Abstract
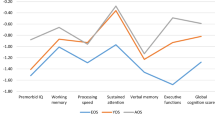
Cognitive impairments are proposed as predictors in the differentiation between subjects with psychosis risk syndrome (PRS) who will develop a psychotic disorder (PRS-P) and those who will not (PRS-NP). More in-depth study of the PRS-NP group could contribute to defining the role of cognitive alterations in psychosis. This study aims to analyze cognition of children and adolescents with PRS in terms of their clinical outcome at 18-month follow-up (psychosis, remission, and non-remission) and of determinate predictors of transition to psychosis and remission of PRS. The method is two-site, naturalistic, longitudinal study design, with 98 help-seeking adolescents with PRS and 64 healthy controls (HC). PRS-P (n = 24) and PRS-NP (n = 74) participants were clinically and cognitively assessed at baseline, and when full-blown psychotic disorder had developed or at 18-month follow-up. PRS-P subjects showed lower scores at baseline in processing speed, visuospatial memory, attention, and executive function (cognitive flexibility/processing speed) compared to HC. PRS-NP subjects showed lower baseline scores in verbal working memory and verbal fluency compared to HC. This deficit is also observed in the PRS group of participants still presenting attenuated psychotic symptoms at 18-month follow-up, while PRS subjects in remission showed a similar cognitive profile to HC subjects. Baseline score on processing speed, measured with a coding task, appeared to be a predictive variable for the development of a psychotic disorder. Performance in verbal working memory was predictive of remission in the PRS-NP. Post hoc comparisons indicate the need for careful interpretation of cognitive markers as predictors of psychosis. Cognitive impairments are present in both PRS-P and PRS-NP. Those individuals who recover from PRS show baseline cognitive performance comparable to the HC group. Together with sociodemographic variables, this observation could help in the differentiation of a variety of PRS trajectories in children and adolescents.

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Murray RM, Lewis SW (1987) Is schizophrenia a neurodevelopmental disorder? Br Med J (Clin Res Ed) 295:681–682
Weinberger DR (1986) The pathogenesis of schizophrenia: a neurodevelopmental theory. In: Nasrallah HA, Weinberger DR (eds) The neurology of schizophrenia. Elsevier, Amsterdam, pp 387–405
Bora E (2017) Neurodevelopmental origin of cognitive impairment in schizophrenia. Psychol Med. https://doi.org/10.1017/S0033291714001263
Murray RM, Bhavsar V, Tripoli G, Howes O (2017) 30 Years on: how the neurodevelopmental hypothesis of schizophrenia morphed into the developmental risk factor model of psychosis. Schizophr Bull 43:1190–1196. https://doi.org/10.1093/schbul/sbx121
Kahn RS, Keefe RSE (2013) Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiat 70:1107–1112. https://doi.org/10.1001/jamapsychiatry.2013.155
Seidman LJ, Mirsky AF (2017) Evolving notions of schizophrenia as a developmental neurocognitive disorder. J Int Neuropsychol Soc 23:881–892. https://doi.org/10.1017/S1355617717001114
Cannon TD, Chung Y, He G et al (2015) Progressive reduction in cortical thickness as psychosis develops: a multisite longitudinal neuroimaging study of youth at elevated clinical risk. Biol Psychiatry 77:147–157. https://doi.org/10.1016/j.biopsych.2014.05.023
Cannon TD (2015) How schizophrenia develops: cognitive and brain mechanisms underlying onset of psychosis. Trends Cogn Sci. https://doi.org/10.1016/j.tics.2015.09.009
Sugranyes G, de la Serna E, Ilzarbe D et al (2020) Brain structural trajectories in youth at familial risk for schizophrenia or bipolar disorder according to development of psychosis spectrum symptoms. J Child Psychol Psychiatry Allied Discip. https://doi.org/10.1111/jcpp.13321
Yung AR, McGorry PD (1996) The prodromal phase of first-episode psychosis: past and current conceptualizations. Schizophr Bull 22:353–370
McGorry P (1995) A treatment-relevant classification of psychotic disorders. Aust N Z J Psychiatry 29:555–558. https://doi.org/10.3109/00048679509064966
Correll CU, Hauser M, Auther AM, Cornblatt BA (2010) Research in people with the psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol Psychiatry 51:390–431. https://doi.org/10.1111/j.1469-7610.2010.02235.x.Research
De Herdt A, Wampers M, Vancampfort D et al (2013) Neurocognition in clinical high risk young adults who did or did not convert to a first schizophrenic psychosis: a meta-analysis. Schizophr Res 149:48–55. https://doi.org/10.1016/j.schres.2013.06.017
Hauser M, Zhang J-P, Sheridan EM et al (2017) Neuropsychological test performance to enhance identification of subjects at clinical high risk for psychosis and be most promising for predictive algorithms for conversion to psychosis: a meta-analysis. J Clin Psychiatry 78178:28–40. https://doi.org/10.4088/JCP.15r10197
Fusar-Poli P, Deste G, Smieskova R et al (2012) Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry 69:562–571. https://doi.org/10.1001/archgenpsychiatry.2011.1592
Bora E, Murray RM (2014) Meta-analysis of cognitive deficits in ultra-high risk to psychosis and first-episode psychosis: do the cognitive deficits progress over, or after, the onset of psychosis? Schizophr Bull 40:744–755. https://doi.org/10.1093/schbul/sbt085
Catalan A, Salazar De Pablo G, Aymerich C et al (2021) Neurocognitive functioning in individuals at clinical high risk for psychosis: a systematic review and meta-analysis. JAMA Psychiat 78:859. https://doi.org/10.1001/JAMAPSYCHIATRY.2021.1290
Lam M, Lee J, Rapisarda A et al (2018) Longitudinal cognitive changes in young individuals at ultrahigh risk for psychosis. JAMA Psychiat 75:929–939. https://doi.org/10.1001/jamapsychiatry.2018.1668
Lee TY, Kim SN, Correll CU et al (2014) Symptomatic and functional remission of subjects at clinical high risk for psychosis: a 2-year naturalistic observational study. Schizophr Res. https://doi.org/10.1016/j.schres.2014.04.002
Cui H, Giuliano AJ, Zhang T et al (2020) Cognitive dysfunction in a psychotropic medication-naïve, clinical high-risk sample from the ShangHai-At-Risk-for-Psychosis (SHARP) study: associations with clinical outcomes. Schizophr Res 226:138–146. https://doi.org/10.1016/j.schres.2020.06.018
Addington J, Stowkowy J, Liu L et al (2019) Clinical and functional characteristics of youth at clinical high-risk for psychosis who do not transition to psychosis. Psychol Med 49:1670–1677. https://doi.org/10.1017/S0033291718002258
Simon AE, Grädel M, Cattapan-Ludewig K et al (2012) Cognitive functioning in at-risk mental states for psychosis and 2-year clinical outcome. Schizophr Res 142:108–115. https://doi.org/10.1016/j.schres.2012.09.004
Cornblatt BA, Lencz T, Smith CW et al (2003) The schizophrenia prodrome revisited: a neurodevelopmental perspective. Schizophr Bull 29:633–651. https://doi.org/10.1093/oxfordjournals.schbul.a007036
Tor J, Dolz M, Sintes A et al (2018) Clinical high risk for psychosis in children and adolescents: a systematic review. Eur Child Adolesc Psychiatry 27:683–700. https://doi.org/10.1007/s00787-017-1046-3
Catalan A, Salazar de Pablo G, Vaquerizo Serrano J et al (2020) Annual research review: prevention of psychosis in adolescents—systematic review and meta-analysis of advances in detection, prognosis and intervention. J Child Psychol Psychiatry Allied Discip. https://doi.org/10.1111/jcpp.13322
Ziermans TB, Durston S, Sprong M et al (2009) No evidence for structural brain changes in young adolescents at ultra high risk for psychosis. Schizophr Res 112:1–6. https://doi.org/10.1016/j.schres.2009.04.013
Ziermans T, de Wit S, Schothorst P et al (2014) Neurocognitive and clinical predictors of long-term outcome in adolescents at ultra-high risk for psychosis: a 6-year follow-up. PLoS ONE 9:e93994. https://doi.org/10.1371/journal.pone.0093994
Tor J, Dolz M, Sintes-Estevez A et al (2020) Neuropsychological profile of children and adolescents with psychosis risk syndrome: the CAPRIS study. Eur Child Adolesc Psychiatry 29:1311–1324. https://doi.org/10.1007/s00787-019-01459-6
Woodberry KA, Seidman LJ, Giuliano AJ et al (2010) Neuropsychological profiles in individuals at clinical high risk for psychosis: relationship to psychosis and intelligence. Schizophr Res 123:188–198. https://doi.org/10.1016/j.schres.2010.06.021
Carrión RE, McLaughlin D, Auther AM et al (2015) The impact of psychosis on the course of cognition: a prospective, nested case-control study in individuals at clinical high-risk for psychosis. Psychol Med. https://doi.org/10.1017/S0033291715001233
Carrión RE, Walder DJ, Auther AM et al (2018) From the psychosis prodrome to the first-episode of psychosis: no evidence of a cognitive decline. J Psychiatr Res 96:231–238. https://doi.org/10.1016/j.jpsychires.2017.10.014
Lencz T, Smith CW, McLaughlin D et al (2006) Generalized and specific neurocognitive deficits in prodromal schizophrenia. Biol Psychiatry 59:863–871. https://doi.org/10.1016/j.biopsych.2005.09.005
Thaden E, Rhinewine JP, Lencz T et al (2006) Early-onset schizophrenia is associated with impaired adolescent development of attentional capacity using the identical pairs continuous performance test. Schizophr Res 81:157–166. https://doi.org/10.1016/j.schres.2005.09.015
Lindgren M, Manninen M, Laajasalo T et al (2010) The relationship between psychotic-like symptoms and neurocognitive performance in a general adolescent psychiatric sample. Schizophr Res 123:77–85. https://doi.org/10.1016/j.schres.2010.07.025
Kim SJ, Lee YJ, Jang JH et al (2012) The relationship between psychotic-like experiences and attention deficits in adolescents. J Psychiatr Res 46:1354–1358. https://doi.org/10.1016/j.jpsychires.2012.07.002
Ziermans TB (2013) Working memory capacity and psychotic-like experiences in a general population sample of adolescents and young adults. Front Psychiatry. https://doi.org/10.3389/fpsyt.2013.00161
Tor J, Dolz M, Sintes-Estevez A et al (2020) Neuropsychological profile of children and adolescents with psychosis risk syndrome: the CAPRIS study. Eur Child Adolesc Psychiatry 13:1062–1072. https://doi.org/10.1007/s00787-019-01459-6
Sheffield JM, Karcher NR, Barch DM (2018) Cognitive deficits in psychotic disorders: a lifespan perspective. Neuropsychol Rev 28:509–533. https://doi.org/10.1007/s11065-018-9388-2
Schultze-Lutter F, Michel C, Schmidt SJ et al (2015) EPA guidance on the early detection of clinical high risk states of psychoses. Eur Psychiatry 30:405–416. https://doi.org/10.1016/j.eurpsy.2015.01.010
Schultze-Lutter F, Hubl D, Schimmelmann BG, Michel C (2017) Age effect on prevalence of ultra-high risk for psychosis symptoms: replication in a clinical sample of an early detection of psychosis service. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-017-0994-y
Simon AE, Cattapan-Ludewig K, Gruber K et al (2009) Subclinical hallucinations in adolescent outpatients: an outcome study. Schizophr Res 108:265–271. https://doi.org/10.1016/j.schres.2008.12.018
Gerstenberg M, Theodoridou A, Traber-Walker N et al (2016) Adolescents and adults at clinical high-risk for psychosis: age-related differences in attenuated positive symptoms syndrome prevalence and entanglement with basic symptoms. Psychol Med 46:1069–1078. https://doi.org/10.1017/S0033291715002627
Schimmelmann BG, Michel C, Martz-Irngartinger A et al (2015) Age matters in the prevalence and clinical significance of ultra-high-risk for psychosis symptoms and criteria in the general population: findings from the BEAR and BEARS-kid studies. World Psychiatry 14:189–197. https://doi.org/10.1002/wps.20216
Dolz M, Tor J, De la Serna E et al (2018) Characterization of children and adolescents with psychosis risk syndrome: The Children and Adolescents Psychosis Risk Syndrome (CAPRIS) study. Early Interv Psychiatry. https://doi.org/10.1111/eip.12728
Miller TJ, McGlashan TH, Rosen JL et al (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull 29:703–715
Lencz T, Smith CW, Auther A et al (2004) Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophr Res 68:37–48. https://doi.org/10.1016/S0920-9964(03)00214-7
Klosterkötter J, Birchwood M, Linszen D, et al (2005) Overview on the recruitment, sample characteristics, and distribution of inclusion criteria of the European Prediction of Psychosis Study (EPOS). Eur PsychiatryPsychiatry Suplement 48
Hollingshead AB, Redlich FC (1958) Social class and mental illness: community study. Wiley, Hoboken
Miller TJ, McGlashan TH, Rosen JL et al (2002) Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry 159:863–865. https://doi.org/10.1176/appi.ajp.159.5.863
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988. https://doi.org/10.1097/00004583-199707000-00021
Hamilton M (1967) Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 6:278–296
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435
Cornblatt BA, Auther AM, Niendam T et al (2007) Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull 33:688–702. https://doi.org/10.1093/schbul/sbm029
Nuechterlein KH, Green MF, Kern RS et al (2008) The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry 165:203–213. https://doi.org/10.1176/appi.ajp.2007.07010042
IBM corp (2016) IBM SPSS Statistics for Windows, Version 24.0
Bang M, Kim KR, Song YY et al (2015) Neurocognitive impairments in individuals at ultra-high risk for psychosis: who will really convert? Aust N Z J Psychiatry 49:462–470. https://doi.org/10.1177/0004867414561527
Seidman LJ, Shapiro DI, Stone WS et al (2016) Association of Neurocognition with transition to psychosis: baseline functioning in the second phase of the North American prodrome longitudinal study. JAMA Psychiat 73:1239. https://doi.org/10.1001/jamapsychiatry.2016.2479
de Paula ALD, Hallak JEC, Maia-de-Oliveira JP et al (2015) Cognition in at-risk mental states for psychosis. Neurosci Biobehav Rev 57:199–208. https://doi.org/10.1016/j.neubiorev.2015.09.006
Castro-Fornieles J, Bargalló N, Calvo A et al (2018) Gray matter changes and cognitive predictors of 2-year follow-up abnormalities in early-onset first-episode psychosis. Eur Child Adolesc Psychiatry 27:113–126. https://doi.org/10.1007/s00787-017-1013-z
Mollon J, David AS, Zammit S et al (2018) Course of cognitive development from infancy to early adulthood in the psychosis spectrum. JAMA Psychiat 75:270–279. https://doi.org/10.1001/jamapsychiatry.2017.4327
Knowles EEM, David AS, Reichenberg A (2010) Processing speed deficits in schizophrenia: reexamining the evidence. Am J Psychiatry 167:828–835. https://doi.org/10.1176/appi.ajp.2010.09070937
Puig O, Penadés R, Baeza I et al (2012) Processing speed and executive functions predict real-world everyday living skills in adolescents with early-onset schizophrenia. Eur Child Adolesc Psychiatry 21:315–326. https://doi.org/10.1007/s00787-012-0262-0
Frommann I, Pukrop R, Brinkmeyer J et al (2011) Neuropsychological profiles in different at-risk states of psychosis: executive control impairment in the early–and additional memory dysfunction in the late–prodromal state. Schizophr Bull 37:861–873. https://doi.org/10.1093/schbul/sbp155
Keefe RSE, Perkins DO, Gu H et al (2006) A longitudinal study of neurocognitive function in individuals at-risk for psychosis. Schizophr Res 88:26–35. https://doi.org/10.1016/j.schres.2006.06.041
Seidman LJ, Giuliano AJ, Meyer EC et al (2010) Neuropsychology of the Prodrome to Psychosis in the NAPLS Consortium<subtitle>Relationship to Family History and Conversion to Psychosis</subtitle><alt-title>Neuropsychology of Prodrome to Psychosis</alt-title>. Arch Gen Psychiatry 67:578. https://doi.org/10.1001/archgenpsychiatry.2010.66
Carrión RE, Goldberg TE, McLaughlin D et al (2011) Impact of neurocognition on social and role functioning in individuals at clinical high risk for psychosis. Am J Psychiatry 168:806–813. https://doi.org/10.1176/appi.ajp.2011.10081209
Bachman P, Niendam TA, Jalbrzikowkski M et al (2012) Processing speed and neurodevelopment in adolescent-onset psychosis: cognitive slowing predicts social function. J Abnorm Child Psychol 40:645–654. https://doi.org/10.1007/s10802-011-9592-5
Addington J, Barbato M (2012) The role of cognitive functioning in the outcome of those at clinical high risk for developing psychosis. Epidemiol Psychiatr Sci 21:335–342. https://doi.org/10.1017/S204579601200042X
Bolt LK, Paul Amminger G, Farhall J et al (2018) Neurocognition as a predictor of transition to psychotic disorder and functional outcomes in ultra-high risk participants: findings from the NEURAPRO randomized clinical trial. Schizophr Res. https://doi.org/10.1016/j.schres.2018.12.013
Kelleher I, Murtagh A, Clarke MC et al (2012) (2013) Neurocognitive performance of a community-based sample of young people at putative ultra high risk for psychosis: support for the processing speed hypothesis. Cogn Neuropsychiatry. https://doi.org/10.1080/13546805.2012.682363
Mam-lam-Fook C, Danset-Alexandre C, Pedron L et al (2017) Neuropsychologie des sujets à ultra-haut risque de psychose (UHR): une analyse critique de la littérature. Encephale 43:241–253. https://doi.org/10.1016/j.encep.2017.02.001
Myles-Worsley M, Ord LM, Ngiralmau H et al (2007) The Palau Early Psychosis Study: neurocognitive functioning in high-risk adolescents. Schizophr Res 89:299–307. https://doi.org/10.1016/j.schres.2006.08.003
Walder DJ, Mittal V, Trotman HD et al (2008) Neurocognition and conversion to psychosis in adolescents at high-risk. Schizophr Res 101:161–168. https://doi.org/10.1016/j.schres.2007.12.477
Pukrop R, Schultze-Lutter F, Ruhrmann S et al (2006) Neurocognitive functioning in subjects at risk for a first episode of psychosis compared with first- and multiple-episode schizophrenia. J Clin Exp Neuropsychol 28:1388–1407. https://doi.org/10.1080/13803390500434425
Zabala A, Rapado M, Arango C et al (2010) Neuropsychological functioning in early-onset first-episode psychosis: comparison of diagnostic subgroups. Eur Arch Psychiatry Clin Neurosci 260:225–233. https://doi.org/10.1007/s00406-009-0046-9
Carrión RE, Demmin D, Auther AM et al (2016) Duration of attenuated positive and negative symptoms in individuals at clinical high risk: associations with risk of conversion to psychosis and functional outcome. J Psychiatr Res 81:95–101. https://doi.org/10.1016/j.jpsychires.2016.06.021
Armando M, Nelson B, Yung AR et al (2010) Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr Res 119:258–265. https://doi.org/10.1016/j.schres.2010.03.001
Fusar-Poli P, Nelson B, Valmaggia L et al (2014) Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull 40:120–131. https://doi.org/10.1093/schbul/sbs136
van Os J, Guloksuz S (2017) A critique of the “ultra-high risk” and “transition” paradigm. World Psychiatry 16:200–206. https://doi.org/10.1002/wps.20423
Dean K, Stevens H, Mortensen PB et al (2010) Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Arch Gen Psychiatry 67:822–829
Lee TY, Shin YS, Shin NY et al (2014) Neurocognitive function as a possible marker for remission from clinical high risk for psychosis. Schizophr Res 153:48–53. https://doi.org/10.1016/j.schres.2014.01.018
Mollon J, David AS, Morgan C et al (2016) Psychotic experiences and neuropsychological functioning in a population-based sample. JAMA Psychiat 73:129–138. https://doi.org/10.1001/jamapsychiatry.2015.2551
McCarthy JB, Weiss SR, Segovich KT, Barbot B (2016) Impact of psychotic symptoms on cognitive functioning in child and adolescent psychiatric inpatients with severe mood disorders. Psychiatry Res 244:223–228. https://doi.org/10.1016/j.psychres.2016.07.049
de Wit S, Wierenga LM, Oranje B et al (2016) Brain development in adolescents at ultra-high risk for psychosis: longitudinal changes related to resilience. NeuroImage Clin 12:542–549. https://doi.org/10.1016/j.nicl.2016.08.013
Stern Y (2009) Cognitive reserve. Neuropsychologia 47:2015–2028
de la Serna E, Andrés-Perpiñá S, Puig O et al (2013) Cognitive reserve as a predictor of two year neuropsychological performance in early onset first-episode schizophrenia. Schizophr Res 143:125–131. https://doi.org/10.1016/j.schres.2012.10.026
Amoretti S, Bernardo M, Bonnin CM et al (2016) The impact of cognitive reserve in the outcome of first-episode psychoses: 2-year follow-up study. Eur Neuropsychopharmacol 26:1638–1648. https://doi.org/10.1016/j.euroneuro.2016.07.003
Camprodon-Boadas P, de la Serna E, Baeza I et al (2020) Cognitive reserve in patients with first-episode psychosis as outcome predictor at 5-year follow-up. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-020-01668-4
Conners K (2000) Conners’ Continuous Performance Test, CPT-II, MHS. ed. Toronto
Heaton R, Chelune GJ, Talley JL, Kay G, Curtiss G (1997) Wisconsin Card Sorting Test (WCST), TEA Edicio. ed. Madrid
Loonstra AS, Tarlow AR, Sellers AH (2001) COWAT metanorms across age, education, and gender. Appl Neuropsychol Adult 8:161–166. https://doi.org/10.1207/S15324826AN0803
Reitan R (1985) The Halstead–Reitan neuropsychological test battery: theory and clinical interpretation, Reitan Neu. ed. Tucson, Arizona
Reynolds CR, Bigler ED (2001) TOMAL: test de memoria y aprendizaje, TEA Edicio. ed. Madrid
Wechsler D (2003) Wechsler Intelligence Scale for Children-IV (WISC-IV), TEA Edicio. ed. Madrid
Wechsler D (2001) Escala de inteligencia de Wechsler para adultos (WAIS-III), TEA Edicio. ed. Madrid
Wechsler D (1997) The Wechsler Memory Scale, 3rd edn. (WMS-III), TEA Edicio. ed. Madrid
Acknowledgements
IB would like to thank ISCIII for her support (INT19/00021). All the authors would like to thank all the participants in this study.
Funding
This study was supported by grants from the Carlos III Institute (ISCIII), Spanish Department of Health (Fondo de Investigación Sanitaria PI11/1349; PI11/02684; PI15/0444; PI15/00509, PI18/0242, PI18/0976, PI21/0396, PI21/0090, PI21/0330), CIBERSAM Network, Fundación Alicia Koplowitz, and Fondos FEDER, “Una manera de hacer Europa”.
Author information
Authors and Affiliations
Contributions
MD and IB designed the study and wrote the protocol. JT manages the literature search, performed data analysis and wrote the first draft. All authors contributed to the planning of the study and enrolling participants. All authors critically reviewed the paper, and have approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
JT, AS, ES, OP, and DM declare that they have no conflict of interest. JA has received support to attend conferences or honoraria for lectures from Otsuka-Lundbeck and Janssen, Shire, Rubio, and Exeltis Healthcare. Dr. Sugranyes has received grants from the Spanish Ministry of Health, Instituto de Salud Carlos III «Health Research Fund»/ FEDER funds (PI18/00976; PI21/00330); Fundació Clínic Recerca Biomèdica (Ajut a la Recerca Pons Bartran), Alicia Koplowitz Foundation; European Commission (grant Number 101057529); the Brain and Behaviour Research Foundation (NARSAD Young Investigator Award ID 26731); and the Government of Catalonia (PERIS award SLT006/17/00362). She has received speaker fees from Angelini Pharma and consulting fees from Fenix Group. IB has received grants from the Spanish Ministry of Health, Instituto de Salud Carlos III (PI11/1349; PI15/0444; PI18/0242; PI21/0396) and Fundación Alicia Koplowitz, financial support from ISCIII (INT19/00021) and has received support to attend conferences or speaker fees from Otsuka-Lundbeck, Angelini, and Janssen. MD has received grants from Fundación Alicia Koplowitz; the Spanish Ministry of Health, Instituto de Salud Carlos III (PI11/02684; PI15/00509; PI21/0090) and she has received support to attend conferences or speaker fees from Shire, Janssen and Osuka-Lundbeck.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tor, J., Baeza, I., Sintes-Estevez, A. et al. Cognitive predictors of transition and remission of psychosis risk syndrome in a child and adolescent sample: longitudinal findings from the CAPRIS study. Eur Child Adolesc Psychiatry 33, 89–104 (2024). https://doi.org/10.1007/s00787-022-02137-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-022-02137-w