Abstract
Objectives
This systematic review and meta-analysis aimed to evaluate the prevalence of middle mesial canal (MMC) in permanent mandibular molars of different populations and regions based on cone-beam computed tomography (CBCT) studies.
Materials and methods
PubMed, Scopus, Embase, Web of Science, and Open-Grey were searched up to October 2023 according to specific keywords. A hand search was conducted on the references of the included studies and articles from three peer-reviewed journals in endodontics. The main variable of interest was the prevalence of MMC. Additional data such as the total number of included cases, age and country of the population, CBCT device information, voxel size, and field of view details were also extracted. Extracted data were analyzed qualitatively with the JBI quality assessment checklist and quantitatively with STATA software.
Results
Of 32,793 studied teeth, the cumulative prevalence of MMC in both mandibular 1st and 2nd molars was 3.11% (95% CI: 2.00-4.44%). The subgroup analysis reveals a prevalence of 4.15% (95% CI: 2.69-5.89%) for mandibular 1st molars and 1.2% (95% CI: 0.2-2.83%) for mandibular 2nd molars. The highest prevalence of MMC in 1st molar was attributed to South Asia (11.24%) and Africa (6.61%).
Conclusions
The prevalence of MMC varies among regions. Clinicians should be aware of the potential prevalence of MMC, particularly in mandibular first molars, as a missed MMC could result in endodontic failure.
Clinical relevance
The presence of MMCs varies in different geographic regions (0% to 29.7%). Clinicians should always look for MMC when doing an endodontic treatment on mandibular molars, as the presence of this canal is not uncommon. We suggest searching for this canal as if searching for the second mesiobuccal canal of maxillary 1st molars.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The inability to identify and debride all infected root canals can contribute to failure in root canal treatment [1, 2]. The complexities of anatomy can limit the ability of clinicians to see or find root canals and hence reduce their ability to disinfect and adequately obturate the canals [2].
Mandibular 1st and 2nd molars have been commonly described as having two roots, one mesial and one distal [3, 4], with the mesial root having a mesiobuccal (MB) and a mesiolingual canal (ML), while the distal root has a single canal [5]. A variation is an additional canal originating between the MB and the ML canal, referred to as the middle mesial canal (MMC) [6]. Due to the poor accessibility of the MMC, this canal might act as a reservoir for residual infected pulp tissue and bacteria, leading to persistent apical periodontitis [2, 7].
A systematic review assessed MMC’s prevalence, finding that MMCs ranged between 0.26-53.8% [8]. This wide range was related to the included studies that varied in methodology. The methods of the studies included the clearing technique, conventional radiography, scanning electron microscope, dental operating microscope (DOM), cone-beam computed tomography (CBCT), and micro-CT. Moreover, their search keywords were somehow limited and were not comprehensive.
Micro-CT studies are accurate and can reveal details of the root canal anatomy. However, the sample size of such studies is often limited due to the expenses of such studies [9]. Moreover, they can only be performed on extracted teeth that are not representative of healthy teeth because extracted teeth may have been associated with endodontic or periodontal disease [10]. Furthermore, these studies are primarily performed on a pool of extracted teeth; therefore, they cannot differentiate between the extracted 1st, 2nd, and 3rd molars.
Clinical in vivo studies with an operating microscope can explore negotiable MMCs in non-extracted teeth [11, 12]. However, it may be difficult to distinguish a true MMC from an isthmus [11]; therefore, a higher incidence of MMC may be found in such studies.
CBCT is as accurate as micro-CT for identifying canals and is clinically realistic for what can be identified when treating patients [9]. CBCT has the advantages of being in vivo and non-invasive and allows for expanding the sample size compared to microscopic analysis or other laboratory studies using extracted teeth. CBCT is an appropriate in vivo tool for evaluating anatomic variations and has been widely used to study large populations [13, 14]. In addition, detailed epidemiological data such as gender, race, and ethnicity can also be obtained from CBCT studies.
Recently, a meta-analysis was performed on the global prevalence of MMC, focusing primarily on CBCT studies [15]. They reported the pooled prevalence rates on 4 continents (Asia, Europe, America, and Africa). However, categorizing into only 4 continents and reporting the prevalence based on such vast continents seems biased. For example, there are different races in East Asia compared to West Asia or North America compared to South America. Moreover, after their study, some new articles in new regions with considerable sample sizes were published; the most prominent one is a very well-designed multinational study with a sample size of 12,608 teeth [16].
Thus, this study aimed to perform a systematic review of the literature and meta-analysis to evaluate the prevalence of MMC in permanent mandibular molars of different populations based on CBCT studies.
Material and methods
This systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA) [17]. The protocol of this review was registered in PROSPERO under the code number CRD42022375405.
Eligibility criteria
Studies using CBCT to evaluate MMC prevalence in human permanent mandibular molars, except third molars, with completely developed apices, and without previous endodontic treatment, were included. Moreover, only studies using voxel sizes equal to or below 200 μm were included [4]. In vitro studies were excluded. No language limitation was applied. Review articles, case reports, surveys, comment letters, book chapters, and conference abstracts were excluded.
Information sources
PubMed, Scopus, Embase, and Web of Science were searched with specific search terms up to the 1st of October 2023. Two separate reviewers performed the screening process for studies evaluating the prevalence and morphology of MMC in permanent human mandibular molars using CBCT. In addition, a gray literature search was conducted in Open-Grey (opengrey.org) and Google Scholar. Finally, three peer-reviewed endodontic journals (International Endodontic Journal, Journal of Endodontics, and Australian Endodontic Journal) and the references of the included studies were manually searched to identify relevant literature. Possible relevant articles were investigated during the screening process by considering references and citations from included studies and relevant published reviews. When necessary, authors were contacted to request unavailable data or analyses.
Search strategy
The search syntax was developed with the direct supervision of two expert endodontists. First, keywords such as “mid mesial canal,” “root canal morphology,” “molar,” “mandibular molar,” “posterior teeth,” “cone-beam computed tomography,” “CBCT,” and “prevalence” were used to construct the main body of the syntax. Synonyms, Boolean operators, field tags, and MeSH terms (if applicable) were added in the following steps to finalize the syntax. The search terms and filters used to search PubMed (MEDLINE and PMC) to identify relevant studies are shown in Supplementary Table S1. (By searching other databases with similar syntax and adapting them to match the operators of each database, we have maximized the effectiveness of our search.)
Studies selection process
Titles and abstracts of the articles were screened according to reviewers’ predefined inclusion and exclusion criteria, and “relevant” articles were subjected to full-text screening by two separate reviewers. Discussion with a senior endodontist resolved any disagreements between the two reviewers.
Data collection and data items
Data extraction was summarized using Microsoft Excel (Microsoft, Redmond, WA), and two independent reviewers collected the data independently. Afterward, disagreements were resolved through discussion among the reviewers. The data extraction form contained the following details: study title, author/year, sample size, tooth type, age, gender, and geographic location. In addition, CBCT parameters such as machine brand and voxel size used in that particular study were also tabulated.
To extract the number of MMCs, we considered MMC as
-
1)
an extra canal between mesiobuccal (MB) and mesiolingual (ML) canals [10] or
-
2)
any specific modifications of root canal classifications with three or more root canals in a single root [18]. For example, Vertucci’s type VIII [5], additional modifications of Vertucci’s canal types introduced by Gulabivala et al. (except type X) [19], all types of Pomeranz et al. classification [6], Sert and Bayirli classification types VIII to XXIII (except type XIX) [20], and Kartal’s type VI and VII [21].
Variables were extracted into two main categories. The first category included demographic characteristics such as the author’s name, study year, and location. The second category comprised the total number of studied teeth, the prevalence of MMC, and tooth type (mandibular 1st or 2nd molar).
Risk of bias assessment
Risk of bias assessment of the included articles was performed using the Joanna Briggs Institute (JBI) critical appraisal tool for prevalence data [22]. Two evaluators independently assessed eligible studies and scored each JBI question as “yes”, “no”, or “unclear”. Discrepancies in the assessment were discussed with senior team members until a consensus was reached. The final score of each article subjected to the JBI appraisal was calculated based on the percentage of positive answers (“yes”). In addition, it was classified as having a “high” risk of bias when the score was <50%, a “moderate” risk of bias if the score ranged from 50% to <70%, and a “low” risk of bias if the score was >70%.
Synthesis methods
The DerSimonian-Laird bivariate random-effects model analysis was performed with STATA software version 16 (StataCorp, College Station, TX) with the “metaprop” package written by VN Nyaga [23]. In addition, the Freeman-Tukey Double Arcsine Transformation method was used to stabilize the variances by studying confidence intervals for analyzing studies involving a small sample size and proportions value that were too high (towards 1) or low (towards 0).
Results
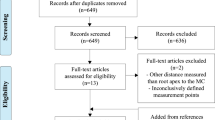
A total of 1165 articles were obtained from the electronic database search, gray literature, and hand searching. After applying the eligibility criteria and eliminating duplicates, 88 articles were selected for full-text assessment. Following the reading of the full-texts, 54 studies were excluded. Thus, 34 studies that fulfilled the eligibility criteria were included for quality assessment and quantitative synthesis (Fig. 1 & Supplementary Table S2).
Included studies characteristics
A total of 34 studies reporting the prevalence of MMC in mandibular molars were included in the meta-analysis from 27 countries and seven geographical regions reporting data from 32,793 studied teeth (Tables 1 and 2).
Prevalence of MMC in mandibular 1st and 2nd molars
The cumulative prevalence of MMC in both mandibular 1st and 2nd molars is 3.11% (95% CI: 2.00-4.44%). The subgroup analysis reveals a prevalence of 4.15% (95% CI: 2.69-5.89%) for 1st molars and 1.2% (95% CI: 0.2-2.83%) for 2nd molars (Fig. 2). The highest prevalence of MMC in mandibular 1st molars was reported by Iqbal et al. as 29.72% [33] (Fig. 3).
In mandibular 2nd molars, the highest reported prevalence of MMC was in the studies of Inaty et al. [18] and Iqbal et al. [33], which was 16%. However, most studies reported no MMC in mandibular 2nd molars (Fig. 4).
Prevalence of MMC in mandibular molars by geographical region
The included studies reported a prevalence of MMC in mandibular 1st and 2nd molars were categorized into seven geographical regions as follows:
a) South Asia: India and Pakistan; b) West Asia: Iran, Saudi Arabia, Jordan, Kazakhstan, Turkey, Yemen, and Lebanon; c) East Asia: China, Korea, Thailand, Malaysia; d) Africa: Morocco, Egypt, Libya, South Africa, Egypt; e) Europe: Croatia, Germany, Poland, Portugal, Greece, Portugal, Spain, Serbia, Greece, Portugal, Spain, and Serbia; f) North America: USA; and g) South America: Brazil and Venezuela.
According to the subgroup meta-analysis, the highest prevalence of MMC in mandibular 1st molar is attributed to North America with 26.32% (95% CI: 13-22%) [10]. However, this result is from a single study. South Asia followed with 11.24% (95% CI: 5.82-18.11%), and Africa with 6.61% (95% CI: 0.23-20.32%), demonstrating the highest prevalence of MMC in mandibular 1st molars than other regions (Fig. 3). Also, the details of the prevalence of MMC in the mandibular 2nd molar are shown in Fig. 4. The prevalence of MMC in mandibular 1st molars in different countries is depicted in a world map (Fig. 5).
Studies quality assessment
A risk-of-bias assessment is provided in detail for each included study in Supplementary Figure S1. Low bias levels were attributed to 94.1% of studies, and moderate bias levels were attributed to 5.9% of studies. In addition, an overall quality assessment is provided in Supplementary Figure S2.
Discussion
In the present study, the worldwide prevalence of MMC in the mandibular 1st molar was 4.15%. However, the presence of MMC varies in different geographical regions and ranges from 0 to 29.7%. Except for the prevalence of MMC in the United States of America, which was based on only a single study (26%), the highest prevalence of MMC in the mandibular 1st molar was found in South Asia (11.24%), followed by Africa (6.61%).
According to the results of the present study, a cumulative prevalence of 1.2% was found for the occurrence of MMC in the mandibular 2nd molars. The highest prevalence of MMC in the mandibular 2nd molar was found in the South Asia (3.97%) and the West Asia (3.56%).
In the present study, for the first time, the cumulative prevalence of MMC is reported by different countries (Fig. 5). Moreover, the prevalence of MMC is reported separately in different regions and continents of the world. Before our study, a systematic review assessed the prevalence of MMC [8]. However, their study had some limitations; for instance, the studies varied in methodology, and voxel sizes of more than 200 μm were included, which is unsuitable for detecting root canal anatomy [55]. Moreover, there was no mention of whether the studies excluded endodontically treated teeth [8]. These differences might depict why the prevalence range of MMCs varied in their study (0.26-53.8%) compared to ours (0-29.7%). Recently, Al-Maswary et al. published a meta-analysis on the global prevalence of MMC focused primarily on CBCT studies [15]. They reported the global prevalence of MMC to be 4.4% in the 1st molar and 1.3% in the 2nd molar, which was in accordance with the results of our study. However, they reported the pooled prevalence rates based on only 4 continents (Asia, Europe, America, and Africa). The racial discrepancy cannot be applied in such a classification based on the vast extent of the continents. For instance, there are different races in East Asia compared to West Asia or North America compared to South America. Therefore, in our study, the regions were classified more precisely including more number of regions but with less extent, including South Asia, West Asia, East Asia, Africa, Europe, North America, and South America. By doing this, the racial bias can be controlled. Compared to the study of Al-Maswary et al., we reported the pooled prevalence rates based on countries wherever possible; therefore, clinicians can find the prevalence of MMC in their country (Fig. 5). More importantly, based on the studies that were published after the study of Al-Maswary, we were able to include another 11,820 samples from new countries, including Saudi Arabia, Egypt, Germany, Croatia, Jordan, Kazakhstan, Libya, Malaysia, Poland, and Turkey.
A well-designed multinational cross-sectional study on the prevalence of MMC with a sample size of 12,608 reported a range of 1-23% [16]. In their study, the prevalence of MMC was 7% for the mandibular 1st molar, which is more than the results of our study. The greater prevalence can be because their study does not include countries from East Asia, North America, and South America [16].
One of the limitations of our study is that regional prevalence cannot necessarily imply ethnic diversities [4]. A geographic region can have multiple ethnic origins, as many countries are a mix of ethnicities. For example, in the study by Pan et al. performed in Malaysia, the majority were Chinese (92.3%), followed by Indians (4.3%), Malays (2.4%), and other races (1.0%) [56]. Furthermore, the root canal anatomy of teeth may vary with sex and age [4]. In our study, the gender and age of the studied population could not be analyzed due to variations in measurements and frequently missed data. However, in general, the studies that focused only on the prevalence of the MMC canal did not find any difference in gender [10, 16, 30, 57].
As mentioned above, no meta-analysis was performed on age and its relation with the prevalence of MMC because of the insufficient data and heterogeneity of the most included studies regarding age. However, some studies reported that the prevalence of identifiable MMC decreases as age increases [8, 46]. Therefore, the prevalence of identifiable MMC could be related to secondary dentin deposition [58]. In contrast, Tahmasbi et al. [10] found the highest prevalence of MMC in the 41-60 age group, and Srivastava et al. [57] found the highest prevalence of MMC in the 31-50 age group. The contrast in findings could also be due to the formation of dentin within the isthmus between the MB and the ML canal, where a previously joined canal becomes separated by dentin and thus creates another canal.
It is also essential to differentiate and clarify the meaning of the isthmus and MMC. Bansal et al. defined an isthmus as a narrow connection between two root canals containing pulp tissue [8]. Pomeranz et al. described MMC as a fin, confluent, or independent canal between the MB and ML canals [6]. However, this definition cannot distinguish between an isthmus and an actual canal [10]. Some have defined a “true MMC” as a clear, round cross-section in the radiographic image between the MB and ML canals, which can be with an isthmus [10, 45]. A systematic review discussed that the inconsistent definition of MMC might be a reason for the wide range of MMC occurrences [8].
Another reason for the diversity of the data in the literature might be the different detection methods to identify MMC. For example, clinical in vivo studies with a DOM can explore negotiable MMCs in non-extracted teeth [11, 12]; however, differentiating a true MMC from an isthmus may not be possible [11], which may account for a higher incidence of MMC in the study of Azim et al. (46%) [11] compared with our study (4.15%).
The voxel size is crucial for detecting root canal system anatomy in CBCT studies. Mirmohammadi et al. has shown that a voxel size of 125 μm has an accuracy of 96% for detecting the second MB canal in maxillary molars [59]. Zhang et al. came to the same conclusion for choosing a voxel size of 125 μm when detecting root canal anatomy of mandibular premolars [60]. Vizzotto et al. reported that a CBCT voxel size of 200 μm had a higher sensibility than larger voxel sizes to detect the second MB canal [55]. Therefore, voxel sizes of more than 200 μm might miss some root canal anatomy. Thus, we excluded the studies that had advocated voxel sizes of more than 200 μm from the present study (Supplementary Figure S1). However, the analysis of the effect of different voxel sizes <200 μm on MMC detection has shown no significant differences [16]. In the study of Hatipoglu et al., the prevalence of MMC was equal (7%) for either voxel sizes ≤150 μm or 150–200 μm [16].
Field of view (FOV) is an important criterion in CBCT imaging. In endodontics, particularly for detecting root canals, a limited FOV CBCT is preferred over medium or large FOV CBCT [61]. This preference is due to the lower radiation dose to the patient, higher spatial resolution, and fewer volumes to interpret. As the FOV size increases, the spatial resolution and image quality decrease, resulting in a higher probability of missing a canal [61]. It should be noted that in morphological studies, CBCT images were not prescribed for endodontic reasons but for general aims such as surgical interventions or evaluation of the surrounding anatomies. Therefore, a medium to high field of view is commonly used, which can lead to underestimation of root canals, such as MMCs. The larger field of view is an inevitable limitation of studies included in the present meta-analysis.
Based on the recommendation of the joint position statement of the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology, a limited FOV CBCT should be considered the imaging modality of choice for initial treatment of teeth with the potential for extra canals and suspected complex morphology [61]. As mentioned before, along with a limited FOV, voxel sizes ≤200 μm should be set for endodontic evaluations [55], such as detecting MMCs.
DOM is another essential aid in nonsurgical and surgical endodontics for locating additional canals [62]. In particular, performing a standardized troughing under high magnification between MB and ML canals is suggested to search for a MMC [11]. To manage the MMC canal during apical surgery of mandibular molars, Pomeranz et al. suggested that after resecting the apex and retro-preparation of the MB and ML canals, to deeply connect the canals to satisfactorily debride and to allow for good retention and sealing of the retrograde filling material [6]. Although the prevalence of MMC was rare in all geographic populations included in this study, the authors suggest always looking for MMC when doing an endodontic treatment on mandibular molars.
A limitation of the present study is that most of the included studies did not include C-shaped and single-rooted teeth in their sample size for estimating the prevalence of MMC; therefore, in only one study [34], to calculate the total number of included teeth, we excluded C-shaped and single-rooted teeth from the original sample size in that study. This procedure was performed to match and adjust their methodology to the other included studies. Although C-shaped and single-rooted molars are rare, excluding such teeth from the study may result in an over-representation of the remaining teeth, leading to an overestimation of the prevalence of MMC. Based on the topic of the present review, only cross-sectional studies could be inserted that, in the hierarchy of evidence, were considered as low level of evidence. However, 94.1% of the included studies had low bias levels.
When interpreting the results of the present study, it is important to consider the limited number of studies available in certain regions. For example, only a single study was conducted on the vast continent of North America [10]. Similarly, countries like Libya and Germany, which are larger than their neighbors, had only one study that met the inclusion criteria for our meta-analysis [16]. The scarcity of studies in these regions may explain the higher prevalence of MMCs compared to their neighboring countries. Among the included studies, only a few countries had two or more studies on the prevalence of MMCs. These countries included China, India, Iran, Pakistan, Yemen, Saudi Arabia, Portugal, and Brazil. Furthermore, there are still many countries for which we were unable to find any data regarding the prevalence of MMCs. Therefore, caution should be employed when generalizing the results of this meta-analysis to each region. It seems that further studies are needed on the prevalence of MMCs in different regions of the world.
For future studies, it is suggested that 1) studies must define their precise definition of a MMC versus isthmus so that it is easier to interpret the data, 2) perform studies on patients over multiple decades of age to determine how age may affect the detectability of MMC, and 3) consider a voxel size equal to or lower than 200 μm.
Conclusion
The prevalence of MMC varies among regions. The MMC prevalence in mandibular 1st molars is 4.15% globally. The mandibular 2nd molar rarely has the MMC (1.2%). Understanding the incidence of MMC can guide clinicians as to whether troughing under high magnification or further investigation with CBCT is indicated when performing endodontic treatment of mandibular molars.
Data availability
No datasets were generated or analysed during the current study.
References
Song M, Kim H, Lee W, Kim E (2011) Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J Endod 37:1516–1519
Karabucak B, Bunes A, Chehoud C, Kohli M, Setzer F (2016) Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: a cone-beam computed tomography study. J Endod 42:538–541
Black G (1897) Descriptive anatomy of the human teeth. SS White Manufacturing Company
Martins J, Marques D, Silva E, Caramês J, Versiani M (2019) Prevalence studies on root canal anatomy using cone-beam computed tomographic imaging: a systematic review. J Endod 45(372-86):e4
Vertucci F (1984) Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 58:589–599
Pomeranz H, Eidelman D, Goldberg M (1981) Treatment considerations of the middle mesial canal of mandibular first and second molars. J Endod 7:565–568
Wayman B, Murata S, Almeida R, Fowler C (1992) A bacteriological and histological evaluation of 58 periapical lesions. J Endod 18:152–155
Bansal R, Hegde S, Astekar M (2018) Morphology and prevalence of middle canals in the mandibular molars: a systematic review. J Oral Maxillofac Pathol 22:216
Borges C, Estrela C, Decurcio DA, Pécora J, Sousa-Neto M, Rossi-Fedele G (2020) Cone-beam and micro-computed tomography for the assessment of root canal morphology: a systematic review. Braz Oral Res 34:e056
Tahmasbi M, Jalali P, Nair M, Barghan S, Nair U (2017) Prevalence of middle mesial canals and isthmi in the mesial root of mandibular molars: an in vivo cone-beam computed tomographic study. J Endod 43:1080–1083
Azim AA, Deutsch AS, Solomon CS (2015) Prevalence of middle mesial canals in mandibular molars after guided troughing under high magnification: an in vivo investigation. J Endod 41:164–168
Nosrat A, Deschenes R, Tordik P, Hicks M, Fouad A (2015) Middle mesial canals in mandibular molars: incidence and related factors. J Endod 41:28–32
Martins JN, Kishen A, Marques D, Silva EJNL, Carames J, Mata A, Versiani MA (2020) Preferred reporting items for epidemiologic cross-sectional studies on root and root canal anatomy using cone-beam computed tomographic technology: a systematized assessment. J Endod 46:915–935
Michetti J, Maret D, Mallet J-P, Diemer F (2010) Validation of cone beam computed tomography as a tool to explore root canal anatomy. J Endod 36:1187–1190
Al-Maswary AA, Almadhoon HW, Elkhateb A, Hamdallah A, Halboub E (2023) The global prevalence of middle mesial canal in mandibular first and second molars assessed by cone beam computed tomography: a systematic review and meta-analysis. J Endod 49:638–656
Hatipoğlu FP, Mağat G, Hatipoğlu Ö, Taha N, Alfirjani S, Abidin IZ, Lehmann AP, Alkhawas M-BAM, Buchanan GD, Kopbayeva M (2023) Assessment of the prevalence of middle mesial canal in mandibular first molar: a multinational cross-sectional study with meta-analysis. J Endod 49:549–558
Moher D, Liberati A, Tetzlaff J, Altman D, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Inaty E, Jabre C, Haddad G, Nehme W, Khalil I, Naaman A, Zogheib C (2020) Anatomical investigation of middle mesial canals of mandibular molars in a Middle Eastern population: a cross-sectional cone-beam computed tomography study. J Contemp Dent Pract 21:910–915
Gulabivala K, Aung T, Alavi A, Ng YL (2001) Root and canal morphology of Burmese mandibular molars. Int Endod J 34:359–370
Sert S, Bayirli G (2004) Evaluation of the root canal configurations of the mandibular and maxillary permanent teeth by gender in the Turkish population. J Endod 30:391–398
Kartal N, Yanıkoğlu F (1992) Root canal morphology of mandibular incisors. J Endod 18:562–564
Institute JB (2017) The Joanna Briggs Institute critical appraisal tools for use in JBI systematic reviews: checklist for prevalence studies. The University of Adelaide: The Joanna Briggs Institute
Nyaga V, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72:1–10
Almeida JC, Candemil AP, Bertolini GR, Souza-Gabriel AE, Cruz-Filho AM, Sousa-Neto MD, Silva RG (2023) Cone-beam computed tomographic evaluation of the root canal anatomy of the lower premolars and molars in a Brazilian sub-population. Imaging Sci Dent 53:77–82
Alroomy R, Elbaz F, Asiri A, Almulhim B, Kumari M, Gunaranjan T, Mashyakhy M, Okazaki K (2022) Assessment of the middle mesial canals of mandibular first molars using cone-beam computed tomography: an in vivo study. Eur Rev Med Pharmacol Sci 26:2861–2866. https://doi.org/10.26355/eurrev_202204_28616
Arayasantiparb R, Wanichwetin W, Banomyoug D (2017) Prevalence and morphology of middle mesial canals in a group of Thai permanent mandibular molars from cone-beam computed tomography images. M Dent J 37:281–287
Bhatti UA, Muhammad M, Javed MQ, Sajid M (2022) Frequency of middle mesial canal in mandibular first molars and its association with various anatomic variables. Aust Endod J 48:494–500
Caputo BV, Noro Filho GA, de Andrade Salgado DM, Moura-Netto C, Giovani EM, Costa C (2016) Evaluation of the root canal morphology of molars by using cone-beam computed tomography in a Brazilian population: part I. J Endod 42:1604–1607. https://doi.org/10.1016/j.joen.2016.07.026
Drouri S, Dhaimy S, Benkiran I, Jabri M, Al Jalil Z, Hamza M (2022) Root and canal morphology of mandibular first molars in a Moroccan subpopulation by cone-beam computed tomography and its international comparison: a cross-sectional study. J Int Oral Health 14:94–100
Hasheminia M, Razavian H, Khorrami L, Mosleh H, Mohamadi S (2021) Prevalence of middle mesial canal in mandibular first molars using cone-beam computed tomography technique. Dent Res J 18:42
Hosseini S, Soleymani A, Moudi E, Bagheri T, Gholinia H (2020) Frequency of middle mesial canal and radix entomolaris in mandibular first molars by cone beam computed tomography in a selected Iranian population. Caspian J Dent Res 9:63–70
Hu X, Huang Z, Huang Z, Lei L, Cui M, Zhang X (2019) Presence of isthmi in mandibular mesial roots and associated factors: an in vivo analysis. Surg Radiol Anat 41:815–822
Iqbal S, Kochhar R, Kumari M (2022) Prevalence of middle mesial canal in the Indian subpopulation of Greater Noida and the related variations in the canal anatomy of mandibular molars using cone-beam computed tomography. Endodontology 34:50–54
Kantilieraki E, Delantoni A, Angelopoulos C, Beltes P (2019) Evaluation of root and root canal morphology of mandibular first and second molars in a Greek population: a CBCT study. Eur Endod J 4:62–68. https://doi.org/10.14744/eej.2019.19480
Kim S, Kim B, Woo J, Kim Y (2013) Morphology of mandibular first molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals. J Endod 39:1516–1521. https://doi.org/10.1016/j.joen.2013.08.015
Martins J, Gu Y, Marques D, Francisco H, Caramês J (2018) Differences on the root and root canal morphologies between Asian and white ethnic groups analyzed by cone-beam computed tomography. J Endod 44:1096–1104. https://doi.org/10.1016/j.joen.2018.04.001
Pérez-Heredia M, Ferrer-Luque CM, Bravo M, Castelo-Baz P, Ruíz-Piñón M, Baca P (2017) Cone-beam computed tomographic study of root anatomy and canal configuration of molars in a Spanish population. J Endod 43:1511–1516. https://doi.org/10.1016/j.joen.2017.03.026
Popović M, Živanović S, Vučićević T, Grujović M, Papić M (2020) Cone-beam computed tomography study of tooth root and canal morphology of permanent molars in a Serbian population. Vojnosanit Pregl 77:470–478
Qiao X, Zhu H, Yan Y, Li J, Ren J, Gao Y, Zou L (2020) Prevalence of middle mesial canal and radix entomolaris of mandibular first permanent molars in a Western Chinese population: an in vivo cone-beam computed tomographic study. BMC Oral Health 20:224. https://doi.org/10.1186/s12903-020-01218-z
Rehman U, Siddique SN, Munawar M, Ginai HA (2020) Prevalence of middle mesial canals and isthmi in mandibular molars using cone beam computed tomography. JPDA 29:114–119
Senan EM, Madfa AA, Alhadainy HA (2020) Root and canal configuration of mandibular first molars in a Yemeni population: a cone-beam computed tomography. Eur Endod J 5:10–17. https://doi.org/10.14744/eej.2020.99609
Shakeri F, Azizi H, Razian F, Haghanifar S, Hoshyari N (2019) Prevalence of mid-mesial canal and isthmuses in mandibular first and second molars in an Iranian population. J Res Dent Maxillofac Sci 4:30–34
Silva EJ, Nejaim Y, Silva AV, Haiter-Neto F, Cohenca N (2013) Evaluation of root canal configuration of mandibular molars in a Brazilian population by using cone-beam computed tomography: an in vivo study. J Endod 39:849–852. https://doi.org/10.1016/j.joen.2013.04.030
Wang Y, Zheng QH, Zhou XD, Tang L, Wang Q, Zheng GN, Huang DM (2010) Evaluation of the root and canal morphology of mandibular first permanent molars in a Western Chinese population by cone-beam computed tomography. J Endod 36:1786–1789. https://doi.org/10.1016/j.joen.2010.08.016
Xu S, Dao J, Liu Z, Zhang Z, Lu Y, Zeng X (2020) Cone-beam computed tomography investigation of middle mesial canals and isthmuses in mandibular first molars in a Chinese population. BMC Oral Health 20:135. https://doi.org/10.1186/s12903-020-01126-2
Yang Y, Wu B, Zeng J, Chen M (2020) Classification and morphology of middle mesial canals of mandibular first molars in a southern Chinese subpopulation: a cone-beam computed tomographic study. BMC Oral Health 20:358. https://doi.org/10.1186/s12903-020-01339-5
Zhang R, Wang H, Tian YY, Yu X, Hu T, Dummer PM (2011) Use of cone-beam computed tomography to evaluate root and canal morphology of mandibular molars in Chinese individuals. Int Endod J 44:990–999. https://doi.org/10.1111/j.1365-2591.2011.01904.x
Zhang X, Xiong S, Ma Y, Han T, Chen X, Wan F, Lu Y, Yan S, Wang Y (2015) A cone-beam computed tomographic study on mandibular first molars in a Chinese subpopulation. PLoS One 10:e0134919. https://doi.org/10.1371/journal.pone.0134919
Donyavi Z, Shokri A, Khoshbin E, Khalili M, Faradmal J (2019) Assessment of root canal morphology of maxillary and mandibular second molars in the Iranian population using CBCT. Dent Med Probl 56:45–51. https://doi.org/10.17219/dmp/101783
Gomez F, Brea G, Gomez-Sosa J (2021) Root canal morphology and variations in mandibular second molars: an in vivo cone-beam computed tomography analysis. BMC Oral Health 21:1–7
Kim S, Kim B, Kim Y (2016) Mandibular second molar root canal morphology and variants in a Korean subpopulation. Int Endod J 49:136–144. https://doi.org/10.1111/iej.12437
Pawar AM, Pawar M, Kfir A, Singh S, Salve P, Thakur B, Neelakantan P (2017) Root canal morphology and variations in mandibular second molar teeth of an Indian population: an in vivo cone-beam computed tomography analysis. Clin Oral Investig 21:2801–2809. https://doi.org/10.1007/s00784-017-2082-6
Saber SM, Seoud MA, Sadat SM, Nawar NN (2023) Root and canal morphology of mandibular second molars in an Egyptian subpopulation: a cone-beam computed tomography study. BMC Oral Health 23:217
Senan E, Alhadainy H, Madfa AA (2021) Root and canal morphology of mandibular second molars in a Yemeni population: a cone-beam computed tomography. Eur Endod J 6:72–81. https://doi.org/10.14744/eej.2020.94695
Vizzotto M, Silveira P, Arús N, Montagner F, Gomes B, Silveira H (2013) CBCT for the assessment of second mesiobuccal (MB 2) canals in maxillary molar teeth: effect of voxel size and presence of root filling. Int Endod J 46:870–876
Pan JYY, Parolia A, Chuah SR, Bhatia S, Mutalik S, Pau A (2019) Root canal morphology of permanent teeth in a Malaysian subpopulation using cone-beam computed tomography. BMC Oral Health 19:14. https://doi.org/10.1186/s12903-019-0710-z
Srivastava S, Alrogaibah NA, Aljarbou G (2018) Cone-beam computed tomographic analysis of middle mesial canals and isthmus in mesial roots of mandibular first molars-prevalence and related factors. J Conserv Dent 21:526–530. https://doi.org/10.4103/jcd.Jcd_205_18
Johnstone M, Parashos P (2015) Endodontics and the ageing patient. Aust Dent J 60:20–27
Mirmohammadi H, Mahdi L, Partovi P, Khademi A, Shemesh H, Hassan B (2015) Accuracy of cone-beam computed tomography in the detection of a second mesiobuccal root canal in endodontically treated teeth: an ex vivo study. J Endod 41:1678–1681
Zhang D, Chen J, Lan G, Li M, An J, Wen X, Liu L, Deng M (2017) The root canal morphology in mandibular first premolars: a comparative evaluation of cone-beam computed tomography and micro-computed tomography. Clin Oral Investig 21:1007–1012
Fayad MI, Nair M, Levin MD, Benavides E, Rubinstein RA, Barghan S, Hirschberg CS, Ruprecht A (2015) AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 120:508–512
Yoshioka T, Kobayashi C, Suda H (2002) Detection rate of root canal orifices with a microscope. J Endod 28:452–453
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
Mahmood Reza Kalantar Motamedi: Conceptualization, Methodology, Validation, Writing - Original Draft
Mohammad Hosein Amirzade-Iranaq: Methodology, Validation, Writing - Original Draft, Formal analysis
William N Ha: Methodology, Supervision, Project administration, Writing - Review & Editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable (based on the type of the study). The protocol of this systematic review was registered in PROSPERO under the code number CRD42022375405.
Informed consent
Not applicable (based on the type of the study).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Motamedi, M.R.K., Amirzade-Iranaq, M.H. & Ha, W.N. A systematic review and meta-analysis of the prevalence and global distribution of middle mesial canals in mandibular molars identified by CBCT. Clin Oral Invest 28, 310 (2024). https://doi.org/10.1007/s00784-024-05660-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-024-05660-z