Abstract
Objectives
The purpose of this systematic review was to appraise the existing literature on the effect of hard tissue defects on the clinical outcome of endodontic microsurgery (EMS).
Methods
MEDLINE (PubMed), Embase, Web of Science, Cochrane Library and grey literature were searched from January 2000 to May 2023. Study selection and data extraction were performed in duplicate. Eligible studies were critically appraised for the risk of bias using the Cochrane Risk of bias tool. The quality of evidence was assessed using GRADE. Review Manager (RevMan Computer program Version 5.4, The Cochrane Collaboration, 2020) was utilized and the Mantel Haenszel fixed or random effects model was applied, depending on the heterogeneity of the studies. Meta-analysis was performed to estimate the Risk ratio (RR) and 95% Confidence Interval (CIs) to correlate the effects of these factors on treatment outcomes.
Results
Nineteen studies were included. The EMS overall pooled success rate was 84.5%. Five characteristics of hard tissue were identified. The size of the lesion (Small ≤ 5 mm: 78.4% vs. Large > 5 mm: 63.3%, RR = 1.12, 95% CI 1.00–1.26, P ≤ .05), significantly affected the outcomes of EMS. Endodontic lesions exhibited slightly better outcomes than endodontic-periodontal lesions (81.4% vs. 68.2%, RR = 1.14 95% CI 0.98–1.33, P > .05). Cases with the height of the buccal bone > 3 mm also exhibited slightly better outcomes (91.5% vs. 71.4%, RR = 1.20, 95% CI 0.88–1.62, P > .05). Additionally, through and through lesions exhibited better outcomes when grafting was completed during the EMS procedure both in 2D (RR = 1.12 95% CI 0.97–1.29, P > .05) and 3D evaluation ((RR = 1.28 95% CI 0.69–2.37 P > .05). The overall quality of evidence was graded as low to high.
Conclusion
With a low to high quality of evidence, the size of the lesion is a key prognostic variable that significantly affects the outcome of EMS, as lesions ≤ 5 mm exhibit better outcomes as compared to larger lesions.
Clinical significance
The presence of hard tissue defects can affect the outcome of endodontic microsurgery (EMS). The presented data can aid the clinicians’ decision-making process by examining certain pre-operative prognostic variables, when considering EMS as a treatment option. Clinical cases with more favorable hard tissue characteristics lead to a better prognosis in EMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endodontic microsurgery (EMS) procedures are indicated in previously treated teeth where non-surgical retreatment is not feasible or as an adjunct to non-surgical root canal treatment in teeth with longstanding periapical disease and can also be useful in the diagnosis of pathosis [1]. The primary objective of EMS is to restore the apical periodontium to its functional state [2, 3]. EMS success depends on the absence of clinical symptoms, such as pain, swelling, tenderness to percussion, lack of sinus tracts, and normal, physiologic tooth mobility [4]. Various preoperative and postoperative factors can differ widely in magnitude at different points in time, making it difficult to assess their combined effects on the outcome of treatment [5].
In recent decades, numerous clinical studies have focused on the technical aspects of EMS, particularly on the innovative use of instruments, devices, and filling materials [6]. Subsequently, improvements in techniques, magnification aids, and the use of biocompatible root-end filling materials have made EMS treatment outcomes more predictable [7]. In a meta-analysis, the weighted pooled success rate of EMS was 95% (95% confidence intervals (CI), 0.88–0.98), making it 1.6 times more successful than traditional surgery, which had a weighted pooled success rate of 59% (95% CI, 0.55–0.63) [8].
Following EMS, soft tissue incisions heal mainly by primary intention, whereas bone defects and resected root surfaces heal by secondary intention [9]. The periapical pathosis, bone tomography, lesion size and inadequate bone preparation during osteotomy procedures can, however, affect the quality, quantity, and level of bone destruction, leading to delayed healing and a higher risk of postoperative complications [10]. The characteristics of hard tissues, and their effect on EMS outcomes have not yet been comprehensively analyzed. The presence of multiple unfavorable hard tissue characteristics may lead to a poor EMS prognosis. Sufficient knowledge about the characteristics of hard tissues can aid the clinician in the development of the treatment plan when considering it as a treatment option for the healing of persistent apical pathosis. Therefore, the purpose of this systematic review was to determine whether the presence of hard tissue defects influenced outcome of treatment in patients who had undergone EMS with a minimum one-year follow-up period.
Materials and methods
This systematic review was registered in the PROSPERO database (CRD42021270431) under the universally accepted systematic review process [11]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was used to report our methodology and results [12].
The eligibility and criteria were as follows:
-
Population: Adults with a history of the previously treated teeth with EMS. For the purposes of this review, EMS procedures should include the use of a surgical operating microscope, ultrasonic root-end preparation, and biocompatible root-end filling materials.
-
Exposure: Hard tissue prognostic variables such as the size of lesion, type of lesion (presence of endodontic-periodontal), the use of grafting in through and through lesions (TATL), and the height of the buccal bone plate, during EMS.
-
Outcome (O): The outcomes of EMS in each study were evaluated clinically and/or radiographically, according to Rud et al. [13] and Molven et al. [14] classifications, or modified PENN 3D criteria [15], namely, complete healing (reformation of the lamina dura), incomplete healing (scar tissue), uncertain healing, and unsatisfactory healing. Success was defined as the absence of clinical signs and symptoms (pain, swelling, tenderness to percussion, sinus, and lack of mobility) and evidence of radiographic healing as determined by CBCT or PA (absence of periapical radiolucency). The criteria for failure included any clinical signs and/or symptoms or radiographic evidence of uncertain or unsatisfactory healing. The success of EMS should be measured after a period of at least 12 months.
-
Study design: Randomized controlled trials, prospective and retrospective cohort studies were included. A prospective study design was selected because preoperative factors, outcome assessments, and follow-up examinations can be easily documented and analyzed.
Studies were excluded if they involved the primary dentition, teeth with horizontal or vertical fractures, studies in which the effect of hard tissues on the outcome of EMS was not examined, studies involving other surgical endodontic procedures (e.g., replantation, hemisection, root amputation), studies with inconsistent designs, non-endodontic microsurgical procedures, outdated retrograde materials (i.e. amalgam), studies with < 12 months follow-up periods, studies conducted on animal, ex vivo or in vitro studies, as well as review articles, letters, and opinion articles were also excluded.
Search methods for identification of studies
Three independent reviewers were involved in determining the search terms (P.K., M.S., and M.S.I) in consultation with the librarian. Four major electronic databases were used: MEDLINE (PubMed), Embase, Web of Science and the Cochrane Library up to March 2023, for English language studies. (Table 1 ). Unpublished studies (or grey literature, such as technical reports or dissertations) through Google Scholar™ (Google, Mountain View, CA, USA) and ProQuest (Ann Harbor, Michigan, USA) (the first 100 hits) were also included. A reference list of previous reviews of the same topic, including studies and major textbooks [4, 5] was also manually searched. All identified records were retrieved and imported into bibliographic software (Zotero 5.0.83 version). Duplicate records were removed.
Screening and data extraction
Two reviewers (P.K, M.S.I) independently reviewed and selected eligible studies from the searches and extracted the data. The disagreements were resolved by consulting a third reviewer (M.S), who reviewed the selection of studies and data extraction. The information outlined in Table 2 was extracted from each study to verify the inclusion criteria. The data from the included studies were entered into a standardized Excel (Microsoft, Richmond, WA, USA). Reasons for exclusion at the full-text stage were recorded (Table 3 ). The following data from each study was extracted:
-
General characteristics of the study (author, year, title, type of study design)
-
Detailed information about the participants, including preoperative pulpal and periapical diagnosis.
-
A description of the exposure status and the number of subjects assigned to each prognostic factor of interest (lesion size, lesion type, height of buccal bone plate, and the duration of the follow-up visits)
-
A description of the methods used to assess the outcomes.
Two independent reviewers (P.K and M.S.I) independently verified the accuracy of data extraction. The corresponding authors of all eligible studies were contacted when in doubt about the procedure, methodology, or material of the studies.
Risk of bias assessment
Two authors (M.S.I and P.K) independently used the Cochrane risk of bias tool [16] to evaluate the included randomized controlled trials across 7 domains: random sequence generalization, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. For retrospective and prospective studies, the items “random sequence generation”, “allocation concealment” and “blinding of participants and personnel” were rated as not applicable. Disagreements were resolved by consulting a third reviewer (M.S). A determination of low risk in all domains of a study rendered it as a “low risk” of bias, some concerns or unclear risk of bias in at least 1 domain classified the study as having “some concerns,” and some concerns in 3 or more domains or high risk in at least 1 domain rendered the study as “high risk.”
Quality of the evidence
The Grading of Recommendations, Assessment, Development and Evaluation (GRADEpro GDT: GRADEpro Guideline Development Tool; McMaster University, Hamilton, ON, Canada) was used to objectively rate the quality of outcome analyses for the prospective and retrospective cohort studies. Two reviewers (P.K and M.S.I) assessed five categories: the risk of bias, inconsistent results, indirectness of the evidence, imprecision, and publication bias. (Table 3 ) An overall judgment of high, moderate, low, or very low confidence was given to each result [17]. Consensus was reached by consulting a third reviewer (M.S).
Quantitative analyses
For each intervention, data was summarized, based on the outcomes associated with those teeth with or without the respective hard tissue characteristics. Based on the potential predictors, we stratified the subgroup analysis for the outcome of EMS during the follow-up period to further assess the following hard tissue characteristics: size and type of lesion, height of the buccal bone, and effect of grafting on outcome when through and through lesions were present. Review Manager (RevMan Computer program Version 5.4, The Cochrane Collaboration, 2020) [18] was utilized. Statistical heterogeneity was evaluated using the I2 statistic, with 25% equating low heterogeneity, 50% equating medium heterogeneity, and 75% equating high heterogeneity [16]. The Mantel Haenszel fixed-effects model of analysis was applied if the I2 was < 50% otherwise, a random-effects model of analysis was used [19, 20]. The meta-analysis used risk ratio (RR) and 95% CI to estimate outcome. Sensitivity analyses were performed to evaluate the influence of studies with a high risk of bias. For all test results, P ≤ 0.05 was considered significant.
Results
Search results
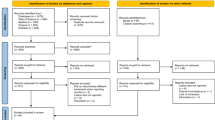
From the initial search of 536 records, 296 duplicates were removed. The titles and abstracts of 240 records were screened. A total of 51 records were retrieved, and finally, 19 studies met our inclusion criteria [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] (Fig. 1). The reasons for exclusion can be found in the Supplementary Table.
Descriptive results
The included studies (Table 2 ) were conducted in various locations. There were a total of 3,506 cases of EMS included. The decision to perform EMS was confirmed by the presence of either a radiographic apical radiolucency and/or clinical symptoms such as pain, tenderness to percussion, infection, and swelling of the buccal mucosa [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
Risk of bias
The results of the Cochrane Risk of Bias tool (RoB 2) is presented in Fig. 2. No included study was judged to exhibit a high risk of bias.
Quality of evidence
The overall certainty of evidence across studies was rated as low to high. Due to the variation, this indicates that our confidence in the estimate of the effect is limited. Therefore, the true effect may be substantially different from the estimate of the effect. (Table 3).
Quantitative analyses
The overall pooled success rate of EMS from the 18 included studies is 84.5%. Meta-analysis was performed on each of the hard tissue characteristics (Fig. 3). The impact of the following hard tissue characteristics on the success of EMS outcome was investigated:
-
Lesion size:
-
o
In seven studies [21,22,23,24,25,26,27], lesion size was measured by periapical radiographs and characterized as small (≤ 5 mm) or large lesions (> 5 mm). The pooled result of 1078 cases revealed that small lesions (≤ 5 mm) exhibited significantly better outcome of healing compared to large lesions (> 5 mm); (78.4% vs. 63.3%, RR = 1.12, 95% CI 1.00–1.26, P ≤ 0.05). Medium heterogeneity was observed (I2 = 58%).
-
o
-
Lesion type:
-
o
In five studies [28,29,30,31,32], the lesion type was dichotomized as endodontic vs. endodontic-periodontal lesion. The pooled result of 1,625 cases revealed that endodontic lesions exhibited slightly better outcomes of healing compared to the Endodontic-Periodontal lesion: (81.4% vs. 68.2%, RR = 1.14 95% CI 0.98–1.33, P > 0.05). A medium level of heterogeneity (I2 = 66%) was observed.
-
o
-
Through and through lesions:
-
o
In five studies [33,34,35,36,37], the outcome of through and through lesions was dichotomized, based on if grafting was used during the EMS procedure. The pooled result of 135 cases examined the result of EMS in the presence of through and through lesions and compared groups based on whether or not a graft was placed during the procedure. All the studies assessed the result using conventional PA radiography, but only two studies [35, 36] used CBCT as an adjunct. Both the 2D evaluation (RR = 1.12 95% CI 0.97–1.29, P > 0.05) and the 3D evaluation (RR = 1.28 95% CI 0.69–2.37 P > 0.05) showed that there were slightly better outcomes when a graft was utilized. There was no heterogeneity between the five studies, but a high level of heterogeneity was observed in the two 3D analysis studies (I2 = 77%).
-
o
-
Height of Buccal Bone:
-
o
In two studies [38, 39], the height of buccal bone was dichotomized as ≤ 3 mm vs. > 3 mm. The pooled result of 232 cases revealed that those with a longer buccal bone height (> 3 mm) had slightly better outcomes compared to those with a shorter buccal bone height (≤ 3 mm); (91.4% vs. 71.4%, RR = 0.84, 95% CI 0.62–1.14, P > 0.05). A medium-level heterogeneity was observed (I2 = 70%).
-
o
Discussion
In this study, we assessed the effects of hard tissue defects on the outcome of EMS. With a low to moderate certainty, this systematic review and meta-analysis showed that the size of the lesion can significantly impact the healing outcomes of EMS. No major treatment-related concerns were reported in the included studies.
The success of EMS can be influenced by patient-related, tooth-related, and treatment-related factors [8]. In terms of tooth-related factors, the outcome of EMS can vary depending on the size of the lesion. Similar to previous research studies [8, 24, 40, 41], our study found that the size of the periapical lesion can affect the outcome of EMS. Our results were similar to other studies that assessed lesion size and outcome [24, 40, 41]. A systematic review that evaluated tooth-related prognostic factors when performing EMS found that, at a minimum follow-up period of 12 months, the healing rate was significantly higher for teeth with smaller lesions (≤ 5 mm) than for those with larger lesions (> 5 mm) (OR = 1.82; 95% CI, 1.13–2.92; p = 0.01) [8]. It should be noted that for cases with a large lesion, it is possible that incomplete curettage can cause persistent inflammation due to the presence of residual tissues [42, 43]; hence, larger lesions usually heal more slowly [31]. This pattern was also noted in Lui et al.’s long-term study. They reported that the healing outcome of EMS was 71% at 1- to 2-years after apical surgery. Most healed cases maintained their healed status while those with uncertain healing gradually transitioned to complete healing over long-term follow-up, hence, their overall healing outcome improved to 78.3% at 5- to 9-years after apical surgery. Similarly, a long-term retrospective study [44] reported that EMS had a healing rate of 91.6% after one year and 91.4% after five years. However, these healing rates declined by 10% at 10 years to 81.5%. Therefore, long-term monitoring is needed to assess the outcomes of EMS.
The outcome of endodontic surgery can be influenced by the presence of a periodontal defect. [28, 45, 46]. Clinically, it is possible for a tooth to have endodontic and periodontal lesions that are independent of or communicate with each other. An isolated endodontic lesion typically has a closed wound with sinus tracts and a normal probing depth. A combined lesion may initially appear as an isolated endodontic or periodontal lesion with subsequent involvement of other lesions [47]. Therefore, a complete clinical history and accurate diagnosis are necessary for a successful outcome. Prior studies have shown that lesions that are solely of endodontic origin have a better chance of healing than those with an endodontic-periodontal origin [28,29,30]. Although statistically insignificant, our study confirmed this by demonstrating that the healing and outcome of EMS is better when lesions are solely of endodontic origin.
When considering periapical lesions and resorption of marginal bone, it is recommended that the buccal bone plate height be at least 3 mm [48]. In our study, although teeth with a longer height of buccal bone (> 3 mm) had better healing outcomes in EMS than those with a shorter height of buccal bone (≤ 3 mm), this difference did not significantly affect the outcome. This is most likely due to the wide variation in the sample sizes for the included studies, which leads to heterogeneous results [31, 39]. Alternatively, it could also be because the measurements were taken at a different time, specifically before and after the surgery. According to Kim et al. [39] the height of the buccal bone was measured preoperatively, but Song et al.[31] measured the height of the buccal bone postoperatively, which decreases after the ostectomy, leading to a difference in measurements.
Moreover, through and through lesions (TATL) present a unique clinical challenge, as the healing often results in periapical scarring, due to the growth of connective tissue into the defect [49]. Our study demonstrated that through and through lesions may have a slightly better outcome when a graft is placed. However, this result was statistically insignificant and there may be very little difference in healing of TATL, regardless of graft status at surgery.
There are some limitations to our systematic review. In terms of the risk of bias, the Cochrane Risk of Bias tool (Table 3) raised some concerns about performance and detection bias. As our included studies are a mix of prospective cohorts, retrospective cohorts, and randomized controlled trials, the differences in interventions and baseline characteristics may cause biases and discrepancies in the overall measurement. Our pooled analyses were based on a relatively wide range of subjects. The included studies primarily compared different hard tissue defects instead of evaluating the outcome of an individual defect, which negatively affected the domain of “overall certainty of evidence” of the quality assessment. Very low to low certainty indicates a potential discrepancy between the estimated and true outcomes. It is important to note that not all of the included studies reported long-term outcomes. Studies with short-term follow-up fail to account for the possibility of outcome relapse, and those that incorrectly classify incomplete healing outcomes as 'success' may inflate the actual success rate. Despite these limitations, our study has several strengths. We used a comprehensive search methodology with a strict inclusion criterion to maximize the amount of evidence. In addition, we analyzed the hard tissue defects and outcomes of EMS and used subgroup and sensitivity analyses to estimate the treatment effects.
Although endodontic research has increased, most studies report inconsistent measurements and outcomes. It is important to document relevant data consistently so that knowledge synthesis can occur over time, allowing healthcare providers to integrate their clinical expertise with the latest clinical research findings. To improve the reliability of endodontic outcome studies, the use of a reporting checklist [e.g. a 19-domain reporting checklist by Azarpazhooh et al. [50]] can address biases, unexplained heterogeneity, inconsistencies, indirectness, and imprecisions in overall quality assessment. It is important for future research studies to use this checklist as a guideline to ensure accuracy of the success rate in terms of EMS outcome. Larger sample sizes with minimal pre-operative confounders may also aid in obtaining a reliable outcome. Studies should document relevant data consistently so that knowledge synthesis can occur over time, allowing healthcare providers to integrate their clinical expertise with the latest clinical research findings. This will aid clinicians in the decision making process when considering EMS as a treatment option, specifically when there may be multiple hard tissue defects present pre-operatively.
Conclusion
While many hard tissue characteristics were analyzed in this review, the results indicate that with a low to high quality of evidence, the size of the lesion appears to significantly influence the healing outcomes of EMS, with lesions ≤ 5 mm having a significantly better outcome than larger lesions. Additional hard tissue characteristics, such as the height of buccal bone < 3 mm, presence of a combined endodontic-periodontal lesion, and presence of through and through lesions, may also influence the outcome of EMS, but these results were statistically insignificant.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ng YL, Mann V, Gulabivala K (2008) Outcome of secondary root canal treatment: A systematic review of the literature. Int Endod J 41:1026–1046
Ng YL, Mann V, Gulabivala K (2010) Tooth survival following non-surgical root canal treatment: A systematic review of the literature. Int Endod J 43:171–189
Ng YL, Mann V, Gulabivala K (2011) A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2: Tooth survival. Int Endod J 44:610–625
Rotstein I, Ingle JI (2019) Ingle’s endodontics, 7th edn. PMPA USA, Raleigh
Hargreaves KM, Berman LH, Rotstein I et al (2021) Cohen’s pathways of the pulp, 12th edn. Elsevier, St. Louis, p 2
Abbott P (2012) Endodontics - Current and future. J Conserv Dent 15:202–205
Elemam RF, Pretty I (2011) Comparison of the success rate of endodontic treatment and implant treatment. ISRN Dent 2011:1–8
von Arx T, Peñarrocha M, Jensen S (2010) Prognostic factors in apical surgery with root-end filling: a meta-analysis. J Endod 36:957–973
Harrison JW, Jurosky KA (1992) Wound healing in the tissues of the periodontium following periradicular surgery. III. The osseous excisional wound. J Endod 18(2):76–81. https://doi.org/10.1016/S0099-2399(06)81375-
Kang M, In JH, Song M et al (2015) Outcome of nonsurgical retreatment and EMS: a meta-analysis. Clin Oral Invest 19:569–582
Page MJ, Moher D, Bossuyt PM et al (2021) PRISMA (2020) explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:1–36
Shamseer L, Moher D, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350:1–20
Rud J, Andreasen JO, Jensen JE (1972) Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg 1:195–214
Molven O, Halse A, Grung B (1991) Surgical management of endodontic failures: indications and treatment results. Int Dent J 41:33–42
Schloss T, Sonntag D, Kohli MR, Setzer FC (2017) A comparison of 2- and 3-dimensional healing assessment after endodontic surgery using cone-beam computed tomographic volumes or periapical radiographs. J Endod 43:1072–1079
Higgins JP, Altman DG (2008) Assessing risk of bias in included studies. Cochrane Book Series. Wiley-Blackwell, Hoboken, NJ, pp 187–241
GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2022. https://www.gradepro.org/.
Cumpston M, Li T, Page MJ et al (2019) Updated guidance for trusted systematic reviews: a newedition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev 10:ED000142
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45:139–145
Higgins JPT, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
von Arx T, Jensen SS, Hänni S et al (2021) Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod 38:570–9
von Arx T, Jensen SS, Hänni S (2007) Clinical and radiographic assessment of various predictors for healing outcome 1 year after periapical surgery. J Endod 33:123–128
Liao WC, Lee YL, Tsai YL et al (2019) Outcome assessment of apical surgery: A study of 234 teeth. J Formos Med Assoc 118:1055–1061
Huang S, Chen NN, Yu VSH et al (2020) Long-term success and survival of EMS. J Endod 46:149–157
Pallarés-Serrano A, Glera-Suarez P, Tarazona-Alvarez B et al (2021) Prognostic factors after EMS: a retrospective study of 111 cases with 5 to 9 years of follow-up. J Endod 47:397–403
Yoo YJ, Kim DW, Perinpanayagam H et al (2020) Prognostic factors of long-term outcomes in EMS: a retrospective cohort study over five years. J Clin Med 9:1–13
Caliskan MK et al (2016) The outcome of apical microsurgery using MTA as the root-end filling material: 2- to 6-year follow-up study. Int Endod J 45:245–254
Kim E, Song JS, Jung IY et al (2008) Prospective clinical study evaluating EMS outcomes for cases with lesions of endodontic origin compared with cases with lesions of combined periodontal-endodontic origin. J Endod 34:546–551
Song M, Chung W, Lee SJ et al (2012) Long-term outcome of the cases classified as successes based on short-term follow-up in EMS. J Endod 38:1192–1196
Song M et al (2011) Prognostic Factors for Clinical Outcomes in Endodontic Microsurgery: A Retrospective Study. J Endod 37:927–933
Song M et al (2013) Prognostic Factors of Clinical Outcomes in Endodontic Microsurgery: A Prospective Study. J Endo 39(12):1491–1497
Lai PT, Wu SL, Huang CY, Yang SF (2022) A retrospective cohort study on outcome and interactions among prognostic factors of endodontic microsurgery. J Formos Med Assoc 121(11):2220–2226. https://doi.org/10.1016/j.jfma.2022.04.005
Pecora G, De Leonardis D, Ibrahim N, Bovi M, Cornelini R (2001) The use of calcium sulphate in the surgical treatment of a “through and through” periradicular lesion. Int Endod J 34(3):189–197
Taschieri S, Del Fabbro M, Testori T, Saita M, Weinstein R (2008) Efficacy of guided tissue regeneration in the management of through-and-through lesions following surgical endodontics: a preliminary study. Int J Periodontics and Restorative Dentistry 28:264–271
Taschieri S, Del Fabbro M, Testori T, Weinstein R (2007) Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg 65(6):1121–1127
Parmar PD, Dhamija R, Tewari S, Sangwan P, Gupta A, Duhan J, Mittal S (2019) 2D and 3D radiographic outcome assessment of the effect of guided tissue regeneration using resorbable collagen membrane in the healing of through-and-through periapical lesions - a randomized controlled trial. Int Endod J 52(7):935–948. https://doi.org/10.1111/iej.13098. (Erratum in: Int Endod J. ;52(10):1529)
Dhamija R, Tewari S, Sangwan P, Duhan J, Mittal S (2020) Impact of Platelet-rich Plasma in the Healing of Through-and-through Periapical Lesions Using 2-dimensional and 3-dimensional Evaluation: A Randomized Controlled Trial. J Endod 46(9):1167–1184. https://doi.org/10.1016/j.joen.2020.06.004. (Erratum in: J Endod.;47(2):336-338)
Song M, Kim SG, Shin SJ, Kim HC, Kim E (2013) The influence of bone tissue deficiency on the outcome of endodontic microsurgery: a prospective study. J Endod 39(11):1341–1345
Kim D, Ku H, Nam T et al (2016) Influence of size and volume of periapical lesions on the outcome of EMS: 3-dimensional analysis using cone-beam computed tomography. J Endod 42:1196–1201
Serrano-Giménez M, Sánchez-Torres A, Gay-Escoda C (2015) Prognostic factors on periapical surgery: A systematic review. Med Oral Patol Oral Cir Bucal 20:e715–e722
Lui JN, Khin MM, Krishnaswamy G et al (2014) Prognostic factors relating to the outcome of EMS. J Endod 40:1071–1076
Çalışkan MK, Kaval ME, Tekin U et al (2016) Radiographic and histological evaluation of persistent periapical lesions associated with endodontic failures after apical microsurgery. Int Endod J 49:1011–1019
Pitcher B, Alaqla A, Noujeim M et al (2017) Binary decision trees for preoperative periapical cyst screening using cone-beam computed tomography. J Endod 43:383–388
von Arx T, Jensen SS, Janner SFM, Hänni S, Bornstein MM (2019) A 10-year Follow-up Study of 119 Teeth Treated with Apical Surgery and Root-end Filling with Mineral Trioxide Aggregate. J Endod 45:394–401
Hirsch JM, Ahlstrom U, Henrikson PA et al (1979) Periapical surgery. Int J Oral Surg 8:173–185
Jansson L, Sandstedt P, Laftman AC et al (1997) Relationship between apical and marginal healing in periradicular surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:596601
Youngjune J, Taek HH, Jae CH et al (2015) Influence of apical root resection on the biomechanical response of a single-rooted tooth-part 2: apical root resection combined with periodontal bone loss. J Endod 41:412–416
Harrison JW, Jurosky KA (1991) Wound healing in the tissues of the periodontium following periradicular surgery. 2. The dissectional wound. J Endod 17:544–52
Dahlin C, Linde A, Gottlow J, Nyman S (1988) Healing of bone defects by guided tissue regeneration. Plast Reconstr Surg 81(5):672–676. https://doi.org/10.1097/00006534-198805000-00004
Azarpazhooh A, Khazaei S, Jafarzadeh H et al (2022) A Scoping Review of Four Decades of Outcomes in Nonsurgical Root Canal Treatment, Nonsurgical Retreatment, and Apexification Studies: Part 3-A Proposed Framework for Standardized Data Collection and Reporting of Endodontic Outcome Studies. J Endod 48:40–54
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
All authors have been involved in the work leading to the publication of the paper and have read and approved this final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sabeti, M., Ihsan, M.S., Kharat, P. et al. The effect of hard tissue defects on the clinical outcome of endodontic microsurgery: a systematic review and meta-analysis. Clin Oral Invest 27, 7079–7089 (2023). https://doi.org/10.1007/s00784-023-05341-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05341-3