Abstract
Objectives
To study the effects of one or two repeated subgingival instrumentations (RSI) in achieving the endpoints of therapy (EoT) in open pockets [residual probing pocket depth (PPD) ≥ 6 mm and PPD 4–5 mm with bleeding on probing (BoP)] after steps I-II of therapy.
Materials and methods
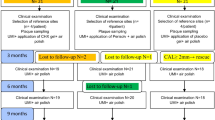
Twenty-five patients (3,552 total sites; 1,450 open pockets) with stage III-IV periodontitis received steps I-II of periodontal therapy and were re-evaluated after 4–6 weeks (T1). Residual pockets received RSI at T1 and at 3 months (T2). EoT (PPD < 4 or PPD < 6 BoP-) rate at T1, T2 and 6 months (T3) was computed. The number of needed surgeries and treatment costs were calculated.
Results
At T1, 67.6% of open pockets achieved EoT. At residual PPD ≥ 6 mm at T1 (n = 172), one and two RSI resulted in 33.1% and 45.9% of EoT at T2 and T3, respectively. At residual PPD 4–5 mm with BoP at T1 (n = 298), one and two RSI resulted in 66.8% and 72.1% of EoT at T2 and T3, respectively. PPD at T1 predicted EoT after RSI in both cases, while tooth type only in residual PPD 4–5 mm BoP + . At T1, mean number of surgeries per patient and associated costs were significantly higher than after one/two RSI.
Conclusions
RSI may achieve EoT in residual PPD 4–5 mm BoP + and PPD ≥ 6 mm in a considerable number of cases.
Clinical relevance
These findings may support the administration of one/two cycles of RSI prior to surgical approach.
Protocol registration
ClinicalTrials.gov identification number: NCT04826926.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontitis represents one of the most common non-communicable diseases of humankind [1], with detrimental effects on both tooth-supporting structures and general health [2,3,4,5]. In late 2019, the European Federation of Periodontology (EFP) S3 level clinical practice guideline for the treatment of stage I-III periodontitis was approved by an international consensus of experts [6]. This guideline recommends a stepwise approach involving a first step aimed at controlling local and systemic risk factors, followed by a second step aimed at removing the subgingival biofilm through non-surgical instrumentation with or without adjunctive therapies [7]. After these steps, patients undergo a clinical re-evaluation to assess the achievement of the endpoints of therapy [EoT: probing pocket depth (PPD) < 4 or PPD < 6 with bleeding on probing (BoP)]. Residual PPD ≥ 6 mm represents indication for periodontal surgery; while PPD 4–5 mm with BoP indicates the need for subgingival re-instrumentation (RSI) [6, 8]. Conversely, sites achieving EoT are enrolled in the supportive periodontal care (SPC) recall system [9].
To this regard, it is still debated whether all residual PPD ≥ 6 mm should undergo surgery, since it has been shown that specific patients, teeth or sites may achieve the EoT after RSI [10, 11]. Moreover, it remains unclear to what extent residual PPD 4–5 with BoP achieves EoT after a second/third cycle of re-instrumentation. This is relevant because residual pockets during SPC have higher risk of disease progression and tooth loss [12, 13]. Finally, it is yet to be established whether open pockets (PPD ≥ 6 mm and PPD 4–5 mm with BoP) which achieved EoT at the first re-evaluation may remain closed at early SPC appointments [14].
Since the number of periodontal surgeries is strictly dependent on the distribution of residual pockets at the time of re-evaluation [8], it is relevant to understand to what extent is appropriate to stress on RSI for both economical and biological costs justification. Moreover, it would be crucial to understand which patients, teeth and sites possess the highest likelihood of EoT after RSI, and which are better indicated for an early surgical approach [15].
Therefore, the aims of this study were to assess: 1) the efficacy of RSI in achieving EoT in residual PPD ≥ 6 mm and 2) in sites 4–5 mm with BoP; 3) whether sites which achieved EoT at the first re-evaluation remained closed during early SPC appointments; 4) the factors at patient-, tooth- and site- level that can predict EoT at each different time point; 5) the need for surgery and the associated costs after one and two cycles of RSI.
Materials and methods
This prospective clinical study was approved by the human subjects ethics board of “A.O.U. Città della Salute e della Scienza” of Turin (Protocol number: 0112880) and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. The manuscript is reported according to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [16].
Study population
Stage III-IV periodontitis patients [4] were consecutively enrolled at the Section of Periodontology at the C.I.R. Dental School of Turin during the period between April 24th and July 31st 2021. All participants gave written informed consent. Age < 18 years, pregnancy or lactation, heavy smokers (> 10/day), conditions or diseases influencing periodontal healing (including uncontrolled diabetes mellitus), and the inability to complete any of the follow-ups were all considered exclusion criteria.
Interventions
As part of the step I of treatment, all patients received oral hygiene instructions and motivation (OHI), and supragingival instrumentation was carried out in one single session. As for step II, subgingival instrumentation was performed using the quadrant-wise conventional method over a 2-week period by one experienced dental hygienist (MRe), using both ultrasonic devices (EMS Piezon Master, EMS, Nyon, Switzerland) and hand curettes (Gracey curettes, Hu-Friedy, Chicago, IL, USA) [7]. Chlorhexidine 0.12% rinses were prescribed twice a day for 1 min throughout the whole step II period [17]. As part of the study protocol, patients were recalled at 4–6 weeks (T1), 3 (T2) and 6 (T3) months after the end of step II. At any of these follow-up recalls, OHI were reinforced, and PPD = 4–5 mm with BoP as well as PPD ≥ 6 mm were re-instrumented using hand/ultrasonic instruments.
Periodontal examination
A full-mouth periodontal examination was performed at baseline (T0), T1, T2 and T3 by the use of a manual periodontal probe (PCP-UNC15, Hu-Friedy, Chicago, IL, USA) by a single experienced examiner (FF). The following clinical parameters were recorded at 6 sites per tooth excluding third molars: PPD, recession (REC), clinical attachment level (CAL), BoP [18], and presence of plaque [19]. Moreover, mobility (Miller index) and furcation involvement were recorded. Full-mouth plaque (FMPS) and bleeding scores (FMBS) were calculated. All patients also received a full-mouth intraoral radiographic examination at T0 [4].
Outcome measures
The primary outcome of this study was EoT defined at site level as PPD < 4 or PPD < 6 without BoP, evaluated at T1, T2 and T3. EoT was only evaluated on a subset of the available sites (n = 1,749) considered open at T0 (i.e., PPD ≥ 4 with BoP or PPD ≥ 6 mm). Sites experiencing relapse after EoT (T0 sites which achieved EoT at T1 and re-opened again) were also considered.
Secondary outcome variables included PPD, CAL and REC changes at the same time-points, evaluated considering all the sites (n = 3,726) of the included subjects. Furthermore, at each timepoint the number of surgeries needed as recommended by the treatment guideline was evaluated [6]. The number of surgeries was computed based on number and distribution of residual PPD ≥ 6 mm at T1, T2 and T3. When such residual pockets were present at the same sextant, they were considered as one single surgery. Also, the cost of the necessary procedures was studied using a fee schedule derived as an average from the tariff quota suggested by the National Association of Italian Dentists (ANDI).
Sample size calculation
Sample size calculation has been performed using an online software. A previous report showed that the mean number of closed pockets at 2 months after non-surgical therapy was 52.5 ± 2.5 [20]. Thus, a further increase of 25% has been considered clinically relevant in order to justify the longer time of follow-up before the surgical treatment plan execution. To obtain a power of 80% and alpha 0.05, a sample of 23 patients have been considered adequate. In order to account for a possible 10% of drop-outs 25 patients were required.
Statistical analyses
All the analyses were performed using a statistical software (STATA/SE®; Statacorp, College Station, Texas, US). Firstly, the rate of EoT at T1, T2 and T3 was described. Secondly, possible T1 predictors (i.e., PPD, plaque, tooth type, site location, mobility, furcation involvement) of EoT at T2 and T3 were explored through multilevel analysis adjusted for clustering. A priori subgroup analyses by residual PPD at T1 (PPD ≥ 6 mm; PPD 4–5 mm with BoP) were also reported. P < 0.05 was considered as statistically significant.
Results
Data retrieved from 25 patients who completed the 6-month re-evaluation were included in the final analysis. Baseline characteristics of the study sample are presented in Table 1. On average, participants were middle aged (57.4 ± 7.9 years of age), 60.0% were males, with current light smokers being 40.0%. Participants presented a baseline mean CAL of 5.2 ± 2.5 mm, PPD of 4.0 ± 1.7 mm, and 71.1 ± 26.9 open pockets. FMBS and FMPS were 63.5 ± 23.0% and 73.9 ± 15.8%, respectively.
Clinical outcomes after single and repeated subgingival instrumentation
All patients were compliant with the study protocol. As expected, steps I-II of periodontal therapy resulted in a significant improvement of all clinical parameters at patient-level (Table 2). At T1, 18 teeth were extracted and a mean reduction of 28.5 ± 14.5 in the number of open pockets was achieved, together with a significant reduction in FMBS and FMPS. RSI provided an additional, albeit modest reduction in mean periodontal parameters at T2 and T3. Overall, the achievement of EoT at T1 was 67.6%, EoT at T2 was 79.2%, while EoT at T3 was 81.3% (Table 3). In the multilevel regression analyses, the factors which negatively influenced EoT at T2 and T3 were multirooted teeth, furcation involvement (degree 2 and 3), initial PPD and interproximal site location (Table 4).
RSI in sites PPD ≥ 6 mm at T1
After the first cycle of RSI, 33.1% of sites with residual PPD ≥ 6 mm achieved EoT. At the end of the second cycle, EoT reached up to 45.9% (Table 3). Multilevel analyses indicated that PPD at T1 was the preeminent predictor of EoT at T2 and T3 (Table 5).
RSI in sites PPD 4–5 mm with BoP at T1
After the first cycle of RSI, 66.8% of sites with PPD 4–5 mm with BoP achieved EoT, whereas a second cycle provided slight changes—72.1% (Table 3). Multilevel analyses indicated how multirooted teeth were associated with inferior rates of EoT both at T2 and T3 (OR = 0.43 and OR = 0.43, respectively); as well as sites with PPD = 5 mm (OR = 0.25 and OR = 0.28, respectively) (Table 5).
Relapse during SPC in sites which achieved EoT at T1
Of the 980 EoT sites at T1, 88 showed relapse at T2 (9.0%), whereas 95 at T3 (9.7%). Multilevel analyses indicated how multirooted teeth (OR = 2.06), PPD at T1 (OR = 0.80), III degree FI (OR = 10.28), and site location (OR = 5.48) were associated with higher rates of relapse at T2; whereas multirooted teeth (OR = 3.08) and site location (OR = 2.23) were associated with higher rates of relapse at T3 (Supplementary Table 1).
Need for surgeries and cost analysis
After steps I-II, 172 sites had PPD ≥ 6 mm which would have been reflected in 2.5 ± 1.6 surgeries in 24 patients, with a mean associated cost of 1,872.00 ± 1,149.00 €. After the first cycle of RSI, 115 sites had PPD ≥ 6 mm which would have been reflected in 1.7 ± 1.3 surgeries in 23 patients, with a mean associated cost of 1,289.00 € ± 937.00 €. After the second cycle of RSI, 93 sites had PPD ≥ 6 mm which would have been reflected in 1.3 ± 1.3 surgeries in 19 patients, with a mean associated cost of 996.00 € ± 978.00 €. The mean number of surgeries and associated costs significantly decreased at different time-points (Table 6).
Discussion
In residual PPD ≥ 6 mm, one and two cycles of RSI yielded EoT in one third and 45% of the cases, respectively. When re-instrumenting PPD 4–5 mm BoP + as per EFP guideline, a relevant benefit (two thirds of additional EoT) was found after the first cycle of RSI, while a further cycle only provided minimal additional benefits. Moreover, 10% of the sites which achieved EoT after steps I-II of therapy manifested relapse at T3. PPD at T1, tooth type (multi-rooted) and interproximal site location were significant negative predictors. Finally, number of needed surgeries and associated costs decreased after each cycle of RSI.
The first question of the present study was focused on evaluating the efficacy of RSI in residual PPD ≥ 6 mm, which are recommended for surgery [6]. Our results indicated benefits in performing one or two cycles of RSI in terms of achievement of EoT. This finding partially contrasts with early randomized clinical trials of Badersten et al. [21] and König et al. [22], where the effects of non-surgical therapy were maximized at the first instrumentation (step II), and then they tended to stabilize after the following RSI cycles. Besides some differences in methodology and study population (i.e. including only single-rooted teeth for the former and only aggressive forms of periodontitis in the latter), the aforementioned studies employed mean patient-level differences in periodontal parameters as study outcomes. In the present investigation, EoT thresholds as from EFP guideline were employed, as they are more closely related to the goal of therapy than commonly reported mean differences in fractions of a millimeter [6, 23]. Also, these composite surrogate outcomes are directly transferable to daily practice and easy to interpret for patients and clinicians [24]. Indeed, the present investigation confirmed previous understanding on the effect of RSI on mean differences in clinical parameters (PPD changes, CAL gain, REC increase), while finding significant benefits, albeit partial, on the number of residual pockets after each RSI cycle. According to our findings, clinicians may consider residual PPD at T1 as the most relevant parameter for decision making, since PPD = 6 mm was associated with higher odds of EoT compared to higher PPD values. The rationale for giving ‘more chances’ to RSI stems from classic studies which compared it to surgery, with unclear clinical relevance of the statistical superiority of the latter [8, 25, 26]. Moreover, leaving more time for tissue healing allows the clinician to possess the best semiotic elements for surgical treatment planning and management [27]. Indeed, in our study 81.3% of baseline pockets achieved EoT at 6 months. Therefore, while RSI could not be considered resolutive in all residual PPD ≥ 6 mm, its advantages could be more relevant from the patient’s perspective, in light of the associated reduced biological (less invasiveness) and economic costs related to surgery.
The second question of the present study was focused on testing the effect of RSI in residual PPD 4–5 mm with BoP, as per EFP guideline [6]. The findings from the present study partially confirmed the benefits of RSI in those cases, however the EoT was not achieved in all situations. According to our findings, clinicians may consider residual PPD = 5 mm and multi-rooted teeth as relevant predictors for decision making, since they were associated with lower EoT rates. These predictors are consistent with the available evidence [15, 28]. To this regard, the concept of ‘critical probing depth’ introduced by Lindhe et al. [29] can be advocated, assuming that the surgical approach resulted in more attachment loss than the non-surgical modality when performed in more shallow PPDs and in anterior compared to posterior teeth [30].
The third question was focused on exploring the effect of SPC in clinical sites which achieved EoT after steps I-II, as per the EFP guideline. Our results highlighted a relapse in 10% of those sites, with a higher rate in PPD = 4 mm, interproximal site location and multi-rooted teeth. This observation may be relevant in tailoring SPC recall frequency and protocols [31].
This study presents some limitations, being relatively short-termed, having a sample size which might have reduced the power for patient level predictors (i.e., smoking, diabetes, and lifestyle factors [32,33,34,35]) and a monocentric setting which might have affected generalizability. In the present investigation, only light smokers were included (< 10 cigarettes a day), representing a considerable part of the sample (40%). Smoking is known to yield a significant impact on bleeding rates and pocket closure [11], although this variable could not be included in the multilevel analysis. Moreover, it may be also advocated that 4–6 weeks represent a too short healing time before the first re-evaluation. This timing has always represented a matter of debate, the decision being influenced by both biological and clinical observations. Despite the junctional epithelium re-establishes on the tooth surface in 1–2 weeks after scaling and root planing [36], the minimal interval allowed for probing a previously treated site is considered 4 to 6 weeks, being the connective tissue slower to heal [37]. However, since clinical guidelines do not make any specific recommendation about this matter, we have based our choice according to the aforementioned biological rationale and to previously published articles [38]. Finally, the absence of a control group could not allow speculation on whether some sites would have closed anyway even without re-instrumenting, or whether surgery would have been more effective in closing pockets than RSI at both short- and long-term. Future randomized clinical trials may clarify all these clinically relevant aspects, providing practice-based evidence feedback for the most effective real-life application of the available EFP guideline.
Conclusions
The current study suggests that RSI may achieve EoT in both residual PPD 4–5 mm BoP + and PPD ≥ 6 mm in a considerable number of cases. PPD at T1, tooth type (multi-rooted) and interproximal site location were significant negative predictors of EoT. Moreover, the number of needed surgeries and associated costs significantly decreased after each RSI cycle. Despite study limitations, the present findings support the decision to perform one or two cycles of RSI before evaluating the surgical approach, for both biological and economical cost justification.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Morales A, Strauss FJ, Hämmerle CHF et al (2021) Performance of the 2017 AAP/EFP case definition compared with the CDC/AAP definition in population-based studies. J Periodontol. https://doi.org/10.1002/JPER.21-0276
Botelho J, Mascarenhas P, Viana J et al (2022) An umbrella review of the evidence linking oral health and systemic noncommunicable diseases. Nat Commun 13:7614. https://doi.org/10.1038/s41467-022-35337-8
Marruganti C, Baima G, Aimetti M et al (2023) Periodontitis and low cognitive performance: A population-based study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13779
Papapanou PN, Sanz M, Buduneli N et al (2018) Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89:S173–S182. https://doi.org/10.1002/JPER.17-0721
Antonoglou GN, Romandini M, Meurman JH et al (2023) Periodontitis and edentulism as risk indicators for mortality: results from a prospective cohort study with 20 years of follow-up. J Periodontal Res 58:12–21. https://doi.org/10.1111/jre.13061
Sanz M, Herrera D, Kebschull M et al (2020) Treatment of stage I-III periodontitis—The EFP S3 level clinical practice guideline. J Clin Periodontol 47:4–60. https://doi.org/10.1111/jcpe.13290
Suvan J, Leira Y, Moreno Sancho FM et al (2020) Subgingival instrumentation for treatment of periodontitis. A systematic review. J Clin Periodontol 47(Suppl 22):155–175. https://doi.org/10.1111/jcpe.13245
Sanz-Sánchez I, Montero E, Citterio F et al (2020) Efficacy of access flap procedures compared to subgingival debridement in the treatment of periodontitis. A systematic review and meta-analysis. J Clin Periodontol 47:282–302. https://doi.org/10.1111/jcpe.13259
Trombelli L, Farina R, Pollard A et al (2020) Efficacy of alternative or additional methods to professional mechanical plaque removal during supportive periodontal therapy: a systematic review and meta-analysis. J Clin Periodontol 47:144–154. https://doi.org/10.1111/jcpe.13269
Tomasi C, Koutouzis T, Wennström JL (2008) Locally delivered doxycycline as an adjunct to mechanical debridement at retreatment of periodontal pockets. J Periodontol 79:431–439. https://doi.org/10.1902/jop.2008.070383
Citterio F, Gualini G, Chang M et al (2022) Pocket closure and residual pockets after non-surgical periodontal therapy: a systematic review and meta-analysis. J Clin Periodontol 49:2–14. https://doi.org/10.1111/jcpe.13547
Matuliene G, Pjetursson BE, Salvi GE et al (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35:685–695. https://doi.org/10.1111/j.1600-051X.2008.01245.x
Ramseier CA, Woelber JP, Kitzmann J et al (2020) Impact of risk factor control interventions for smoking cessation and promotion of healthy lifestyles in patients with periodontitis: a systematic review. J Clin Periodontol 47(Suppl 22):90–106. https://doi.org/10.1111/jcpe.13240
Leow NM, Moreno F, Marletta D et al (2022) Recurrence and progression of periodontitis and methods of management in long-term care: a systematic review and meta-analysis. J Clin Periodontol 49:291–313. https://doi.org/10.1111/jcpe.13553
Tomasi C, Leyland AH, Wennström JL (2007) Factors influencing the outcome of non-surgical periodontal treatment: a multilevel approach. J Clin Periodontol 34:682–690. https://doi.org/10.1111/j.1600-051X.2007.01111.x
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Figuero E, Roldán S, Serrano J et al (2020) Efficacy of adjunctive therapies in patients with gingival inflammation: a systematic review and meta-analysis. J Clin Periodontol 47:125–143. https://doi.org/10.1111/jcpe.13244
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38. https://doi.org/10.1902/jop.1972.43.1.38
D’Aiuto F, Ready D, Parkar M, Tonetti MS (2005) Relative contribution of patient-, tooth-, and site-associated variability on the clinical outcomes of subgingival debridement I Probing depths. J Periodontol 76:398–405. https://doi.org/10.1902/jop.2005.76.3.398
Badersten A, Nilveus R, Egelberg J (1984) Effect of nonsurgical periodontal therapy. III. Single versus repeated instrumentation. J Clin Periodontol 11:114–124. https://doi.org/10.1111/j.1600-051x.1984.tb00839.x
König J, Schwahn C, Fanghänel J et al (2008) Repeated scaling versus surgery in young adults with generalized advanced periodontitis. J Periodontol 79:1006–1013. https://doi.org/10.1902/jop.2008.070380
Loos BG, Needleman I (2020) Endpoints of active periodontal therapy. J Clin Periodontol 47:61–71. https://doi.org/10.1111/jcpe.13253
Tomasi C, Wennström JL (2017) Is the use of differences in the magnitude of CAL gain appropriate for making conclusions on the efficacy of non-surgical therapeutic means? J Clin Periodontol 44:601–602. https://doi.org/10.1111/jcpe.12733
Pihlstrom BL, Ortiz-Campos C, McHugh RB (1981) A randomized four-year study of periodontal therapy. J Periodontol 52:227–242. https://doi.org/10.1902/jop.1981.52.5.227
Ramfjord SP, Caffesse RG, Morrison EC et al (1987) 4 modalities of periodontal treatment compared over 5 years*. J Clin Periodontol 14:445–452. https://doi.org/10.1111/j.1600-051X.1987.tb02249.x
Aimetti M (2014) Nonsurgical periodontal treatment. Int J Esthet Dent 9:251–267
Axtelius B, Söderfeldt B, Attström R (1999) A multilevel analysis of factors affecting pocket probing depth in patients responding differently to periodontal treatment. J Clin Periodontol 26:67–76. https://doi.org/10.1034/j.1600-051x.1999.260202.x
Lindhe J, Socransky SS, Nyman S et al (1982) “Critical probing depths” in periodontal therapy. J Clin Periodontol 9:323–336. https://doi.org/10.1111/j.1600-051x.1982.tb02099.x
Heitz-Mayfield LJA, Lang NP (2013) Surgical and nonsurgical periodontal therapy. Learned and unlearned concepts. Periodontol 2000 62:218–231. https://doi.org/10.1111/prd.12008
Nibali L, Sun C, Akcalı A et al (2018) The effect of horizontal and vertical furcation involvement on molar survival: a retrospective study. J Clin Periodontol 45:373–381. https://doi.org/10.1111/jcpe.12850
Marruganti C, Baima G, Grandini S et al (2023) Leisure-time and occupational physical activity demonstrate divergent associations with periodontitis: a population-based study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13766
Marruganti C, Romandini M, Gaeta C et al (2023) Healthy lifestyles are associated with a better response to periodontal therapy: a prospective cohort study. J Clin Periodontol. https://doi.org/10.1111/jcpe.13813
Marruganti C, Gaeta C, Romandini M et al (2023) Multiplicative effect of stress and poor sleep quality on periodontitis: A university-based cross-sectional study [published online ahead of print, 2023 Jul 21]. J Periodontol. 2023. https://doi.org/10.1002/JPER.23-0209
Romano F, Perotto S, Mohamed SEO et al (2021) Bidirectional association between metabolic control in type-2 diabetes mellitus and periodontitis inflammatory burden: a cross-sectional study in an Italian population. J Clin Med 10:1787. https://doi.org/10.3390/jcm10081787
Caton JG, Zander HA (1979) The attachment between tooth and gingival tissues after periodic root planing and soft tissue curettage. J Periodontol 50:462–466. https://doi.org/10.1902/jop.1979.50.9.462
Stahl SS, Weiner JM, Benjamin S, Yamada L (1971) Soft tissue healing following curettage and root planing. J Periodontol 42:678–684. https://doi.org/10.1902/jop.1971.42.11.678
Cercek JF, Kiger RD, Garrett S, Egelberg J (1983) Relative effects of plaque control and instrumentation on the clinical parameters of human periodontal disease. J Clin Periodontol 10:46–56. https://doi.org/10.1111/j.1600-051x.1983.tb01266.x
Funding
Open access funding provided by Università degli Studi di Torino within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
FF contributed to study conception and design, data acquisition, and critically revised the manuscript. GB and MRo contributed to study design, data analysis, data interpretation, and manuscript drafting. MRe contributed to data acquisition, and critically revised the manuscript. FC and FR contributed to data analysis, and critically revised the manuscript. MA, FM, and GMM contributed to study conception and critically revised the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The investigation was approved by Institutional Ethics Committee of the AOU Città della Salute e della Scienza Turin, Italy (approval No. 0112880).
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ferrarotti, F., Baima, G., Rendinelli, M. et al. Pocket closure after repeated subgingival instrumentation: a stress test to the EFP guideline for stage III-IV periodontitis. Clin Oral Invest 27, 6701–6708 (2023). https://doi.org/10.1007/s00784-023-05279-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05279-6