Abstract
The objective of this study is to investigate the prevalence of autism (ASD) symptoms, i.e. , social difficulties, repetitive behaviors, and communicational problems, among children born extremely preterm (EP) compared to a reference group, and to investigate possible antecedents of ASD symptoms among EP children. Method is a national Norwegian cohort of 11 year old EP children, excluding those with intellectual disabilities, non-ambulatory cerebral palsy, blindness, and/or deafness. Parents and teachers reported ASD symptoms using The Autism Spectrum Screening Questionnaire (ASSQ). Social difficulties, repetitive behaviors, communicational problems, and a total ASSQ score were presented. Combined ratings on the ASSQ was defined as parent and/or teacher scoring the child ≥ 98th percentile of the reference group, which was the population-based Bergen Child Study. Of eligible children, 216 (64%) EP and 1882 (61%) reference children participated. EP children had significantly higher mean scores and combined ratings on social difficulties (14.5% vs. 4.1%, OR: 3.2), repetitive behaviors (23.7% vs. 4.0%, OR: 6.4), communicational problems (23.1% vs. 4.8%, OR: 5.4), and the total ASSQ score (18.3% vs. 3.4%, OR: 5.7) compared to reference children. Only no prenatal steroids, IQ 70–84, and mental health problems at 5 years of age were significantly associated with ASD symptoms at 11 years of age. EP children were at increased risk of social difficulties, repetitive behaviors, and communicational problems, and approximately one out of five were reported as high scorers of ASD symptoms. No prenatal steroids use, IQ in the lower range, and mental health problems at 5 years of age were associated with ASD symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Social difficulties, repetitive behaviors, and communication deficits are the three main symptom domains of Autism Spectrum Disorder (ASD) [1]. The prevalence of ASD among children born extremely preterm (EP), defined as gestational age < 28 weeks or birth weight < 1000 g, has been estimated to 7–8% [2, 3], which is significantly higher than the expected prevalence rate of 0.7% in the general population [4]. EP born children without a diagnosis of ASD also have a higher load of ASD symptoms compared to term born children [5]. Children suffering from severe neurodevelopmental disabilities (NDD), i.e., non-ambulatory cerebral palsy (CP), intellectual disabilities (ID), blindness, and deafness, are at increased risk of ASD [6, 7]. EP children are at increased risk of severe NDD [8]. Interestingly, even after excluding those with severe NDD [9] and IQ < 85 [10], EP children are still at risk of ASD symptoms compared to controls.
Most studies investigating ASD symptoms in EP children report this as a total score [2, 3, 10,11,12,13]. However, one study of EP children [5] excluding those with ASD and IQ < 85 investigated the three main symptom domains of ASD separately, finding EP children at increased risk in all the domains compared to norm data. Another study including EP children regardless of cognitive function and ASD had similar findings [14]. However, after adjusting for IQ, repetitive behavior was no longer significantly different compared to term controls. Children with visual and hearing impairments and non-ambulatory CP were included in all the analyses in these two studies, bringing uncertainties to the findings [13]. To understand more fully what the reported ASD symptoms in EP children represents, further studies are needed.
The few studies investigating antecedents of ASD symptoms in EP children report bronchopulmonary dysplasia (BPD) [10, 15], jaundice [16], lower gestational age [14, 17], and neonatal brain abnormalities [14, 16, 17] to be associated with ASD symptoms in EP children. In addition, lower socioeconomic status (SES) [16], cognitive impairment, special educational needs, and poorer academic attainment [14] have been found to co-occur with ASD symptoms in EP children. Due to the increased risk of ASD symptoms in EP born, understanding the mechanisms and identifying possible antecedents would be valuable.
The aims of the present study of a national cohort of EP children at 11 years of age were: (1) To investigate the prevalence and nature of symptoms and the three main symptom domains of ASD, among children born EP without non-ambulatory CP, intellectual disabilities, deafness or blindness compared to a reference group. (2) To investigate possible antecedents of ASD symptoms among EP children including pre, neonatal and perinatal factors, mental health problems, and functional outcomes at 5 years of age.
Method
Populations
EP group
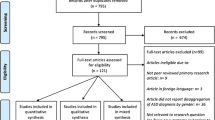
The target population was a national cohort of all children born EP (gestational age (GA) < 28 weeks or birth weight (BW) < 1000 g) in Norway in 1999 and 2000 (n = 638). Of the 638 children born EP, 2 refused to participate, and 263 children died before 2 years of age. One child died between the 2 and 5 year follow-up. Both at 5 and 11 years of age, 372 (58% of the total) EP children were alive. At 5 years of age, 306 EP children attended somatic examination, and 255 of them completed mental health questionnaires. The EP children were prospectively assessed during their stay in the neonatal intensive care unit (NICU) and at 2, 5, and 11 years of age. At 2 and 5 years, they were assessed by experienced pediatricians, and at 5 years, psychologists assessed IQ using the Wechsler Preschool and Primary Scale of Intelligence-Revised (WPPSI-R) [18]. At 11 years of age, information was based on parent- and teacher-reported questionnaires. Characteristics of the cohort, definitions of neonatal characteristics, and overall outcome in terms of mortality and morbidity until 11 years of age have been published [19,20,21,22,23,24,25].
At 11 years of age, EP children were excluded if they at 5 years had an IQ < 70, non-ambulatory CP (class 4–5 on the Gross Motor Function for Classification of CP-GMFCS [26]), deafness, and/or blindness (n = 33) [22]. For children who did not participate at 5 but at 11 years of age (n = 35) [11], they were excluded based on information obtained from the 2 year follow-up [23]. None of the 35 children had CP, and were blind or deaf. An experienced pediatrician contacted the parents of 17 children by phone to obtain information on ID diagnosis, given that the information in the questionnaires were not sufficient. None of them had parent-reported ID diagnosis. One family was not approached, because the parents had not consented to further contact. A total of 338 EP children were eligible at 11 years of age, and of those 216 (64%) attended. Of them 161 (75%) were born with GA < 28, and 179 (83%) had BW < 1000 g. Furthermore, 69 of the 216 EP children were SGA, and of them, 31 (45%) children had mothers with preeclampsia. Parent-reported questionnaire was available for all participants, and the teacher report for 186 children. Regarding the assessed EP children, they had higher educated mothers, more BPD, less retinopathy, fewer were boys, and fewer had NDD and ambulatory CP at 5 years, compared to those not assessed [11].
Reference group
The reference group was the Bergen Child Study, an unselected population of 11-year-old children living in the municipality of Bergen, Norway [27, 28]. All children born in 1995 who attended public or private schools were invited, and 1893 (61%) participated. Children with ID, according to parent report (n = 11), were excluded. Six children were reported with CP without ID, and were included in the study, with unknown level of ambulation. Children with blindness or deafness without ID may have been included, as necessary information was lacking. A total of 1882 (61%) children were eligible and included in the analysis, including parents’ completed questionnaires for 1767 (57%) and teachers’ questionnaires for 1880 (61%) [11].
Comparing the attending children in the reference and the EP group, the number of fathers with higher education was significantly higher in the reference group, and father’s education was adjusted for in all the analyses comparing the two groups. Higher education was defined as at least 3 years of education at university level. There was no statistical significant difference between the proportion of mother’s with higher education and proportion of boys (see Online Resource 1) [11].
The autism spectrum screening questionnaire (ASSQ)
The Autism Spectrum Screening Questionnaire (ASSQ) is a 27-item questionnaire reflecting symptoms of ASD; social interaction problems, motor clumsiness, repetitive behavior, and tics [29,30,31,32]. The ASSQ was developed by Ehlers and Gillberg as a screening tool intended to identify children who need more comprehensive evaluation for suspected ASD. The test–retest stability for the ASSQ have previously been 0.94 for teachers and 0.96 for parents during a 2 week period [33]. The items can be allocated into three subscales as recommended by Ryland et al. [32]. The subscales are (1) social interaction difficulties; addressing challenges with friendship, prosocial behavior, and social communication (11 items); (2) repetitive behavior (tics/motor/OCD); repetitive, stereotype autism-associated symptoms, such as motoric problems and tics (8 items); (3) autistic style/ communication difficulties; addressing a social–cognitive style and language/communication difficulties (7 items). In addition, a Total Score were presented, including all the items. The 27 items are answered on a scale from “not true” (0), “sometimes true” (1), to “certainly true” (2), giving a possible range of scores from 0 to 54 in total. Higher scores indicate higher frequency of symptoms. One of the items (number 9) was by accident absent in the reference group, and therefore not included in our data. We substituted missing items with the mean individual score for all the items in ASSQ. No child missed more than one item. Both mean scores and cut-off scores ≥ 98th percentile of the reference group were presented. Due to the stepwise change in ASSQ scores, the exact 98 percentiles could not be found in all cases, and some of the scores were approximate. Parents and teachers cut-off score ≥ 98th percentile were > 8 for social interaction difficulties, > 3 and > 2 for repetitive behavior, > 6.7 and > 3 for autistic style, and > 16 and > 13 for the Total score, respectively. In addition, a high combined score for each scale is defined as parent and/or teacher score of the child ≥ 98th percentile for the reference group. A high combined total ASSQ score (when parent and/or teacher score the child ≥ 98th percentile of the reference group on the total score) has been shown to give the highest specificity (0.86) and sensitivity (0.91) for detecting ASD in a Norwegian study [30]. Where parent or teacher report was missing, the child was excluded from this analysis. The ASSQ has not been validated for children with severe CP, blindness, deafness, or IQ < 50.
Statistical analyses
First, mean ASSQ scores with t tests, ASSQ scores ≥ 98 percentiles for the reference group, and the combined ASSQ score with χ2 tests were compared between the EP and the reference group (Table 1). All the analyses in Table 1 were adjusted for fathers’ higher education, performing regression analyses, logistic or linear as appropriate, with ASSQ outcome as the dependent variable, and group and fathers’ higher education as independent variables. Second, the proportion of all the single ASSQ items scored as 1 or 2 were analyzed in both groups with Chi-square tests. Furthermore, binary correlation analyses were performed separately for the EP and reference children between single items and the total ASSQ score ≥ 98 percentiles for both parents and teachers report. Finally, logistic regression analyses were performed individually for each possible antecedent factor for the EP children, with a combined total ASSQ score ≥ 98 percentiles for the reference group as dependent variable, to investigate potential antecedents separately. Not all the 186 children with a combined total ASSQ score ≥ 98 percentiles had information regarding the different antecedent factors, and therefore, the number included in the analysis differs; see Table 3 for more information. In addition, a false discovery rate is calculated and presented for the p values in Table 3.
A p value of < 0.05 was considered statistically significant. The SPSS statistical package version 25.0 (IBM SPSS Statistics, IBM Corporation) was used for all analyses.
The Regional Committee on Medical Research Ethics and The Norwegian Data Inspectorate approved the study, and parents gave written informed consent.
Results
Total score of autism symptoms
EP children had significantly higher (p < 0.001) mean scores on both parent- and teacher-reported total ASSQ score and significantly increased odds of a high combined total ASSQ score (OR: 5.7; 95% CI 3.4–9.4) compared to the reference group (Table 1).
Social interaction difficulties
Regarding social interaction problems reported by parents and teachers, the EP children had significantly higher (p ≤ 0.001) mean scores, increased odds of being scored ≥ the 98th percentile (OR: 3.0 and OR: 3.5, respectively), as well as odds (OR: 3.2) of having a combined social interaction problem score compared to the reference group (Table 1). Both parents and teachers reported “No social fit in language” (28.8 and 29.4%, respectively) as the most frequent individual item in the social interaction domain for the EP children. “Lacks common sense” was the single item with the highest correlation (0.56) to parent-reported total ASSQ score ≥ 98th percentile. “Poor at games, own rules” were the single item for the EP children with the highest correlation (0.66) to teachers reported total ASSQ score ≥ 98th percentile (Table 2).
Repetitive behavior (tics/motor/OCD)
For repetitive behavior reported by parents and teachers, the EP children had significantly higher mean scores (p < 0.001), odds of being scored ≥ the 98th percentile (OR: 2.6 and OR: 10.7, respectively), and odds (OR 6.4) of having a combined repetitive behavior score compared to the reference group (Table 1). “Clumsy” was the most frequent individual item reported by both parents and teachers (16.3 and 30.5%, respectively) (Table 2). “Idiosyncratic attachment” was the single item with the highest correlation (0.54) to parent-reported total ASSQ score ≥ 98th percentile, whereas “Clumsy” was the single item for the EP children with the highest correlation (0.55) to teachers reported total ASSQ score ≥ 98th percentile (Table 2).
Autistic style/communication difficulties
Concerning autistic style, EP children had significantly higher (p < 0.001) mean scores reported both by parents and teachers, and increased odds (OR: 7.5) of being scored ≥ the 98th percentile reported by teachers, and increased odds (OR: 5.4) of having a combined autistic style score compared to the reference group. Parental report score ≥ the 98th percentile between the two groups was not significantly different (Table 1). Both parents and teachers reported “Old-fashioned or precocious” as the most frequent individual item (41.9 and 36.4%, respectively). “Literal understanding” was the single item with the highest correlation (0.42) to parent-reported total ASSQ score ≥ 98th percentile, and “Uneven abilities” was the single item for the EP children with the highest correlation (0.55) to teachers reported total ASSQ score ≥ 98th percentile (Table 2).
Antecedents of a combined total score for the EP children
Of the 27 variables investigated as antecedents of a combined Total Score for the EP children, three were significantly associated with increased risk; no prenatal steroids (p = 0.002), IQ in the lower normal range (IQ 70–84) (p = 0.008), and mental health problems at 5 years of age (p = 0.001). After performing false discovery rate analysis, IQ in the lower normal range (IQ 70–84) (p = 0.008) was no longer significant (p = 0.072, Table 3).
Discussion
The present study found children born EP without non-ambulatory CP, intellectual disabilities, deafness, or blindness to be at a twofold to more than tenfold increased risk of exhibiting autism symptoms compared to reference children. Almost one in five EP children were rated with a combined Total ASSQ score ≥ 98th percentile. Repetitive behavior symptoms were reported with the highest risk of the three ASD symptom domains compared to the reference children. The single ASSQ item with the highest correlation to the Total ASSQ score ≥ 98th percentile for parents was “Lacks common sense” and for teachers “Poor at games, own rules”. Antecedents for ASD symptoms at 11 years of age were not receiving steroids prenatal, IQ in the lower normal range, and mental health problems at 5 years of age.
Strengths of the present study were the large national population-based sample of EP children followed up repeatedly until 11 years of age, the use of a large unselected reference group, multi-informants for autism symptoms, the prospective design, the examination at 5 years of age by psychologist, pediatrician and physiotherapist, substantial information from the NICU, and a small variation in age at assessment. Another strength of the study was the exclusion of children with severe NDD, thereby reducing the proportion of false positives [13]. However, this has possibly excluded most children with ASD from the EP sample, as ID and severe CP often co-occur in EP children with ASD [10]. As Korzeniewski et al. [5], the present study may therefore mainly describe EP children without ASD and ID affecting the outcome of the different main areas of ASD symptoms. A weakness was the use of a screening tool, and not a diagnostic tool, for autism. Further weaknesses were suboptimal follow-up rates, which also limited the power to adjust for additional potentially confounding factors, and lack of data on the eligible reference children who did not participate. However, at 7–9 years of age, it was estimated that the reference participants had fewer mental health symptoms than the nonparticipants [34]. This may also be the case for the EP group, since the attending children had a higher proportion of mothers with higher education, which is associated with less-frequent mental health problems for their children [19]. In addition, some children with ID may have been included both in the EP and the control group, since IQ was not tested at 11 years. Finally, we cannot exclude that the loss of 1 item on the ASSQ may have reduced the validity of the findings.
In accordance with one EP study excluding those with ASD and IQ < 85, the present study found increased risk of all the main symptom domains of ASD for the children born EP compared to the reference group [5]. This is in contrast to another EP study, where Johnson et al. found increased risk of social difficulties and communication deficits, and not repetitive behavior after adjusting for IQ [14]. Interestingly, in accordance with a study of very preterm born children (GA < 32) [35], the present study found repetitive behavior to be the ASD symptom domain with the highest risk for the EP children. However, the most frequent item in the repetitive symptom domain reported by both parents and teachers in the present study was being “Clumsy”. Children born EP are at increased risk of minor motor problems and clumsiness [36], and the high rate of repetitive behavior may be due to clumsiness and not due to ASD. This may reflect a challenge in EP research due to the high prevalence of comorbid conditions with overlapping symptoms. Furthermore, a contributing factor to the differing outcome to Johnson et al., may be their lack of teacher’s informants, as teachers in the present study reported a considerably greater symptom load of repetitive behavior than parents. Finally, the use of different screening tools in these studies may be a possible explanation for the differing outcomes.
To our knowledge, no study in EP children has previous investigated single symptoms of ASD. A study of adolescents born with very low birth weight (VLBW ≤ 1500 g) [37] found them to be high scorers on the ASSQ items; ‘‘Uses language freely, but fails to make adjustment to fit social contexts or the needs of different listeners’’ [37], which in the present study both parents and teachers reported as the most frequent individual item in the social interaction domain. Korzeniewski et al. investigated ASD symptoms in EP children without ASD [5], and found those with a high ASD score to more often have deficits in language and communication. This may suggest that communicational problems represent a great deal of the increased frequency of ASD symptoms previously reported. Furthermore, the VLBW study [37] reported them to be high scorers on the ASSQ items; “Fails to make friends” which was highly correlated to a total ASSQ score in the present study. There might be several explanations for failing to make friends. In addition to language and communication problems, EP children are at increased risk of inattention, emotional problems [11], and lower cognitive function [8], important domains affecting peer relationships. Detecting and helping EP children in need of support for socialization are important, as having friends is a fundamental part of quality of life including social activity and participation.
In accordance with one previous EP study [14], we found IQ in the lower normal range (70–84) and mental health problems at preschool age to be significant predictors of ASD symptoms at 11 years of age. This may not surprise as ASD occurs early in life and lasts a lifetime, and often co-exist with lower cognitive function and other mental health problems [38]. However, for those without ASD, this may reflect a cognitive and mental vulnerability early in childhood being a risk factor for later mental health problems, such as ASD symptoms or social difficulties. This could also be explained by the demands in social interaction, increasing with age and becoming more obvious for those surroundings the EP child.
In contrast to previous studies investigating neonatal factors [10, 14,15,16], the present study found that only not receiving prenatal steroids correlated with ASD symptoms at 11 years of age. The contradicting findings may be due to differences in statistical strategies. Interestingly, the previous findings reflects an additional vulnerability in the neonatal period which may affect the development of the brain causing ASD symptoms among other things.
Conclusion
In this study of Norwegian children born EP without severe functional disabilities are at a twofold to tenfold increased risk of very high scores on all main symptom domains of ASD. Almost every fifth EP child had high scores of ASD symptoms. Not receiving prenatal steroids, IQ in the lower normal range, and mental health problems at 5 years of age were predictors of ASD symptoms at 11 years. However, limitations to the study should be taken into account regarding generalizability to other settings. Understanding the complex pattern of potential mental health problems is important for parents, health care personnel, teachers, and others who relate to children born EP.
Data availability
In accordance with the approvals granted for this study by The Regional Committee on Medical Research Ethics and The Norwegian Data Inspectorate, the data files are stored securely and in accordance with the Norwegian Law of Privacy Protection. The data file cannot be made publicly available as this might compromise the respondents’ privacy. Some of the participating centers are small and the number of extremely preterm births limited with a risk of identifying pseudonymous participants. To prepare future research papers, other researchers in our group currently use the data file. A subset of the data file with anonymized data can be made available to interested researchers upon reasonable request to Maria Vollsæter (maria.vollseter@helse-bergen.no), providing that Norwegian privacy legislation and GDPR are respected, and that permission is granted from The Norwegian Data Inspectorate and the data protection officer at Haukeland University Hospital.
Code availability
Not applicable.
Change history
21 June 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00787-022-02026-2
Abbreviations
- EP:
-
Extremely premature
- ASD:
-
Autism spectrum disorder
- ID:
-
Intellectual disabilities
- CP:
-
Cerebral palsy
- NICU:
-
Neonatal intensive care unit
- ASSQ:
-
The Autism Spectrum Screening Questionnaire
References
ICD-10. ICD-10 Diagnosis code F84.0. Available from: http://icdlist.com/icd-10/F84.0. Accessed 5 Mar 2021.
Johnson S, Hollis C, Kochhar P et al (2010) Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J Am Acad Child Adolesc Psychiatry 49(5):453–463 (e1)
Joseph RM, O’Shea TM, Allred EN et al (2017) Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res 10(2):224–232
Suren P, Bakken IJ, Aase H et al (2012) Autism spectrum disorder, ADHD, epilepsy, and cerebral palsy in Norwegian children. Pediatrics 130(1):e152–e158
Korzeniewski SJ, Joseph RM, Kim SH et al (2017) Social responsiveness scale assessment of the preterm behavioral phenotype in 10-year-olds born extremely preterm. J Dev Behav Pediatr 38(9):697–705
Einfeld SL, Tonge BJ (1996) Population prevalence of psychopathology in children and adolescents with intellectual disability: II. Epidemiological findings J Intellect Disabil Res 40(Pt 2):99–109
Kilincaslan A, Mukaddes NM (2009) Pervasive developmental disorders in individuals with cerebral palsy. Dev Med Child Neurol 51(4):289–294
Johnson S, Fawke J, Hennessy E et al (2009) Neurodevelopmental disability through 11 years of age in children born before 26 weeks of gestation. Pediatrics 124(2):e249–e257
Samuelsson M, Holsti A, Adamsson M et al (2017) Behavioral patterns in adolescents born at 23 to 25 weeks of gestation. Pediatrics 140(1):e20170199
Hack M, Taylor HG, Schluchter M et al (2009) Behavioral outcomes of extremely low birth weight children at age 8 years. J Dev Behav Pediatr 30(2):122–130
Fevang SKE, Hysing M, Markestad T et al (2016) Mental health in children born extremely preterm without severe neurodevelopmental disabilities. Pediatrics 137(4):e20153002
Larroque B, Ancel PY, Marchand-Martin L et al (2011) Special care and school difficulties in 8-year-old very preterm children: the Epipage cohort study. PLoS ONE 6(7):e21361
Johnson S, Hollis C, Hennessy E et al (2011) Screening for autism in preterm children: diagnostic utility of the social communication questionnaire. Arch Dis Child 96(1):73–77
Johnson S, Hollis C, Kochhar P et al (2010) Autism spectrum disorders in extremely preterm children. J Pediatr 156(4):525–531 (e2)
Vederhus BJ, Markestad T, Eide GE et al (2010) Health related quality of life after extremely preterm birth: a matched controlled cohort study. Health Qual Life Outcomes 8:53
Taylor HG, Klein N, Drotar D et al (2006) Consequences and risks of <1000-g birth weight for neuropsychological skills, achievement, and adaptive functioning. J Dev Behav Pediatr 27(6):459–469
Ritchie K, Bora S, Woodward LJ (2015) Social development of children born very preterm: a systematic review. Dev Med Child Neurol 57(10):899–918
Wechsler D (1999) Wechsler preschool and primary scale of intelligence-revised [Swedish edition]. Psykologförlaget AB, Stockholm
Elgen SK, Leversen KT, Grundt JH et al (2012) Mental health at 5 years among children born extremely preterm: a national population-based study. Eur Child Adolesc Psychiatry 21(10):583–589
Elgen SK, Sommerfelt K, Leversen KT et al (2014) Minor neurodevelopmental impairments are associated with increased occurrence of ADHD symptoms in children born extremely preterm. Eur Child Adolesc Psychiatry 4:463–470
Fevang SKE, Hysing M, Sommerfelt K et al (2017) Mental health assessed by the strengths and difficulties questionnaire for children born extremely preterm without severe disabilities at 11 years of age: a norwegian, national population-based study. Eur Child Adolesc Psychiatry 12:1523–1531
Leversen KT, Sommerfelt K, Ronnestad A et al (2011) Prediction of neurodevelopmental and sensory outcome at 5 years in Norwegian children born extremely preterm. Pediatrics 127(3):e630–e638
Leversen KT, Sommerfelt K, Ronnestad A et al (2010) Predicting neurosensory disabilities at two years of age in a national cohort of extremely premature infants. Early Hum Dev 86(9):581–586
Westby Wold SH, Sommerfelt K, Reigstad H et al (2009) Neonatal mortality and morbidity in extremely preterm small for gestational age infants: a population based study. Arch Dis Child Fetal Neonatal Ed 94(5):F363–F367
Markestad T, Kaaresen PI, Ronnestad A et al (2005) Early death, morbidity, and need of treatment among extremely premature infants. Pediatrics 115(5):1289–1298
Palisano R, Rosenbaum P, Walter S et al (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39(4):214–223
Hysing M, Sivertsen B, Stormark KM et al (2009) Sleep in children with chronic illness, and the relation to emotional and behavioral problems—a population-based study. J Pediatr Psychol 34(6):665–670
Heiervang E, Stormark KM, Lundervold AJ et al (2007) Psychiatric disorders in Norwegian 8- to 10-year-olds: an epidemiological survey of prevalence, risk factors, and service use. J Am Acad Child Adolesc Psychiatry 46(4):438–447
Posserud M, Lundevold AJ, Lie A et al (2010) The prevalence of autism spectrum disorders: impact of diagnostic instrument and non-response bias. Soc Psychiatry Psychiatr Epidemiol 45(3):319–327
Posserud MB, Lundervold AJ, Gillberg C (2009) Validation of the autism spectrum screening questionnaire in a total population sample. J Autism Dev Disord 39(1):126–134
Posserud MB, Lundervold AJ, Gillberg C (2006) Autistic features in a total population of 7-9-year-old children assessed by the ASSQ (Autism Spectrum Screening Questionnaire). J Child Psychol Psychiatry 47(2):167–175
Ryland HK, Hysing M, Posserud MB et al (2012) Autism spectrum symptoms in children with neurological disorders. Child Adolesc Psychiatry Ment Health 6(1):34
Ehlers S, Gillberg C, Wing L (1999) A screening questionnaire for Asperger syndrome and other high-functioning autism spectrum disorders in school age children. J Autism Dev Disord 29(2):129–141
Stormark KM, Heiervang E, Heimann M et al (2008) Predicting nonresponse bias from teacher ratings of mental health problems in primary school children. J Abnorm Child Psychol 36(3):411–419
Twilhaar ES, de Kieviet JF, Bergwerff CE et al (2019) Social adjustment in adolescents born very preterm: evidence for a cognitive basis of social problems. J Pediatr 213:66–73 (e1)
Hack M, Taylor HG, Drotar D et al (2005) Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA 294(3):318–325
Indredavik MS, Vik T, Heyerdahl S et al (2004) Psychiatric symptoms and disorders in adolescents with low birth weight. Arch Dis Child Fetal Neonatal Ed 89(5):F445–F450
Gjevik E, Eldevik S, Fjaeran-Granum T et al (2011) Kiddie-SADS reveals high rates of DSM-IV disorders in children and adolescents with autism spectrum disorders. J Autism Dev Disord 41(6):761–769
Acknowledgements
Thanks to members of the Project Extreme Premature Group and all the children born extremely premature. A special acknowledgment goes the Bergen Child Study, for providing this study with a unique and solid reference group.
Funding
Open access funding provided by University of Bergen (incl Haukeland University Hospital). The research was supported by The Western Norway Regional Health Authority.
Author information
Authors and Affiliations
Contributions
We confirm that all authors are responsible for reported research, and that all authors have participated in the concept and design, analysis and interpretation of data, and drafting or revising of the manuscript, and have approved the manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Compliance with ethical standards. The Regional Committee on Medical Research Ethics and The Norwegian Data Inspectorate approved the study.
Consent to participate
Parents gave written informed consent. I confirm that all authors have approved this manuscript for submission, and that all participants have given consent for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elgen, S.K.F., Røiseland, M.A., Bircow, E.I. et al. Symptoms and antecedents of autism in children born extremely premature: a national population-based study. Eur Child Adolesc Psychiatry 32, 1579–1588 (2023). https://doi.org/10.1007/s00787-022-01953-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-022-01953-4