri PR, Chiarotti F, Baglioni V, Neri V, Cardona F, Cavanna AE (2016) Health-related quality of life in patients with Gilles de la Tourette syndrome at the transition between adolescence and adulthood. Neurol Sci 37:1857–1860. https://doi.org/10.1007/s10072-016-2682-y
Wendt FR, Pathak GA, Tylee DS, Goswami A, Polimanti R (2020) Heterogeneity and polygenicity in psychiatric disorders: a genome-wide perspective. Chronic Stress (Thousand Oaks, Calif) 4:2470547020924844. https://doi.org/10.1177/2470547020924844
Abdulkadir M, Mathews CA, Scharf JM, Yu D, Tischfield JA, Heiman GA, Hoekstra PJ, Dietrich A (2019) Polygenic Risk scores derived from a Tourette syndrome genome-wide association study predict presence of tics in the Avon longitudinal study of parents and children cohort. Biol Psychiat 85:298–304. https://doi.org/10.1016/j.biopsych.2018.09.011
Yu D, Sul JH, Tsetsos F, Nawaz MS, Huang AY, Zelaya I, Illmann C, Osiecki L, Darrow SM, Hirschtritt ME et al (2019) Interrogating the genetic determinants of Tourette's syndrome and other Tic disorders through genome-wideassociation studies. Am J Psychiat 176:217–227. https://doi.org/10.1176/appi.ajp.2018.18070857
Mataix-Cols D, Isomura K, Pérez-Vigil A, Chang Z, Rück C, Larsson KJ, Leckman JF, Serlachius E, Larsson H, Lichtenstein P (2015) Familial risks of tourette syndrome and chronic Tic disorders. A population-based cohort study. JAMA Psychiatry 72:787–793. https://doi.org/10.1001/jamapsychiatry.2015.0627
Zilhão NR, Olthof MC, Smit DJ, Cath DC, Ligthart L, Mathews CA, Delucchi K, Boomsma DI, Dolan CV (2017) Heritability of tic disorders: a twin-family study. Psychol Med 47:1085–1096. https://doi.org/10.1017/s0033291716002981
Kim DD, Warburton DER, Wu N, Barr AM, Honer WG, Procyshyn RM (2018) Effects of physical activity on the symptoms of Tourette syndrome: a systematic review. Eur Psychiatry 48:13–19. https://doi.org/10.1016/j.eurpsy.2017.11.002
Rizzo R, Prato A, Scerbo M, Saia F, Barone R, Curatolo P (2022) Use of nutritional supplements based on L-theanine and vitamin B6 in children with tourette syndrome, with anxiety disorders: a pilot study. Nutrients. https://doi.org/10.3390/nu14040852
Isomura K, Sidorchuk A, Sevilla-Cermeño L, Åkerstedt T, Silverberg-Morse M, Larsson H, Mataix-Cols D, Fernández de la Cruz L (2022) Insomnia in tourette syndrome and chronic Tic disorder. Mov Disord 37:392–400. https://doi.org/10.1002/mds.28842
Schnell J, Bond M, Moll N, Weidinger E, Burger B, Bond R, Dietrich A, Hoekstra PJ, Schrag A, Martino D et al (2022) Mycoplasma pneumoniae IgG positivity is associated with tic severity in chronic tic disorders. Brain Behav Immun 99:281–288. https://doi.org/10.1016/j.bbi.2021.10.012
Leisman G, Sheldon D (2022) Tics and emotions. Brain Sci. https://doi.org/10.3390/brainsci12020242
Eyles DW, Burne TH, McGrath JJ (2013) Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front Neuroendocrinol 34:47–64. https://doi.org/10.1016/j.yfrne.2012.07.001
Cannell JJ, Grant WB (2013) What is the role of vitamin D in autism? Dermato-endocrinology 5:199–204. https://doi.org/10.4161/derm.24356
Kočovská E, Gaughran F, Krivoy A, Meier UC (2017) Vitamin-D deficiency as a potential environmental risk factor in multiple sclerosis, schizophrenia, and autism. Front Psych 8:47. https://doi.org/10.3389/fpsyt.2017.00047
Leckman JF, Bloch MH, Smith ME, Larabi D, Hampson M (2010) Neurobiological substrates of Tourette’s disorder. J Child Adolesc Psychopharmacol 20:237–247. https://doi.org/10.1089/cap.2009.0118
Yael D, Vinner E, Bar-Gad I (2015) Pathophysiology of tic disorders. Mov Disord 30:1171–1178. https://doi.org/10.1002/mds.26304
Pertile RA, Cui X, Eyles DW (2016) Vitamin D signaling and the differentiation of developing dopamine systems. Neuroscience 333:193–203. https://doi.org/10.1016/j.neuroscience.2016.07.020
Liu Y, Li YW, Tang YL, Liu X, Jiang JH, Li QG, Yuan JY (2013) Vitamin D: preventive and therapeutic potential in Parkinson’s disease. Curr Drug Metab 14:989–993. https://doi.org/10.2174/1389200211314090005
Cui X, Pertile R, Liu P, Eyles DW (2015) Vitamin D regulates tyrosine hydroxylase expression: N-cadherin a possible mediator. Neuroscience 304:90–100. https://doi.org/10.1016/j.neuroscience.2015.07.048
Greene DJ, Williams Iii AC, Koller JM, Schlaggar BL, Black KJ (2017) Brain structure in pediatric Tourette syndrome. Mol Psychiatry 22:972–980. https://doi.org/10.1038/mp.2016.194
Hou N, Ren L, Gong M, Bi Y, Gu Y, Dong Z, Liu Y, Chen J, Li T (2015) Vitamin A deficiency impairs spatial learning and memory: the mechanism of abnormal CBP-dependent histone acetylation regulated by retinoic acid receptor alpha. Mol Neurobiol 51:633–647. https://doi.org/10.1007/s12035-014-8741-6
Parastouei K, Mirshafiey A, Eshraghian MR, Shiri-Shahsavar MR, Solaymani-Mohammadi F, Chahardoli R, Alvandi E, Saboor-Yaraghi AA (2018) The effect of 1, 25(OH)2 D3 (calcitriol) alone and in combination with all-trans retinoic acid on ROR-γt, IL-17, TGF-β, and FOXP3 gene expression in experimental autoimmune encephalomyelitis. Nutr Neurosci 21:210–218. https://doi.org/10.1080/1028415x.2016.1263039
Chesney RW, Han X (2013) Differential regulation of TauT by calcitriol and retinoic acid via VDR/RXR in LLC-PK1 and MCF-7 cells. Adv Exp Med Biol 776:291–305. https://doi.org/10.1007/978-1-4614-6093-0_27
Li HH, Xu ZD, Wang B, Feng JY, Dong HY, Jia FY (2019) Clinical improvement following vitamin D3 supplementation in children with chronic tic disorders. Neuropsychiatr Dis Treat 15:2443–2450. https://doi.org/10.2147/ndt.S212322
Li HH, Shan L, Wang B, Du L, Xu ZD, Jia FY (2018) Serum 25-hyroxyvitamin D levels and tic severity in Chinese children with tic disorders. Psychiatry Res 267:80–84. https://doi.org/10.1016/j.psychres.2018.05.066
Wang S, Xu Q, Wang A, Yuan F, Luo X, Wang Y, Guo M, Zhang Y, Zhang W, Ji X et al (2022) Correlation between Tic disorders and serum 25-hydroxyvitamin D levels in Chinese children. Front Pediatr 10:833371. https://doi.org/10.3389/fped.2022.833371
Bond M, Moll N, Rosello A, Bond R, Schnell J, Burger B, Hoekstra PJ, Dietrich A, Schrag A, Kocovska E et al (2021) Vitamin D levels in children and adolescents with chronic tic disorders: a multicentre study. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-021-01757-y
Li HH, Yue XJ, Wang CX, Feng JY, Wang B, Jia FY (2020) Serum levels of vitamin A and vitamin D and their association with symptoms in children with attention deficit hyperactivity disorder. Front Psychiatry 11:599958. https://doi.org/10.3389/fpsyt.2020.599958
Wang H, Yang Y, Zhou D, Bai C, Shi M (2022) Correlation between serum levels of vitamin A and vitamin D with disease severity in tic disorder children. Evid Based complement Altern Med 2022:7121900. https://doi.org/10.1155/2022/7121900
Li H, Zong XN, Ji CY, Mi J (2010) Body mass index cut-offs for overweight and obesity in Chinese children and adolescents aged 2–18 years. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi 31:616–620
Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J, Cohen DJ (1989) The yale global tic severity scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 28:566–573. https://doi.org/10.1097/00004583-198907000-00015
Wen F, Gu Y, Yan J, Liu J, Wang F, Yu L, Li Y, Cui Y (2021) Revisiting the structure of the Yale Global Tic Severity Scale (YGTSS) in a sample of Chinese children with tic disorders. BMC Psychiatry 21:394. https://doi.org/10.1186/s12888-021-03399-5
Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL et al (2001) Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 40:168–179. https://doi.org/10.1097/00004583-200102000-00011
Yan J, Gu Y, Wang M, Cui Y, Li Y (2022) The obsessive-compulsive symptoms in tic disorders and the psychometric properties of children’s yale-brown obsessive-compulsive scale: an evidence-based survey in a Chinese sample. Front Pediatr 10:794188. https://doi.org/10.3389/fped.2022.794188
Chen K, Li TY, Chen L, Qu P, Liu YX (2008) Effects of vitamin A, vitamin A plus iron and multiple micronutrient-fortified seasoning powder on preschool children in a suburb of Chongqing, China. J Nutr Sci Vitaminol 54:440–447. https://doi.org/10.3177/jnsv.54.440
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930. https://doi.org/10.1210/jc.2011-0385
Webb AR, Pilbeam C, Hanafin N, Holick MF (1990) An evaluation of the relative contributions of exposure to sunlight and of diet to the circulating concentrations of 25-hydroxyvitamin D in an elderly nursing home population in Boston. Am J Clin Nutr 51:1075–1081. https://doi.org/10.1093/ajcn/51.6.1075
Hawes JE, Tesic D, Whitehouse AJ, Zosky GR, Smith JT, Wyrwoll CS (2015) Maternal vitamin D deficiency alters fetal brain development in the BALB/c mouse. Behav Brain Res 286:192–200. https://doi.org/10.1016/j.bbr.2015.03.008
Pertile RAN, Cui X, Hammond L, Eyles DW (2018) Vitamin D regulation of GDNF/Ret signaling in dopaminergic neurons. FASEB J 32:819–828. https://doi.org/10.1096/fj.201700713R
Martino D, Johnson I, Leckman JF (2020) What does immunology have to do with normal brain development and the pathophysiology underlying tourette syndrome and related neuropsychiatric disorders? Front Neurol 11:567407. https://doi.org/10.3389/fneur.2020.567407
Worbe Y, Marrakchi-Kacem L, Lecomte S, Valabregue R, Poupon F, Guevara P, Tucholka A, Mangin JF, Vidailhet M, Lehericy S et al (2015) Altered structural connectivity of cortico-striato-pallido-thalamic networks in Gilles de la Tourette syndrome. Brain 138:472–482. https://doi.org/10.1093/brain/awu311
Niewiadomska-Cimicka A, Krzyżosiak A, Ye T, Podleśny-Drabiniok A, Dembélé D, Dollé P, Krężel W (2017) Genome-wide analysis of RARβ transcriptional targets in mouse striatum links retinoic acid signaling with huntington’s disease and other neurodegenerative disorders. Mol Neurobiol 54:3859–3878. https://doi.org/10.1007/s12035-016-0010-4
Lane MA, Bailey SJ (2005) Role of retinoid signalling in the adult brain. Prog Neurobiol 75:275–293. https://doi.org/10.1016/j.pneurobio.2005.03.002
Krezel W, Kastner P, Chambon P (1999) Differential expression of retinoid receptors in the adult mouse central nervous system. Neuroscience 89:1291–1300. https://doi.org/10.1016/s0306-4522(98)00342-x
Pan J, Yu J, Sun L, Xie C, Chang L, Wu J, Hawes S, Saez-Atienzar S, Zheng W, Kung J et al (2019) ALDH1A1 regulates postsynaptic μ-opioid receptor expression in dorsal striatal projection neurons and mitigates dyskinesia through transsynaptic retinoic acid signaling. Sci Rep 9:3602. https://doi.org/10.1038/s41598-019-40326-x
Rataj-Baniowska M, Niewiadomska-Cimicka A, Paschaki M, Szyszka-Niagolov M, Carramolino L, Torres M, Dollé P, Krężel W (2015) Retinoic acid receptor β controls development of striatonigral projection neurons through FGF-dependent and Meis1-dependent mechanisms. J Neurosci 35:14467–14475. https://doi.org/10.1523/jneurosci.1278-15.2015
Liao WL, Tsai HC, Wang HF, Chang J, Lu KM, Wu HL, Lee YC, Tsai TF, Takahashi H, Wagner M et al (2008) Modular patterning of structure and function of the striatum by retinoid receptor signaling. Proc Natl Acad Sci USA 105:6765–6770. https://doi.org/10.1073/pnas.0802109105
Marie A, Leroy J, Darricau M, Alfos S, De Smedt-Peyrusse V, Richard E, Vancassel S, Bosch-Bouju C (2022) Preventive vitamin A supplementation improves striatal function in 6-hydroxydopamine hemiparkinsonian rats. Front Nutr 9:811843. https://doi.org/10.3389/fnut.2022.811843
Ngo VL, Shi Z, Jiang B, Gewirtz AT (2023) Segmented filamentous bacteria impede rotavirus infection via retinoic acid receptor-mediated signaling. Gut microbes 15:2174407. https://doi.org/10.1080/19490976.2023.2174407
Earley ZM, Lisicka W, Sifakis JJ, Aguirre-Gamboa R, Kowalczyk A, Barlow JT, Shaw DG, Discepolo V, Tan IL, Gona S, Ernest JD, Matzinger P, Barreiro LB, Morgun A, Bendelac A, Ismagilov RF, Shulzhenko N, Riesenfeld SJ, Jabri B (2023) GATA4 controls regionalization of tissue immunity and commensal-driven immunopathology. Immunity 56:43-57.e10. https://doi.org/10.1016/j.immuni.2022.12.009
Wu R, Yuan X, Li X, Ma N, Jiang H, Tang H, Xu G, Liu Z, Zhang Z (2022) The bile acid-activated retinoic acid response in dendritic cells is involved in food allergen sensitization. Allergy 77:483–498. https://doi.org/10.1111/all.15039
Geng J, Liu C, Xu J, Wang X, Li X (2023) Potential relationship between Tourette syndrome and gut microbiome. Jornal de pediatria 99:11–16. https://doi.org/10.1016/j.jped.2022.06.002
Li H, Wang Y, Zhao C, Liu J, Zhang L, Li A (2022) Fecal transplantation can alleviate tic severity in a Tourette syndrome mouse model by modulating intestinal flora and promoting serotonin secretion. Chin Med J 135:707–713. https://doi.org/10.1097/CM9.0000000000001885
Fernandes de Abreu DA, Eyles D, Féron F (2009) Vitamin D, a neuro-immunomodulator: implications for neurodegenerative and autoimmune diseases. Psychoneuroendocrinology 34(Suppl 1):S265-277. https://doi.org/10.1016/j.psyneuen.2009.05.023
Ferreira BR, Pio-Abreu JL, Januário C (2014) Tourette’s syndrome and associated disorders: a systematic review. Trends Psychiatry Psychother 36:123–133. https://doi.org/10.1590/2237-6089-2014-1003
Kotsi E, Kotsi E, Perrea DN (2019) Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): a meta-analysis. Attent Defic Hyperact Disord 11:221–232. https://doi.org/10.1007/s12402-018-0276-7
Khoshbakht Y, Bidaki R, Salehi-Abargouei A (2018) Vitamin D status and attention deficit hyperactivity disorder: a systematic review and meta-analysis of observational studies. Adv Nutr (Bethesda, Md) 9:9–20. https://doi.org/10.1093/advances/nmx002
Poh W, Payne JM, Gulenc A, Efron D (2018) Chronic tic disorders in children with ADHD. Arch Dis Child 103:847–852. https://doi.org/10.1136/archdischild-2017-314139
Acknowledgements
The authors acknowledge the phenomenal contribution of the enrolled children and their parents in this study.
Funding
The 12th Youth Fund project of the First Hospital of Jilin University (JDYY11202114) sponsored this work.
Author information
Authors and Affiliations
Contributions
HL designed the research and drafted the manuscript; CW collected the data and drafted the manuscript; BW and JS collected the data and revised the manuscript; CX and HM participated in the process of this research and collected the data; HL and FJ contributed to the study concept and manuscript revision. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was carried out without any commercial or financial commitments that may become potential conflicts of interest.
Ethical approval
This work received ethical approval and registry from the First Hospital of Jilin University. The parents or guardians of the children signed documented informed consent before the initiation of the study.
Consent for publication
All authors contributed to the article and approved the submitted version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, CX., Wang, B., Sun, JJ. et al. Circulating retinol and 25(OH)D contents and their association with symptoms in children with chronic tic disorders. Eur Child Adolesc Psychiatry 33, 1017–1028 (2024). https://doi.org/10.1007/s00787-023-02226-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-023-02226-4