Abstract
Objectives
To assess clinical, radiological and esthetic outcomes of restorations supported by root-analogue implants (RAIs) or roots of severely damaged teeth after forced orthodontic extrusion (FOE).
Materials and methods
Clinical data regarding milled one-piece (titanium/zirconia roots and zirconia abutments) RAIs (REPLICATE™ System) and FOE were recorded and retrospectively evaluated for 40 patients by two investigators. Strict inclusion and exclusion criteria were applied. Functional and esthetic outcomes were assessed for n = 20 pre-molars and n = 20 anterior teeth via comparison of radiographic and digital images applying the novel Functional Implant Prosthodontic Score (FIPS). Krippendorff’s alpha coefficient was calculated to assess inter-rater reliability. Mann–Whitney-U-Test was used to compare the assessed parameters. Level of significance was set to p < 0.05.
Results
After a mean observation period of 18.4 ± 5.7 months for restorations supported by RAIs and 43.9 ± 16.4 months for restorations after FOE, mean FIPS scores were 9.2/8.8 ± 1.1/1.2 (RAIs) and 7.4/7.7 ± 1.3/1.5 (FOE), respectively. Krippendorff’s alpha coefficients did not reveal unacceptable inter-rater reliabilities regarding the investigators and applicability of FIPS. Significant differences were documented when comparing restorations after FOE or supported by RAIs regarding bone loss (p < 0.01), presence of papillae (p < 0.05) and quality and quantity of mucosa (p < 0.02) in favor of FOE.
Conclusions
Within the main limitations of sample size and the retrospective study design, both concepts seem to provide clinically acceptable results.
Clinical relevance
Bone- and tissue-preserving characteristics regarding the concept of FOE are promising. It could be applicable for socket preservation and subsequent conventional implant placements in an adapted workflow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In case of extensively destroyed teeth, dentists must regularly decide between tooth preservation and extraction [1, 2]. Regarding this decision, future prosthodontic treatment options to restore function and esthetics should be considered. For the restoration of single-tooth gaps, conventional treatment options such as fixed dental prostheses (FDPs) [3,4,5], resin-bonded fixed dental prostheses (RBFDPs) [6,7,8] and implant-retained restorations [3, 9,10,11,12,13] have been established in daily dental routine. Usually, at this clinical state, teeth have already been removed or are expected to be extracted. However, it is well known that tooth extraction is accompanied by remodeling processes of the surrounding hard and soft tissues whereby volume is usually lost [14]. This can lead to restorative limitations in general and become a challenge, especially in the esthetic zone. To counteract these resorption processes after extraction, immediate implant placement continues to be controversially discussed [15,16,17,18,19,20,21]. Thereby, root-analogue implants (RAIs) represent a highly individual procedure of immediate dental implant installations.
The concept of RAIs was first scientifically described in 1969 with the Dental Polymer Implant Concept by Hodosh et al. [22]. Thereby, RAIs were fabricated from polymethyl methacrylate (PMMA) after extraction with a transfer technique using the removed roots and plaster to copy the anatomical shape. However, connective tissue healing of PMMA RAIs led to the discontinuation of the concept [23]. At the beginning of the 90 s, the idea was revisited and experiments in beagle dogs with roots copied by machine and made of titanium were conducted [24]. After two, twelve and 36 months, the evaluation of clinical, radiographic and histological parameters showed successful osseointegration of 88% of 32 duplicates. Consequently, in the late 90 s, a research group led by Strub and Kohal et al. introduced the "Re-Implant System" (Re-Implant GmbH, Hagen, Germany) [25]. The extracted roots were fabricated from titanium using a milling process, but clinical follow-up in 2002 presented an unsatisfactory survival rate of 48%. By the end of the 2000s, RAIs could be fabricated using modern computer-aided design/computer-aided manufacturing (CAD/CAM) technologies. Again, extracted teeth were used as basis for fabrication and in a two-year clinical study, a survival rate of 92% was documented for the so-called "BioImplant Concept" with RAIs made from zirconia [26]. Finally, the introduction of cone beam computed tomography (CBCT) into dentistry allowed for a prefabrication of RAIs, making immediate implant installation possible without a time delay between extraction and insertion [27]. Recently published data revealed stable peri-implant soft tissue conditions and satisfying esthetic outcomes regarding RAIs with a survival rate of 94.4% after a short-time observation period of 18.9 ± 2.4 months [28]. Nevertheless, clinical studies on RAIs are scarce, especially compared to those for screw-shaped implants. Therefore, more data including different manufacturing techniques and biomaterials are regularly requested in current literature [29,30,31,32,33,34,35,36].
On the other hand, to eliminate the concerns regarding resorption processes, the possibility of tooth/root preservation and restoration should be discussed as a viable treatment option. Thereby, especially the size of defects and subgingival restoration margins can be problematic by affecting the patient’s periodontal health [37] as they might violate biologic width [38]. Additionally, scientific literature demands a circumferential ferrule design preparation for long-term success of restorations [39, 40]. To re-establish biologic width and to facilitate a circumferential ferrule design preparation, pre-prosthetic treatment protocols such as surgical crown lengthening [41] or forced orthodontic extrusion (FOE) procedures [42, 43] have been suggested in the literature. Surgical crown lengthening is an operative procedure associated with an osseous reduction of the alveolar bone and an inevitable lengthening of the clinical crown [44]. This might lead to esthetic deformities, which poses an esthetic problem in the anterior zone. In contrast, FOE is a valid treatment alternative [44] maintaining soft and hard tissues. Therefore, the procedure is regarded maximally tissue preserving and minimally invasive [45]. Extrusion is a defined orthodontic movement in occlusal direction. It enables the re-establishment of biologic width and exposes sound tooth structure to facilitate placement of dental restorations [46]. Orthodontic extrusion is indicated for teeth with horizontal, shear or cuspal fractures, carious destruction, resorption and iatrogenic perforations [46]. Although the treatment procedure of FOE was described as early as in 1973 [42] scientific evidence is currently limited to few studies [43, 47, 48]. Numerous articles have been published demonstrating different approaches of orthodontic extrusion, as by fixed orthodontic arch wires and elastics [49], removable orthodontic appliances [50], existing removable partial dentures [51] as well as complete dentures [52]. Scientific evidence on the long-term prognosis for teeth after FOE is scarce. However, there are two clinical studies reporting on favorable survival rates after a short time of observation and concluding orthodontic relapse as the major complication of this technique [48, 53].
The aim of this retrospective investigation was to evaluate and compare clinical, radiological and esthetic outcomes of prosthodontic rehabilitations supported by RAIs or natural roots after FOE. The working hypothesis was, that both treatment concepts show comparable results.
Materials and methods
Study design and ethical approval
For the present retrospective investigation, available clinical data regarding restorations supported by RAIs or natural roots after FOE were retrospectively evaluated and compared. Ethical approval was given by the local Ethical Committee of Charité – Universitätsmedizin Berlin, Germany (application numbers: EA4/140/18 and EA2/301/20). All RAI-treatments were performed by the author D.H. and respective follow-up examinations by the author M.W.H.B. All FOE-treatments and follow-up examinations were performed by the author M.B. To reduce subjective bias, analyzed outcomes were evaluated independently by both first and last specified authors of this article. All patients have received and signed a written informed consent form and patient information. It was conducted considering the STROBE statement for observational studies (https://www.strobe-statement.org) where applicable.
For treatments with a RAI, the following criteria regarding the patients had to be fulfilled: 1) Non-smokers; 2) No medication affecting the bone metabolism; 3) Non-inflammatory surrounding soft and hard tissues and 4) Bone compartments surrounding the relevant tooth had to be intact. For FOE following inclusion criteria were defined: 1) Patients in need of a restoration of a deeply destroyed tooth with two adjacent teeth; 2) Probing depths ≤ 2 mm and defects violating the biologic width and/or a missing ferrule design preparation; 3) Prospective crown-to-root ratio ≤ 1; 4) Tooth mobility ≤ 1 and prospective single-tooth restorations. Teeth with suspicion of hypercementosis/ankylosis, molars and teeth with vertical root fractures were excluded. Treatments were only performed in patients whose compliance regarding the necessary monitoring was expected.
Due to the retrospective comparative study design, the cases to be evaluated had to be selected based on the available data. Therefore, n = 10 pre-molars restored with single crowns supported by RAIs, n = 10 severely damaged roots of pre-molars restored with single crowns after FOE, n = 10 anterior teeth (canine to canine) restored with single crowns supported by RAIs and n = 10 severely damaged roots of anterior teeth restored with single crowns after FOE were selected. Thus, 40 cases could be included. Available data were anonymized, retrospectively evaluated and statistically analyzed. Post-hoc power-analysis was performed with a free-to use software to calculate statistical power (G* Power 3.1.9.7, Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) with a sample size of n = 20 per group, α = 0.05 and an effect size of 1.17 resulting in a power of 0.97 (97%).
Root-analogue implants (RAIs)
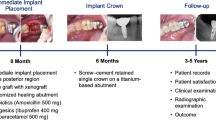
For rehabilitations with RAIs, these had to be manufactured individually before surgeries. Impressions were taken with customized trays and a polyether material (Impregum, 3 M Deutschland GmbH, Neuss, Germany). These were cast with type IV plaster and digitized with a laboratory scanner where after the model data were available as Standard Triangle/Tessellation Language (STL) datasets. Bite records were taken with an injectable elastomeric A-silicone (Futar D, KettenbachGmbH&Co. KG, Eschenburg, Germany) and DICOM data were exported from an x-ray device (PAX i-3D, VATECH, Hwaseong-si, Gyeonggi-do, South Korea). A highly trained specialist of the manufacturer superimposed the DICOM and STL data and designed the Temporary Protective Covers (TPCs), implant and abutment portions of the RAIs (Fig. 1e and f) and Try-Ins (exact copies of the RAIs made from sterilizable resin, Fig. 1c and d). From resulting Computer Aided Design (CAD) data, TPCs and RAI components were milled in a Computer Aided Manufacturing (CAM) process. All ceramic parts (abutment portion, root portion in case of all-ceramic RAIs and TPCs) were made of yttria-stabilized tetragonal polycrystalline zirconia (Y-TZP) and sintered. With hybrid RAIs, root portion was manufactured from pure titanium (medical grade IV) and bonded to the aforementioned abutment portions made from Y-TZP in a special oven process using a biocompatible glass material without any voids. These connections were checked using x-rays within quality control. Afterwards, root portions of both (all-ceramic and hybrid RAIs) were modified with macro- and micro retentions (medical grade corundum and etched). The Benex Extraction-System (Benex Extraction-System, Helmut Zepf Medizintechnik GmbH, Seitlingen-Oberflacht, Germany, Fig. 1b) was used to remove teeth minimally invasive in vertical direction. If this was not successful, teeth were carefully removed using conventional extraction techniques. Intact surrounding bone compartments were obligatory. The expected fit of RAIs was tested by using the respective Try-Ins (Fig. 1d). Before implant insertion, implant surfaces and alveoli were wetted with Plasma Rich Growth Factors (PRGFs; BTI Biotechnology Institute, San Antonio, Spain). RAIs were carefully placed (Fig. 1e) and present voids were filled with PRGFs as well. As load protection TPCs were semi-adhesively attached (RelyX Ultimate, 3 M Deutschland GmbH) to one or both adjacent teeth depending on the design. This provided a protective gap of approx. 0.6 mm between the abutment portion of RAIs and TPCs it selves. The workflow has already been described and illustrated in detail in a publication in 2020 [28] and is additionally shown in Fig. 1. Healing was usually checked 3–6 month after surgeries using clinical and radiological parameters. Prosthodontic treatments were performed in the office of the author D.H. and different referring dentists, whereby no constantly defined workflow was followed. In total, 16 hybrid and four all-ceramic RAIs with respective restorations were investigated.
Clinical workflow regarding the extraction of a deeply destroyed tooth (FDI 24) and exemplary immediate implant placement of a RAI. a Initial clinical situation (FDI 24); b Application of the Benex Extraction-System; c Extracted roots and Try-In; d Testing the expected fit with Try-In; e Insertion of milled one-piece hybrid RAI and (f) Clinical situation after healing period. Abbreviations: (1) FDI: Fédération Dentaire Internationale; (2) RAIs: Root-analogue implants
Forced orthodontic extrusion (FOE)
Prior to orthodontic extrusion, probing depths, tooth mobility, defect size and radiographic images were assessed to determine the amount of extrusion and the prospective crown-to-root ratio for each patient individually. Interocclusal available space for orthodontic extrusion was analyzed with the aid of gypsum models. After removal of insufficient restorations, a fiber-reinforced composite-based post (Extrusion pin, Komet Dental, Lemgo, Germany) was placed on the root surface of respective teeth with self-adhesive resin (RelyX Unicem 2 Automix, 3 M Deutschland GmbH, Fig. 2c) in central vestibulo-oral direction, at the widest root diameter.
Clinical workflow regarding the restoration of a deeply destroyed tooth (FDI 24) after FOE. a Initial clinical situation (FDI 24); b Buccal cusp of the tooth is missing; c Orthodontic elastics initiate tooth movement in occlusal direction; d Tooth is splinted to adjacent teeth after successful extrusion for time of retention; Final preparation from buccal (e) and from occlusal (f) shows a circumferential ferrule design preparation. Abbreviations: (1) FDI: Fédération Dentaire Internationale; (2) FOE: Forced orthodontic extrusion
A second post serving as anchorage was adhesively bonded to adjacent teeth with flowable composite resin (Tetric EvoFlow, Ivoclar Vivadent AG, Schaan, Liechtenstein, Fig. 2c). Elastics were placed in the orthodontic appliance to initiate forced orthodontic extrusion with forces > 0.5N (Fig. 2c). At the same appointment, supra-crestal fibrectomy, scaling and root planning procedures were performed [54]. In some clinical cases two bars had to be bonded to adjacent teeth due to minor occlusal space. In clinical situations requiring crown restorations on neighboring teeth, anchorage was realized with the aid of a provisional FDP and a reduction of the pontic area to allow for a sufficient amount of extrusion. Clinical details on the workflow have already been described and published [47]. An exemplary workflow is additionally shown in Fig. 2. Elastics were changed by the patients twice daily due to the loss of tension. Patients were available for control visits once a week. The mean amount of extrusion was 3.50 ± 0.87 mm and the mean time of extrusion 17.88 ± 10.98 days. After extrusion, teeth were bonded to adjacent teeth with composite resin (Tetric EvoFlow, Ivoclar Vivadent AG, Fig. 2d) for a retention period of at least 8 weeks (mean time of retention 130.60 ± 89.12 days) to prevent orthodontic relapse [46]. After revision of endodontic fillings, placements of glass-fiber posts (X-Post, DentsplySirona, Bensheim, Germany) were performed where indicated, teeth were built up with composite resin and restored with single crowns.
Study parameters
Within the framework of a feasibility analysis regarding this investigation, existing data sets were reviewed for completeness by the authors M.B. and M.W.H.B. to be able to compare restorations supported by RAIs or natural roots after FOE. The novel Functional Implant Prosthodontic Score (FIPS) was chosen [55] for evaluation and slightly modified regarding rehabilitations of natural roots after FOE not representing implant-retained restorations (Table 1). It was selected as it is a straightforward, self-explaining, reliable, reproducible and quickly applicable score [55, 56].
FIPS is defined by five variables, allowing to evaluate the interproximal area, the occlusion, the design, the mucosa and the bone. After rating every mentioned parameter with 0, 1 or 2, a maximum score of 10 can be achieved by a single restoration (Table 1). In case of subcategories (i.e. “interproximal” with “contacts” and “papillae”) with different ratings, the lowest has to be selected. Therefore, for evaluation, following data had to be present: 1) Photographs for the visual assessment of papillae, the design/esthetics of the restorations, and the mucosa; 2) Documented information regarding the interproximal contacts (checked with dental floss); 3) Documented information regarding the static and dynamic occlusion (checked with shimstock foil, thickness: 8 μm); 4) Available x-rays for the evaluation of marginal bone loss.
For evaluation of interproximal bone changes regarding restorations of severely damaged roots after FOE, radiographic images of teeth before intervention and at recall appointments were superimposed. Therefore, reference lines were drawn on apices and incisal edges of neighboring teeth. The root length of the extruded tooth was divided into ten equal segments. An interproximal bone change of one tenth in a section was defined as interproximal bone loss [57]. A stable interproximal bone level was rated with 2, a change in one tenth of a section was rated with 1 and an interproximal bone loss of more than one tenth of a section was rated with 0 (Fig. 3).
Study participant treated with a single-crown after FOE treatment in regio 24 (FDI). Illustration based on original publication of FIPS: a lateral and b occlusal views as well as (c) 2D radiographic image. Abbreviations: (1) FOE: Forced orthodontic extrusion; (2) FDI: Fédération Dentaire Internationale; (3) FIPS: Functional Implant Prosthodontic Score [55]
Due to the availability of the implant lengths of RAIs, the evaluation of bone loss could be carried out in accordance with FIPS score after superimposition of pre- and post-loading x-rays using mathematical rule of three (Fig. 4). Total marginal bone loss without a view to the rough-smooth border between implant and abutment portions were rated. Due to the retrospective study design, no individual bite holders could be used for both investigated concepts.
Study participant treated with a RAI-supported single-crown in regio 24 (FDI). Illustration based on original publication of FIPS: a lateral and (b) occlusal views as well as (c) 2D radiographic image. Abbreviations: (1) RAI: Root-analogue implant; (2) FDI: Fédération Dentaire Internationale; (3) FIPS: Functional Implant Prosthodontic Score [55]
Statistical analysis
All statistical tests were performed by an independent examiner using “SciPy” (https://scipy.org/, last accessed 13th of March, 2022), a Python-based open source software environment mainly used for scientific analysis, visualizations and related activities. Krippendorff’s alpha coefficient was calculated to assess inter-rater reliability between the authors M.W.H.B. and M.B. Due to ordinal FIPS data, Mann–Whitney-U-Test was used to compare the assessed parameters regarding restorations of natural roots after FOE or supported by RAIs. Level of significance was set to p < 0.05.
Results
After analysis of available datasets, 40 patient cases could be retrospectively evaluated. Mean age of patients treated with RAIs was 55.9 ± 14.0 years and 47.3 ± 18.5 years for FOE. The gender ratio for RAIs was 70% females and 30% males, for FOE 45% females and 55% males. Evaluation of RAI-supported restorations was based on data raised 18.4 ± 5.7 months after intervention. For restorations of natural roots after FOE, the observation period was calculated to be 43.9 ± 16.4 months. Survival rates for all investigated restorations was 100%. Ceramic chipping was documented for one restoration each (FOE and RAI) within the follow-up period. Additionally orthodontic relapse occurred in three teeth (15%). Detailed information regarding FIPS including means and standard deviations (SD) for both investigators are shown in Table 2. Krippendorff’s alpha coefficients did not reveal unacceptable inter-rater reliabilities regarding the investigators and applicability of FIPS for both concepts, FOE and RAIs (Tables 3 and 4). Due to “occlusion” ratings of FIPS = 2 for all investigated restorations, no statistical evaluation could be carried out in this regard. However, statistical analysis revealed significant differences comparing restorations of natural roots after FOE or supported by RAIs. For both authors (M.W.H.B. and M.B.) significant differences were documented when comparing the concepts of FOE and RAIs regarding “bone” in favor of FOE (p < 0.01, Table 2). For M.B. significant differences were also documented regarding “interproximal” (p < 0.05) and “mucosa” in favor of FOE (p < 0.02, Table 2).
Discussion
To the best knowledge of the authors, the present study is the first that compares restorations supported by RAIs or natural roots preserved by means of FOE. A retrospective data evaluation was performed because both concepts required for comparable basic prerequisites: deeply destroyed teeth that would have been extracted due to their extension of decay in many cases [28, 47]. In addition, little scientific data is available for both treatment options, mainly consisting of case reports and case series [26, 59,60,61,62,63,64,65,66,67,68,69]. Therefore, more clinical data is desirable and has already been demanded [28, 47, 70]. Working hypothesis must be rejected in particular regarding marginal bone levels in favor of the concept of FOE.
FIPS was chosen for evaluations as it combines functional, esthetic and radiographic parameters, while being a simple, self-explaining, reliable, reproducible and quickly applicable score [55, 56]. Although initially developed for comparison of implant-retained restorations it allows the assessment of clinical and functional parameters for both treatment concepts. Moreover, it might document risk factors and might allow for long-term prognosis. In comparison, this is not the case with other assessment measures such as the pink and white esthetic score [71, 72] or the United States Public Health Service (USPHS) criteria [73]. FIPS is therefore a simple and reproducible score for (implant-supported) restorations [55, 56]. Thereby, it should be mentioned, that FIPS was originally developed for implant-retained restorations. However, four out of five parameters can be applied analogously (Table 1). Documented mean scores of 9.2/8.8 ± 1.1/1.2 (FOE) and 7.4/7.7 ± 1.3/1.5 (RAIs, Table 2) represent highly satisfying results regarding investigated cases, especially for restorations of natural roots after FOE. An adapted assessment of bone loss after FOE as described in materials and methods was applicable (Table 1).
Taking a separate look at the sub-parameters of FIPS, for both investigators, evaluated bone loss was significantly higher after immediate placement of RAIs compared to the concept of FOE (p < 0.01, Table 2). This result is also supported by the documented “moderate” (RAIs) to “almost perfect” (FOE) inter-rater reliabilities (Tables 3 and 4). For the author M.B. significantly better scores were also achieved regarding “interproximal” (p < 0.05) and “mucosa” (p < 0.02, Table 2) after utilizing the concept of FOE. These results are supported by “moderate” (FOE) to “almost perfect” (RAIs) inter-rater reliabilities (Tables 3 and 4) regarding "interproximal", though no statistically significant differences were documented for the author M.W.H.B. However, for “mucosa” only weak inter-rater reliabilities were documented (Tables 3 and 4), which should put the interpretation into perspective and may indicate subjective bias.
According to these results, it can be assumed that the concept of FOE seems to prevent marginal bone loss compared to immediate implant installation of RAIs. This tendency in favor of the concept of FOE can also be observed regarding soft tissues, which, however, seems to have a more subjective component than in the assessment of bone. In comparison a mean pink esthetic score of 7.45 ± 1.50, representing highly satisfying results as well, was documented in an extensive follow-up study of milled RAIs in 2020 [28]. These findings are supported by a scoping review, highlighting that RAIs might prevent a loss of alveolar bone volume with maintenance of peri-implant soft tissues leading to an improved esthetic and functional prosthetic result [36]. However, the review was focused on RAIs manufactured from zirconia and a prospective one-year clinical follow-up study documented higher survival rates for milled titanium RAIs compared to milled zirconia RAIs and RAIs manufactured by direct laser metal sintering (DLMS) [31]. This brief illustration of different materials and manufacturing processes highlights the need for further clinical studies on RAIs, especially regarding manufacturing processes and material selection.
Both treatment options are strongly limited by their inclusion criteria as described in the material and methods section. Functional aspects and available occlusal space are particularly important. Regarding RAIs, preservation of surrounding bones during surgery is mandatory. Additionally, its fit can only be checked intraoperatively, after the root has already been removed. Thus, complications can lead to short-term discontinuation of treatment. For the concept of FOE main limitations are patient’s compliance as they are expected to change the orthodontic elastics and losses of the applied fiber-reinforced posts on root surfaces or neighboring teeth. However, no severe complications can be induced, but quite the opposite: FOE can be an alternative in case of absolute contraindications regarding implant therapy [74, 75], limitation of treatment costs [76] and for growing, young patients [77, 78].
Despite possible limitations and complications, it should be noted that conventional restorations with FDPs, RBFDPs or conventional screw-shaped implants are still possible even if RAI-supported restorations or restorations of natural roots after FOE fail. However, regarding the results of marginal bone loss, possible compromised bone volume after RAI loss should be critically kept in mind. No data in this context is available in the literature.
Though bone loss based on two-dimensional x-rays was applied in numerous publications [79, 80], findings should be interpreted with care. Additionally, the retrospective design and no use of standardized radiographs with customized x-ray holders are limiting the meaningfulness of the results. Furthermore, it must be mentioned, that the mean clinical service differed between 18.4 ± 5.7 months (RAIs) and 43.9 ± 16.4 months (FOE). Marginal bone loss in the RAI group might even be higher as reported after the mean service time of restorations utilizing the concept of FOE. Presumably clinical, radiological and esthetic outcomes of restorations after FOE recorded after approx. 1.5 years wouldn’t effect FIPS values negatively compared to after approx. 3.5 years as specified. To minimize subjective bias, all patient cases were assessed by two practitioners independently. Additionally, inter-rater reliabilities were calculated with Krippendorff’s alpha and McHugh’s strict interpretation model was applied [58]. Compared to other interpretations, inter-rater reliability of 0.40 – 0.59 is thereby already described as “weak”, whereas it is described as “fair”, “good” or “moderate” in other interpretation scales. However, it demonstrated, that the “own" procedure tends to be rated as better than the "other" one, respectively. Thus, these results confirm, but also put into perspective, the objectivity of FIPS. This may also highlight the influence of subjective bias especially with regard to studies with a single examiner/practitioner. In this regard, it should be noted in conclusion that all RAI-treatments were performed by the author D.H. and respective follow-up examinations by the author M.W.H.B. Furthermore, all FOE-treatments and follow-up examinations were performed by the author M.B. It would have been more desirable if the assessment by means of FIPS had been carried out by at least a single or multiple completely independent practitioners. However, regarding the additional effort and the specialty of treatment procedures, this was not implemented. In conclusion, this should be kept in mind as source of bias despite calculations and discussion of inter-rater reliabilities.
Conclusions
It can be concluded that both concepts are equal opportunities in restoring deeply destroyed, i.e. “unrestorable”, teeth showing clinically acceptable results. Nevertheless, they primarily play a role alongside conventional prosthetic treatment options as FDP, rbFDP or an implant-retained single crown. However, especially bone- and tissue-preserving characteristics regarding the concept of FOE are promising. It might also be applicable regarding scheduled socket preservation and subsequent conventional dental implant placement in an adapted workflow [81]. Further long-term data on success, survival, functional and esthetic outcomes are still desirable for both concepts.
References
Torabinejad M, Anderson P, Bader J, Brown LJ, Chen LH, Goodacre CJ, Kattadiyil MT, Kutsenko D, Lozada J, Patel R et al (2007) Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent 98:285–311. https://doi.org/10.1016/S0022-3913(07)60102-4
Pjetursson BE, Heimisdottir K (2018) Dental implants - are they better than natural teeth? Eur J Oral Sci 126(Suppl 1):81–87. https://doi.org/10.1111/eos.12543
Pjetursson BE, Bragger U, Lang NP, Zwahlen M (2007) Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 18(Suppl 3):97–113. https://doi.org/10.1111/j.1600-0501.2007.01439.x
Sailer I, Pjetursson BE, Zwahlen M, Hammerle CH (2007) A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part II: Fixed dental prostheses. Clin Oral Implants Res 18(Suppl 3):86–96. https://doi.org/10.1111/j.1600-0501.2007.01468.x
Lulic M, Bragger U, Lang NP, Zwahlen M, Salvi GE (2007) Ante’s (1926) law revisited: a systematic review on survival rates and complications of fixed dental prostheses (FDPs) on severely reduced periodontal tissue support. Clin Oral Implants Res 18(Suppl 3):63–72. https://doi.org/10.1111/j.1600-0501.2007.01438.x
Pjetursson BE, Tan WC, Tan K, Bragger U, Zwahlen M, Lang NP (2008) A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin Oral Implants Res 19:131–141. https://doi.org/10.1111/j.1600-0501.2007.01527.x
Kern M (2005) Clinical long-term survival of two-retainer and single-retainer all-ceramic resin-bonded fixed partial dentures. Quintessence Int 36:141–147
Kern M (2017) Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J Dent 56:133–135. https://doi.org/10.1016/j.jdent.2016.11.003
Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A (2012) A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res 23(Suppl 6):22–38. https://doi.org/10.1111/j.1600-0501.2012.02546.x
Jung RE, Pjetursson BE, Glauser R, Zembic A, Zwahlen M, Lang NP (2008) A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res 19:119–130. https://doi.org/10.1111/j.1600-0501.2007.01453.x
Roccuzzo A, Imber JC, Marruganti C, Salvi GE, Ramieri G, Roccuzzo M (2022) Clinical outcomes of dental implants in patients with and without history of periodontitis: A 20-year prospective study. J Clin Periodontol 49:1346–1356. https://doi.org/10.1111/jcpe.13716
Schmid E, Morandini M, Roccuzzo A, Ramseier CA, Sculean A, Salvi GE (2020) Clinical and radiographic outcomes of implant-supported fixed dental prostheses with cantilever extension. A retrospective cohort study with a follow-up of at least 10 years. Clin Oral Implants Res 31:1243–1252. https://doi.org/10.1111/clr.13672
Schmid E, Roccuzzo A, Morandini M, Ramseier CA, Sculean A, Salvi GE (2021) Clinical and radiographic evaluation of implant-supported single-unit crowns with cantilever extension in posterior areas: A retrospective study with a follow-up of at least 10 years. Clin Implant Dent Relat Res 23:189–196. https://doi.org/10.1111/cid.12973
Tan WL, Wong TL, Wong MC, Lang NP (2012) A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implants Res 23(Suppl 5):1–21. https://doi.org/10.1111/j.1600-0501.2011.02375.x
Arora H, Khzam N, Roberts D, Bruce WL, Ivanovski S (2017) Immediate implant placement and restoration in the anterior maxilla: Tissue dimensional changes after 2–5 year follow up. Clin Implant Dent Relat Res 19:694–702. https://doi.org/10.1111/cid.12487
Bhola M, Neely AL, Kolhatkar S (2008) Immediate implant placement: clinical decisions, advantages, and disadvantages. J Prosthodont 17:576–581. https://doi.org/10.1111/j.1532-849X.2008.00359.x
Clementini M, Tiravia L, De Risi V, Vittorini Orgeas G, Mannocci A, de Sanctis M (2015) Dimensional changes after immediate implant placement with or without simultaneous regenerative procedures: a systematic review and meta-analysis. J Clin Periodontol 42:666–677. https://doi.org/10.1111/jcpe.12423
Esposito M, Grusovin MG, Polyzos IP, Felice P, Worthington HV (2010) Timing of implant placement after tooth extraction: immediate, immediate-delayed or delayed implants? A Cochrane systematic review. Eur J Oral Implantol 3:189–205
Esposito M, Grusovin MG, Polyzos IP, Felice P, Worthington HV (2010) Interventions for replacing missing teeth: dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants). Cochrane Database Syst Rev CD005968. https://doi.org/10.1002/14651858.CD005968.pub3
Esposito M, Zucchelli G, Cannizzaro G, Checchi L, Barausse C, Trullenque-Eriksson A, Felice P (2017) Immediate, immediate-delayed (6 weeks) and delayed (4 months) post-extractive single implants: 1-year post-loading data from a randomised controlled trial. Eur J Oral Implantol 10:11–26
Monje A, Roccuzzo A, Buser D, Wang HL (2023) Influence of buccal bone wall thickness on the peri-implant hard and soft tissue dimensional changes: A systematic review. Clin Oral Implants Res. https://doi.org/10.1111/clr.14029
Hodosh M, Povar M, Shklar G (1969) The dental polymer implant concept. J Prosthet Dent 22:371–380. https://doi.org/10.1016/0022-3913(69)90200-5
Hodosh M, Montagna W, Povar M, Shklar G (1964) Implants of Acrylic Teeth in Human Beings and Experimental Animals; Clinical and Microscopic Studies. Oral Surg Oral Med Oral Pathol 18:569–579. https://doi.org/10.1016/0030-4220(64)90053-2
Lundgren D, Rylander H, Andersson M, Johansson C, Albrektsson T (1992) Healing-in of root analogue titanium implants placed in extraction sockets. An experimental study in the beagle dog. Clin Oral Implants Res 3:136–143. https://doi.org/10.1034/j.1600-0501.1992.030306.x
Strub JR, Kohal RJ, Klaus G, Ferraresso F (1997) The Re Implant system for immediate implant placement. J Esthet Dent 9:187–196. https://doi.org/10.1111/j.1708-8240.1997.tb00940.x
Pirker W, Kocher A (2009) Immediate, non-submerged, root-analogue zirconia implants placed into single-rooted extraction sockets: 2-year follow-up of a clinical study. Int J Oral Maxillofac Surg 38:1127–1132. https://doi.org/10.1016/j.ijom.2009.07.008
Moin DA, Hassan B, Mercelis P, Wismeijer D (2013) Designing a novel dental root analogue implant using cone beam computed tomography and CAD/CAM technology. Clin Oral Implants Res 24(Suppl A100):25–27. https://doi.org/10.1111/j.1600-0501.2011.02359.x
Böse MWH, Hildebrand D, Beuer F, Wesemann C, Schwerdtner P, Pieralli S, Spies BC (2020) Clinical outcomes of root-analogue implants restored with single crowns or fixed dental prostheses: a retrospective case series. J Clin Med 9. https://doi.org/10.3390/jcm9082346
Dantas T, Madeira S, Gasik M, Vaz P, Silva F (2021) Customized root-analogue implants: a review on outcomes from clinical trials and case reports. Materials (Basel) 14. https://doi.org/10.3390/ma14092296
Aldesoki M, Keilig L, Dorsam I, Evers-Dietze B, Elshazly TM, Bourauel C (2023) Trueness and precision of milled and 3D printed root-analogue implants: A comparative in vitro study. J Dent 130:104425. https://doi.org/10.1016/j.jdent.2023.104425
Akkoyun EF, Demirbas AE, Gumus HO, Alkan BA, Alkan A (2022) Custom-made root analog immediate dental implants: a prospective clinical study with 1-year follow-up. Int J Oral Maxillofac Implants 37:1223–1231. https://doi.org/10.11607/jomi.7198
Zhao B, Liu C, Sun Z, Zhao X, Hu M (2022) Evaluation of root-analog implants and standardized specimens fabricated by selective laser melting. Int J Oral Maxillofac Implants 37:1176–1185. https://doi.org/10.11607/jomi.9632
Liu C, Huang S, Guo F, Li Y, Zhao B, Luo A, Liu H, Wang C, Hu M, Zhou H (2022) Immediate, non-submerged, three-dimensionally printed, one-piece mandibular molar porous root-analogue titanium implants: A 2-year prospective study involving 18 patients. J Stomatol Oral Maxillofac Surg 123:e770–e776. https://doi.org/10.1016/j.jormas.2022.05.019
Liu M, Wang Y, Zhang S, Wei Q, Li X (2022) Success factors of additive manufactured root analogue implants. ACS Biomater Sci Eng 8:360–378. https://doi.org/10.1021/acsbiomaterials.1c01079
Mangano FG, De Franco M, Caprioglio A, Macchi A, Piattelli A, Mangano C (2014) Immediate, non-submerged, root-analogue direct laser metal sintering (DLMS) implants: a 1-year prospective study on 15 patients. Lasers Med Sci 29:1321–1328. https://doi.org/10.1007/s10103-013-1299-0
Pessanha-Andrade M, Sordi MB, Henriques B, Silva FS, Teughels W, Souza JCM (2018) Custom-made root-analogue zirconia implants: A scoping review on mechanical and biological benefits. J Biomed Mater Res B Appl Biomater 106:2888–2900. https://doi.org/10.1002/jbm.b.34147
Schatzle M, Land NP, Anerud A, Boysen H, Burgin W, Loe H (2001) The influence of margins of restorations of the periodontal tissues over 26 years. J Clin Periodontol 28:57–64. https://doi.org/10.1034/j.1600-051x.2001.280109.x
Ingber JS, Rose LF, Coslet JG (1977) The “biologic width”–a concept in periodontics and restorative dentistry. Alpha Omegan 70:62–65
Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M (2012) Ferrule effect: a literature review. J Endod 38:11–19. https://doi.org/10.1016/j.joen.2011.09.024
Naumann M, Schmitter M, Frankenberger R, Krastl G (2018) “Ferrule comes first. Post is second!” Fake news and alternative facts? A systematic review. J Endod 44:212–219. https://doi.org/10.1016/j.joen.2017.09.020
Baima RF (1986) Extension of clinical crown length. J Prosthet Dent 55:547–551. https://doi.org/10.1016/0022-3913(86)90029-6
Heithersay GS (1973) Combined endodontic-orthodontic treatment of transverse root fractures in the region of the alveolar crest. Oral Surg Oral Med Oral Pathol 36:404–415. https://doi.org/10.1016/0030-4220(73)90220-x
Bruhnke M, Beuer F, Bose MWH, Naumann M (2022) Forced orthodontic extrusion to restore extensively damaged anterior and premolar teeth as abutments for single-crown restorations: Up to 5-year results from a pilot clinical study. J Prosthet Dent. https://doi.org/10.1016/j.prosdent.2022.08.033
Krastl G, Filippi A, Zitzmann NU, Walter C, Weiger R (2011) Current aspects of restoring traumatically fractured teeth. Eur J Esthet Dent 6:124–141
Bach N, Baylard JF, Voyer R (2004) Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc 70:775–780
Simon JH (1984) Root extrusion. Rationale and techniques. Dent Clin North Am 28:909–921
Bruhnke M, Bitter K, Beuer F, Bose MWH, Neumeyer S, Naumann M (2022) Tooth preservation of deeply destroyed teeth by forced orthodontic extrusion: A case series. Quintessence Int 0:2–11. https://doi.org/10.3290/j.qi.b2644901
Malmgren O, Malmgren B, Frykholm A (1991) Rapid orthodontic extrusion of crown root and cervical root fractured teeth. Endod Dent Traumatol 7:49–54. https://doi.org/10.1111/j.1600-9657.1991.tb00183.x
Ziskind D, Schmidt A, Hirschfeld Z (1998) Forced eruption technique: rationale and clinical report. J Prosthet Dent 79:246–248. https://doi.org/10.1016/s0022-3913(98)70231-8
Murchison DF, Schwartz RS (1986) The use of removable appliances for forced eruption of teeth. Quintessence Int 17:497–501
Lythgoe JR, Torabinejad M, Simon JH (1980) Extrusion techniques for the general dentist. Gen Dent 28(42–43):46–49
Molina DG (1984) Using a complete denture for extrusion. Gen Dent 32:247–249
Bruhnke M, Beuer F, Bose MWH, Naumann M (2023) Forced orthodontic extrusion to restore extensively damaged anterior and premolar teeth as abutments for single-crown restorations: Up to 5-year results from a pilot clinical study. J Prosthet Dent 129:61–68. https://doi.org/10.1016/j.prosdent.2022.08.033
Carvalho CV, Bauer FP, Romito GA, Pannuti CM, De Micheli G (2006) Orthodontic extrusion with or without circumferential supracrestal fiberotomy and root planing. Int J Periodontics Restorative Dent 26:87–93
Joda T, Ferrari M, Bragger U (2017) A prospective clinical cohort study analyzing single-unit implant crowns after three years of loading: introduction of a novel functional implant prosthodontic score (FIPS). Clin Oral Implants Res 28:1291–1295. https://doi.org/10.1111/clr.12955
Joda T, Zarone F, Zitzmann NU, Ferrari M (2018) The Functional Implant Prosthodontic Score (FIPS): assessment of reproducibility and observer variability. Clin Oral Investig 22:2319–2324. https://doi.org/10.1007/s00784-017-2332-7
Krug R, Connert T, Soliman S, Syfrig B, Dietrich T, Krastl G (2018) Surgical extrusion with an atraumatic extraction system: A clinical study. J Prosthet Dent 120:879–885. https://doi.org/10.1016/j.prosdent.2018.02.006
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22:276–282
Chaushu S, Zahavi T, Becker A (2004) Forced eruption of maxillary incisor teeth from the lingual side. Quintessence Int 35:431–436
Felippe LA, Monteiro Junior S, Vieira LC, Araujo E (2003) Reestablishing biologic width with forced eruption. Quintessence Int 34:733–738
Kim SH, Tramontina VA, Papalexiou V, Luczyszyn SM, Grassi MB, de Fatima Scarpim M, Tanaka OM (2011) Rapid orthodontic extrusion using an interocclusal appliance for the reestablishment of biologic width: a case report. Quintessence Int 42:201–204
Mangano FG, Cirotti B, Sammons RL, Mangano C (2012) Custom-made, root-analogue direct laser metal forming implant: a case report. Lasers Med Sci 27:1241–1245. https://doi.org/10.1007/s10103-012-1134-z
Pirker W, Kocher A (2008) Immediate, non-submerged, root-analogue zirconia implant in single tooth replacement. Int J Oral Maxillofac Surg 37:293–295. https://doi.org/10.1016/j.ijom.2007.11.008
Pirker W, Kocher A (2011) Root analog zirconia implants: true anatomical design for molar replacement–a case report. Int J Periodontics Restorative Dent 31:663–668
Pirker W, Wiedemann D, Lidauer A, Kocher AA (2011) Immediate, single stage, truly anatomic zirconia implant in lower molar replacement: a case report with 2.5 years follow-up. Int J Oral Maxillofac Surg 40:212–216. https://doi.org/10.1016/j.ijom.2010.08.003
Pontoriero R, Celenza F Jr, Ricci G, Carnevale G (1987) Rapid extrusion with fiber resection: a combined orthodontic-periodontic treatment modality. Int J Periodontics Restorative Dent 7:30–43
Saeidi Pour R, Randelzhofer P, Edelhoff D, Prandtner O, Rafael CF, Liebermann A (2017) Innovative single-tooth replacement with an individual root-analog hybrid implant in the esthetic zone: case report. Int J Oral Maxillofac Implants 32:e153–e160. https://doi.org/10.11607/jomi.5562
Schubert O, Beuer F, Guth JF, Nold E, Edelhoff D, Metz I (2018) Two digital strategies in modern implantology - root-analogue implants and the digital one-abutment/one-time concept. Int J Comput Dent 21:115–131
Zyskind K, Zyskind D, Soskolne WA, Harary D (1992) Orthodontic forced eruption: case report of an alternative treatment for subgingivally fractured young permanent incisors. Quintessence Int 23:393–399
Figliuzzi MM, Aiello D, Rengo C, Parentela L, Mangano C (2022) 10-year evaluation of the first root analogue implant on humans, made Using a CT scan, CAD/CAM and DMLS. Biomimetics (Basel) 7. https://doi.org/10.3390/biomimetics7010032
Belser UC, Grutter L, Vailati F, Bornstein MM, Weber HP, Buser D (2009) Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol 80:140–151. https://doi.org/10.1902/jop.2009.080435
Furhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G (2005) Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res 16:639–644. https://doi.org/10.1111/j.1600-0501.2005.01193.x
Cvar JF, Ryge G (2005) Reprint of criteria for the clinical evaluation of dental restorative materials. Clin Oral Investig 9:215–232. https://doi.org/10.1007/s00784-005-0018-z
Chappuis V, Avila-Ortiz G, Araujo MG, Monje A (2018) Medication-related dental implant failure: Systematic review and meta-analysis. Clin Oral Implants Res 29(Suppl 16):55–68. https://doi.org/10.1111/clr.13137
Chen H, Liu N, Xu X, Qu X, Lu E (2013) Smoking, radiotherapy, diabetes and osteoporosis as risk factors for dental implant failure: a meta-analysis. PLoS One 8:e71955. https://doi.org/10.1371/journal.pone.0071955
Beikler T, Flemmig TF (2015) EAO consensus conference: economic evaluation of implant-supported prostheses. Clin Oral Implants Res 26(Suppl 11):57–63. https://doi.org/10.1111/clr.12630
Jemt T, Ahlberg G, Henriksson K, Bondevik O (2006) Changes of anterior clinical crown height in patients provided with single-implant restorations after more than 15 years of follow-up. Int J Prosthodont 19:455–461
Thilander B, Odman J, Lekholm U (2001) Orthodontic aspects of the use of oral implants in adolescents: a 10-year follow-up study. Eur J Orthod 23:715–731. https://doi.org/10.1093/ejo/23.6.715
Malloy KA, Wadhwani C, McAllister B, Wang M, Katancik JA (2017) Accuracy and reproducibility of radiographic images for assessing crestal bone height of implants using the precision implant X-ray locator (PIXRL) device. Int J Oral Maxillofac Implants 32:830–836. https://doi.org/10.11607/jomi.5683
Walton TR, Layton DM (2018) Intra- and inter-examiner agreement when assessing radiographic implant bone levels: Differences related to brightness, accuracy, participant demographics and implant characteristics. Clin Oral Implants Res 29:756–771. https://doi.org/10.1111/clr.13290
Alsahhaf A, Att W (2016) Orthodontic extrusion for pre-implant site enhancement: Principles and clinical guidelines. J Prosthodont Res 60:145–155. https://doi.org/10.1016/j.jpor.2016.02.004
Acknowledgements
This investigation was supported by clinical data from the private dental office of Dr. Detlef Hildebrand in Berlin, Germany and product specific data provided by former company NDI Berlin in Berlin, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
M.W.H.B.: Conception and design, acquisition, analysis and interpretation of data, drafting the manuscript, giving final approval; F.B.: Conception and design, interpretation of data, revising the manuscript, giving final approval; M.N.: Conception and design, interpretation of data, revising the manuscript, giving final approval; B.C.S.: Conception and design, interpretation of data, revising the manuscript, giving final approval; S.N.: analysis and interpretation of data, revising the manuscript, giving final approval; D.H.: acquisition and analysis of data, revising the manuscript, giving final approval; M.B.: Conception and design, acquisition, analysis and interpretation of data, drafting the manuscript, giving final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was given by the local Ethical Committee of Charité – Universitätsmedizin Berlin, Germany (application numbers: EA4/140/18 and EA2/301/20). All patients have received and signed a written informed consent form and patient information.
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Böse, M.W.H., Beuer, F., Naumann, M. et al. Root-analogue implants compared to forced orthodontic extrusion: a retrospective analysis of clinical, radiological and esthetic outcomes after restoration. Clin Oral Invest 27, 5875–5886 (2023). https://doi.org/10.1007/s00784-023-05198-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05198-6