Abstract
Objective
This study aims to review the role of the oral cavity in SARS-CoV-2- and other viral upper respiratory tract infections.
Material and methods
Data reviewed in the text have been researched online and also reflect personal expertise.
Results
Numerous respiratory and other viruses replicate in the oral cavity and are transmitted via aerosols (< 5 µm) and droplets (> 5 µm). SARS-CoV-2 replication has been documented in the upper airways as well as in oral mucosa and salivary glands. These sites are also virus reservoirs that can infect other organs, e.g., the lungs and gastrointestinal tract, as well as other individuals. Laboratory diagnosis of viruses in the oral cavity and upper airways focuses on real-time PCR; antigen tests are less sensitive. For screening and monitoring infections, nasopharyngeal and oral swabs are tested; saliva is a good and more comfortable alternative. Physical means like social distancing or masks have been proven successful to reduce the risk of infection. Both wet-lab and clinical studies confirm that mouth rinses are effective against SARS-CoV-2 and other viruses. Antiviral mouth rinses can inactivate all viruses that replicate in the oral cavity.
Conclusions
The oral cavity plays an important role in viral infections of the upper respiratory tract: it serves as a portal of entry, a site of replication, and a source of infection by droplets and aerosols. Physical means but also antiviral mouth rinses can help reduce the spread of viruses and contribute to infection control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has caused one of the largest pandemics in human history. This has been possible because of a specific viral feature: its high transmissibility at the pandemic onset end of 2019. During one infection, the virus was passed to 3.6 to 6 others in a susceptible population in a European setting, measured by the basic reproductive number R0 [1]. During the last 3 years, even better transmissible variants have evolved [2]. As a respiratory virus, SARS-CoV-2 spreads through droplets and aerosols, which are emitted during normal breathing, but to a much higher extent during speaking, singing, coughing, and sneezing. As the oral cavity is anatomically and functionally involved in these processes, it is conceivable that it plays a paramount role in SARS-CoV-2 transmission. Thus, a better understanding of the oral cavity as an entry point and reservoir of SARS-CoV-2 and other viruses is critical for infection control. In this review, both epidemiology and wet-lab data will be critically discussed and put into a medical context.
Viral infections and transmission through the respiratory tract and oral cavity
Respiratory viruses infect susceptible individuals through droplets and aerosols that reach mucous membranes of the upper respiratory tract and oral cavity. Airborne liquid particles > 5 µm are considered droplets, < 5 µm aerosols. Even though size influences the fate of airborne particles, the 5-µm threshold has been defined artificially [3]. Airborne particle size usually decreases by evaporation or can increase by coalescence. Aerosols remain suspended in the air for several hours, particularly when their size decreases quickly in dry air. Larger droplets sink to surfaces in minutes, particularly in humid air [3]. SARS-CoV-2 stays infectious in droplets and aerosols with a half-life of 1 h [4, 5].
Droplets and aerosols expelled during breathing and talking originate mainly from the respiratory tract [6]. During dental procedures, droplets and aerosols naturally emerge from the oral cavity. Thus, preprocedural antiviral mouth rinses are expected to reduce infectious virions in those aerosols.
Aerosols are more likely to be inhaled deeper, thus reaching lower portions of the respiratory tract than larger droplets. The cellular SARS-CoV-2 receptors ACE2 and TMPRSS have been well-characterized and detected in oral mucosa, including the tongue, gingival tissue, and salivary glands [7]. Influenza virus replication was detected in several tissues of ferrets, as soft palate, nasal cavity, and lungs [8]. While other respiratory viruses, as RSV, metapneumo- or parainfluenza viruses replicate mainly in the respiratory epithelia, influenza viruses and SARS-CoV-2 infect multiple tissues, sometimes causing clinical illness in other organs. Examples are myocarditis as a complication of influenza viremia and SARS-CoV-2 infection of endothelial cells, possibly causing thrombosis.
SARS-CoV-2
As a beta coronavirus, SARS-CoV-2 resembles SARS-CoV that caused an epidemic in Asia in 2003 [9]. The human coronaviruses (hCoV) HKU1 and OC43 also belong to the beta genus and are among the most frequent causes for common colds [10]. Other common cold viruses are types NL63 and 229E, which belong to the alpha genus. All four types are endemic worldwide and are detected with similar frequencies [11]. The SARS-CoV-2 genome comprises around 30,000 nucleotides and encodes numerous proteins [12]. They orchestrate viral replication, including cell entry and egress. The relatively big and complex genome requires a proof-reading polymerase to keep it stable. Even though it reduces the SARS-CoV-2 mutation rate, it is estimated that the virus accumulates 33 genome mutations per year [13]. This is also due to the exceedingly high number of infected subjects, each harboring 109 to 1011 virions at the peak of infection [14].
From the upper respiratory tract and oral cavity, SARS-CoV-2 can spread to lower respiratory tissues and other organs, as the gastrointestinal tract or blood vessels.
SARS-CoV-2 and COVID-19
SARS-CoV-2 is associated with multiple clinical symptoms, summarized as coronavirus disease 2019 (COVID-19). It is antigenically distinct enough from endemic human coronaviruses to render the entire human population susceptible, thus causing one of the largest pandemics ever. Several features are characteristic for SARS-CoV-2 compared to other respiratory viruses:
-
Pandemic spread with prevalence varying in waves.
-
New variants emerging and replacing previous ones on a global level.
-
Replication in gingival tissue and salivary glands has been documented.
-
Various cell types can be infected in cell culture, facilitating systemic infection.
-
Sequelae in various organs, e.g., the blood vessels, lungs, heart, kidneys.
-
Generalized symptomatic complications as multisystem inflammatory syndrome and long COVID-19.
Differing from other respiratory viruses, SARS-CoV-2 has been circulating in waves but has never fully disappeared during the last 3 years. This has been due to a novel and pandemic virus that differed antigenically enough from other hCoV to encounter an immunologically naïve population. With SARS-CoV-2 becoming endemic and facing substantial herd immunity, it will likely virtually disappear in the summer months as other respiratory viruses.
Several variants have emerged during the last 3 years. Four of them have been designated “variants of concern” by the World Health Organization (WHO). Particularly, the alpha, delta, and omicron variants have quickly replaced previous variants, due to immune escape or higher replication capacity.
Compared to other respiratory viruses, SARS-CoV-2 is transmitted very efficiently between humans. In early stages of the pandemic, SARS-CoV-2 was considered to be transmitted by close contacts, droplets, and fomites; aerosols came into the focus later [15].
When SARS-CoV-2 is inhaled through aerosols, it infects epithelial cells of the upper respiratory mucous membranes. Previous studies indicate that SARS-CoV-2 also enters the human body via the oral cavity and readily replicates there [16]. Viral RNA detected in salivary glands is a result of in situ viral replication and cannot stem from the upper respiratory tract for anatomic reasons. Moreover, cellular SARS-CoV-2 receptors ACE2 and TMPRSS have been detected in oral mucosa, including the tongue, gingival tissue, and salivary glands [7]. Huang et al. confirmed oral SARS-CoV-2 infection by in situ hybridization and susceptibility by RNA single-cell sequencing. Saliva, even from asymptomatic persons, was found to infect culture cells ex vivo [17].
SARS-CoV-2 RNA has been detected in several tissues [18, 19]. Accordingly, various cell types, as respiratory and intestinal can be infected [20, 21]
Sequelae in various organs have been documented, and they increased in reinfected people [22].
Long COVID-19 implies symptoms lasting longer than the acute infection phase of 4 weeks (https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Long-COVID/Inhalt-gesamt.html). Main symptoms are fatigue, chest pain, dyspnea, and cough [23]. Objective diagnostic criteria for long COVID-19 are not available, so diagnoses rely mainly on subjective symptoms. Distinct etiologies of long-term sequelae have been established by transcriptome-wide investigation [24]. Clinical signs of SARS-CoV-2 replication in the oral cavity, like discoloration, ulceration, and hemorrhage have been reported in long COVID-19 patients [25].Oral lesions can correlate to other long COVID-19 symptoms and are thus of diagnostic value in routine patient care.
Another COVID-19 complication is multisystem inflammatory syndrome. It can occur in children [26, 27] and adults with divergent pathologies [28, 29].
SARS-CoV-2 laboratory diagnosis and the importance of the oral cavity in its diagnosis
Most commonly, SARS-CoV-2 is detected in nasopharyngeal swabs by nucleic acid tests, usually real-time PCR. The resulting threshold cycle (Ct) values are frequently translated in viral loads. Viral loads or Ct values have been used as a basis for hygiene management. PCRs cannot differentiate infectious viral particles from non-infectious viral particles or RNA fragments. Infectious viral particles can only be detected in permissive cell culture. Such cell culture systems have been established; they reliably cultivate infectious virus from patient samples [30]. More than 7 days after initial positive PCR, no infectious SARS-CoV-2 can be detected in most patients anymore, even under immune suppression [31]. However, these procedures are too time-consuming for routine diagnostics. Antibodies directed to SARS-CoV-2 are detected with enzyme immune assays and pseudo-neutralization assays. The presence of neutralizing antibodies in vulnerable patients can impact further treatment options.
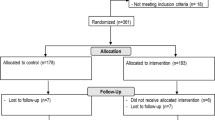
Figure 1 shows the trajectory of infectious virus and RNA load in different compartments and antibodies.
Detection of infectious virus-, RNA, and antibodies during the course of SARS-CoV-2 infection [51]
Around 8–10 days after symptom onset, antibody responses become detectable. In most cases, viral particles are neutralized at this time; thus, infectious virions cannot be detected anymore. At the same time, total RNA begins to decline. Thus, RNA load trajectories and neutralizing antibodies are taken into account to assess if a person is considered infectious. Figure 1 also illustrates that in later infection stages, RNA load can be low or undetectable in nasopharyngeal swabs while still high in bronchoalveolar lavage or sputum. In reinfections, trajectories can vary with lower RNA loads [32] and earlier immune responses.
Since deep nasopharyngeal swabs cause discomfort, alternative sample types have been sought. Saliva and oropharyngeal swabs offer similar sensitivities and easier sampling [33, 34]. This applies to a screening setting [35] and to asymptomatic adults such with mild COVID-19 symptoms [36]. The authors report 4.12 log10 copies/mL initial viral load. Personal experience confirms that saliva samples suit well for screening opera staff for SARS-CoV-2 infections (manuscript in preparation).
Other viruses infecting the oral cavity
Respiratory viruses
Influenza-, parainfluenza-, metapneumo-, rhino-, adeno-, and respiratory syncytial viruses are also transmitted by aerosols and droplets, as well as direct and indirect contact (fomites). Reproductive numbers R lie between 1 and 5. Thus, they are lower than the basic R of SARS-CoV-2 at the pandemic start with naïve populations. Influenza viruses, particularly A strains, typically cause more severe illnesses with sudden onset. Respiratory viruses normally replicate only in the epithelial cells of the upper respiratory tract and rarely infect other organs or are detected in blood. However, they may infect lower respiratory tissues in immunocompromised patients, causing atypical pneumonia. With multiplex PCR tests being more frequently employed, respiratory viruses are increasingly detected. Currently, we gain experience what clinical implications that has depending on patient characteristics. Influenza viruses more frequently generalize and cause pneumonia or myocarditis even in persons without pronounced immune deficiency.
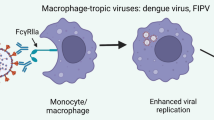
Other viruses affecting the oral mucosa
Enteroviruses, as well as cytomegalovirus (CMV), Epstein–Barr virus (EBV), herpes simplex virus (HSV), and varicella-zoster virus (VZV), infect epithelial cells of the oral cavity. Unlike than respiratory viruses, they cause more specific lesions like ulcers and blisters (Figs. 2 and 3). The oral cavity is the main entry region of these viruses, from where they spread to other tissues and organs. High viral loads are present in primary infection, e.g., EBV mononucleosis and stomatitis herpetica (Fig. 3). Local EBV reactivations in the oral mucosa are usually asymptomatic in immunocompetent persons and can still infect seronegative persons through infectious droplets.
Enterovirus type A infection “hand foot mouth disease” (Altmeyers Enzyklopädie, www.altmeyers.org)
Herpes simplex virus stomatitis (Altmeyers Enzyklopädie, www.altmeyers.org)
Measles, mumps, and rubella typically occur in unvaccinated children and young adults. They are highly contagious with R0 reaching 10 in susceptible populations. The best prophylaxis is a double immunization with live attenuated vaccines. If lesions in the oral cavity occur, they are unspecific and hard to interpret (e.g., Koplick spots indicating measles).
Human papillomaviruses (HPV) differ from the above in host infection, where the latter infect chronically, but not necessarily for life. High-risk HPV have been increasingly detected in the oral cavity [37]. Consequently, the incidence for HPV related cancers of the oral cavity rises worldwide, even in younger populations [38]. HPV are transmitted by direct and prolonged contact, e.g., kissing and sexual activities. They persist for several months to years after primary infection. HPV vaccines elicit specific IgG antibodies in saliva and thus can protect individuals from new HPV infections [39]. HPV DNA in saliva could serve as a tumor marker for HPV-induced head and neck cancers [40].
Diagnosis of viral infections of the oral cavity
Most viruses replicating in the oral cavity do not cause visible lesions. Laboratory diagnosis is important, preferably carried out by real-time PCR. Antigen tests are less sensitive [41, 42] as they do not amplify viral antigenic proteins. Pathognomonic lesion, e.g., Koplick spots, can lead to an immediate diagnosis. Swabs from affected areas offer a good sensitivity. Without obvious lesions, oral rinses or saliva are good alternatives as they come into contact with most of the mucous membrane tissue. Some viruses, e.g., herpesviruses, can replicate independently in different body sites. Thus, detecting CMV in the oral cavity does not establish the diagnosis of a CMV pneumonia but hints at a CMV mucositis. In fact, particularly EBV but also other herpesviruses can be detected in immunocompetent individuals without mucosal abnormalities [43]. On the other hand, a positive PCR detection of respiratory virus in the oral cavity clearly indicates an active infection with viral replication. Influenza/RS viruses were detected at similar rates in saliva and nasopharyngeal aspirates of patients with respiratory infections [44, 45]. Testing of saliva samples, in addition to nasopharyngeal specimen, was reported to detect more respiratory viruses than nasopharyngeal specimen alone [46]. Thus, saliva seems suitable not only for detecting SARS-CoV-2 and influenza viruses but also for other respiratory viruses (adeno-, metapneumo- parainfluenza-, and RS viruses). Being a notorious source of droplets and aerosols, the oral cavity plays an important role in transmitting respiratory viruses.
General measures against COVID-19 and other infections transmitted via the upper respiratory tract and the oral cavity
Pharmaceutical interventions, e.g., vaccines or antiviral drugs, are distinguished from non-pharmaceutical interventions which consist of contact prevention, i.e., self-isolation and quarantines, contact tracing, triage of patients with respiratory symptoms, and masks.
If used for treatment, antiviral drugs require a virological diagnosis. Alternatively, they can be used for prophylaxis to prevent viral replication.
Vaccines do not directly inhibit viral replication but trigger the host’s immune system to mount an antibody and T cell response against a pathogen. Usually, they are administered as a prophylaxis to prevent or alleviate an infection, but they can also boost the host’s immune response during a chronic infection and thus help treat it (therapeutic vaccination).
Non-pharmaceutical interventions do not require a virological diagnosis, as they work for all viruses. Social distancing limits the spread of every pathogen. Most human pathogenic viruses are transmitted by aerosols and larger droplets. Thus, face masks are effective barriers.
Virological and clinical effects of mouth rinses
There are two different ways of studying the impact of antiviral mouth rinses:
-
1.
Assay with stable cell culture system whether rinsing reduces infectious viral particles.
-
2.
Assess the effect of mouth rinses in controlled clinical studies.
Numerous antiviral components have inhibited coronavirus replication in high-throughput screening assays [47]. For example, cetylpyridinium chloride (CPC) is active against the hCoV strains OC43, NL63, and MERS. Commercially available mouth rinses inhibited hCoV infectiousness for Huh7 cells by up to 99.9% [48]. Virucidal assays showed that chlorhexidine was effective against influenza- and parainfluenza-, herpes simplex-, and cytomegalovirus in 30 s [49].
A CPC formulation significantly reduced cold symptoms in a randomized placebo-controlled double-blind trial with 94 participants [50]. Three control individuals were tested PCR positive for respiratory viruses, whereas no test person was positive. These encouraging results warrant larger multi-center studies. The effect of preprocedural mouth rinses in a dentist setting is discussed separately in this supplement by J. Weber et al.
Conclusions
The SARS-CoV-2 pandemic has boosted research in viral transmission and expedited our understanding of viral replication in the oral cavity. Respiratory viruses causing acute infections as well as herpes- and papillomaviruses infecting the host chronically are transmitted through aerosols and droplets. The oral cavity is an important reservoir of many viruses and thus a source of infection. Reducing the pathogens at the site of their multiplication, i.e., in the oral cavity, through the use of antiviral mouth rinses can, at least temporarily, reduce the viral load in aerosols and droplets.
Even though the COVID-19 pandemic caused tremendous suffering, the lessons learned make us much better prepared for future pandemics but also for endemic infectious diseases.
Data availability
No specific data other than the cited publications have been used.
References
Ke R, Romero-Severson E, Sanche S, Hengartner N (2021) Estimating the reproductive number R(0) of SARS-CoV-2 in the United States and eight European countries and implications for vaccination. J Theor Biol 517:110621. https://doi.org/10.1016/j.jtbi.2021.110621
Liu Y, Rocklov J (2022) The effective reproductive number of the omicron variant of SARS-CoV-2 is several times relative to Delta. J Travel Med 29. https://doi.org/10.1093/jtm/taac037
Jarvis MC (2020) Aerosol transmission of SARS-CoV-2: physical principles and implications. Front Public Health 8:590041. https://doi.org/10.3389/fpubh.2020.590041
Smither SJ, Eastaugh LS, Findlay JS, Lever MS (2020) Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity. Emerg Microbes Infect 9:1415–1417. https://doi.org/10.1080/22221751.2020.1777906
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382:1564–1567. https://doi.org/10.1056/NEJMc2004973
Edwards DA, Man JC, Brand P, Katstra JP, Sommerer K, Stone HA, Nardell E, Scheuch G (2004) Inhaling to mitigate exhaled bioaerosols. Proc Natl Acad Sci U S A 101:17383–17388. https://doi.org/10.1073/pnas.0408159101
Zhong M, Lin B, Pathak JL, Gao H, Young AJ, Wang X, Liu C, Wu K, Liu M, Chen JM, Huang J, Lee LH, Qi CL, Ge L, Wang L (2020) ACE2 and furin expressions in oral epithelial cells possibly facilitate COVID-19 infection via respiratory and fecal-oral routes. Front Med (Lausanne) 7:580796. https://doi.org/10.3389/fmed.2020.580796
Lakdawala SS, Jayaraman A, Halpin RA, Lamirande EW, Shih AR, Stockwell TB, Lin X, Simenauer A, Hanson CT, Vogel L, Paskel M, Minai M, Moore I, Orandle M, Das SR, Wentworth DE, Sasisekharan R, Subbarao K (2015) The soft palate is an important site of adaptation for transmissible influenza viruses. Nature 526:122–125. https://doi.org/10.1038/nature15379
Enserink M (2013) SARS: chronology of the epidemic. Science 339:1266–1271. https://doi.org/10.1126/science.339.6125.1266
Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, Liu W, Bi Y, Gao GF (2016) Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 24:490–502. https://doi.org/10.1016/j.tim.2016.03.003
Killerby ME, Biggs HM, Haynes A, Dahl RM, Mustaquim D, Gerber SI, Watson JT (2018) Human coronavirus circulation in the United States 2014–2017. J Clin Virol 101:52–56. https://doi.org/10.1016/j.jcv.2018.01.019
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ (2020) A new coronavirus associated with human respiratory disease in China. Nature 579:265–269. https://doi.org/10.1038/s41586-020-2008-3
Candido DS, Claro IM, de Jesus JG, Souza WM, Moreira FRR, Dellicour S, Mellan TA, du Plessis L, Pereira RHM, Sales FCS, Manuli ER, Theze J, Almeida L, Menezes MT, Voloch CM, Fumagalli MJ, Coletti TM, da Silva CAM, Ramundo MS, Amorim MR, Hoeltgebaum HH, Mishra S, Gill MS, Carvalho LM, Buss LF, Prete CA Jr, Ashworth J, Nakaya HI, Peixoto PS, Brady OJ, Nicholls SM, Tanuri A, Rossi AD, Braga CKV, Gerber AL, de Guimarães APC, Gaburo N Jr, Alencar CS, Ferreira ACS, Lima CX, Levi JE, Granato C, Ferreira GM, Francisco RS Jr, Granja F, Garcia MT, Moretti ML, Perroud MW Jr, Castineiras T, Lazari CS, Hill SC, de Souza Santos AA, Simeoni CL, Forato J, Sposito AC, Schreiber AZ, Santos MNN, de Sa CZ, Souza RP, Resende-Moreira LC, Teixeira MM, Hubner J, Leme PAF, Moreira RG, Nogueira ML, Brazil-Uk Centre for Arbovirus Discovery DG, Epidemiology Genomic Network, Ferguson NM, Costa SF, Proenca-Modena JL, Vasconcelos ATR, Bhatt S, Lemey P, Wu CH, Rambaut A, Loman NJ, Aguiar RS, Pybus OG, Sabino EC, Faria NR (2020) Evolution and epidemic spread of SARS-CoV-2 in Brazil. Science 369:1255–1260. https://doi.org/10.1126/science.abd2161
Sender R, Bar-On YM, Gleizer S, Bernshtein B, Flamholz A, Phillips R, Milo R (2021) The total number and mass of SARS-CoV-2 virions. Proc Natl Acad Sci U S A 118. https://doi.org/10.1073/pnas.2024815118
Tang S, Mao Y, Jones RM, Tan Q, Ji JS, Li N, Shen J, Lv Y, Pan L, Ding P, Wang X, Wang Y, MacIntyre CR, Shi X (2020) Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ Int 144:106039. https://doi.org/10.1016/j.envint.2020.106039
Drozdzik A, Drozdzik M (2022) Oral pathology in COVID-19 and SARS-CoV-2 infection-molecular aspects. Int J Mol Sci 23. https://doi.org/10.3390/ijms23031431
Huang N, Perez P, Kato T, Mikami Y, Okuda K, Gilmore RC, Conde CD, Gasmi B, Stein S, Beach M, Pelayo E, Maldonado JO, Lafont BA, Jang SI, Nasir N, Padilla RJ, Murrah VA, Maile R, Lovell W, Wallet SM, Bowman NM, Meinig SL, Wolfgang MC, Choudhury SN, Novotny M, Aevermann BD, Scheuermann RH, Cannon G, Anderson CW, Lee RE, Marchesan JT, Bush M, Freire M, Kimple AJ, Herr DL, Rabin J, Grazioli A, Das S, French BN, Pranzatelli T, Chiorini JA, Kleiner DE, Pittaluga S, Hewitt SM, Burbelo PD, Chertow D, Consortium NC-A, Oral HCA, Craniofacial Biological Network, Frank K, Lee J, Boucher RC, Teichmann SA, Warner BM, Byrd KM (2021) SARS-CoV-2 infection of the oral cavity and saliva. Nat Med 27:892–903. https://doi.org/10.1038/s41591-021-01296-8
Casagrande M, Fitzek A, Spitzer M, Puschel K, Glatzel M, Krasemann S, Aepfelbacher M, Norz D, Lutgehetmann M, Pfefferle S, Schultheiss M (2022) Detection of SARS-CoV-2 genomic and subgenomic RNA in retina and optic nerve of patients with COVID-19. Br J Ophthalmol 106:1313–1317. https://doi.org/10.1136/bjophthalmol-2020-318618
Roden AC, Vrana JA, Koepplin JW, Hudson AE, Norgan AP, Jenkinson G, Yamaoka S, Ebihara H, Monroe R, Szabolcs MJ, Majumdar R, Moyer AM, Garcia JJ, Kipp BR (2021) Comparison of in situ hybridization, immunohistochemistry, and reverse transcription-droplet digital polymerase chain reaction for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing in tissue. Arch Pathol Lab Med 145:785–796. https://doi.org/10.5858/arpa.2021-0008-SA
Lamers MM, Beumer J, van der Vaart J, Knoops K, Puschhof J, Breugem TI, Ravelli RBG, Paul van Schayck J, Mykytyn AZ, Duimel HQ, van Donselaar E, Riesebosch S, Kuijpers HJH, Schipper D, van de Wetering WJ, de Graaf M, Koopmans M, Cuppen E, Peters PJ, Haagmans BL, Clevers H (2020) SARS-CoV-2 productively infects human gut enterocytes. Science 369:50–54. https://doi.org/10.1126/science.abc1669
Salahudeen AA, Choi SS, Rustagi A, Zhu J, van Unen V, de la OS, Flynn RA, Margalef-Catala M, Santos AJM, Ju J, Batish A, Usui T, Zheng GXY, Edwards CE, Wagar LE, Luca V, Anchang B, Nagendran M, Nguyen K, Hart DJ, Terry JM, Belgrader P, Ziraldo SB, Mikkelsen TS, Harbury PB, Glenn JS, Garcia KC, Davis MM, Baric RS, Sabatti C, Amieva MR, Blish CA, Desai TJ, Kuo CJ (2020) Progenitor identification and SARS-CoV-2 infection in human distal lung organoids. Nature 588:670–675. https://doi.org/10.1038/s41586-020-3014-1
Bowe B, Xie Y, Al-Aly Z (2022) Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nat Med 28:2398–2405. https://doi.org/10.1038/s41591-022-02051-3
Cabrera Martimbianco AL, Pacheco RL, Bagattini AM, Riera R (2021) Frequency, signs and symptoms, and criteria adopted for long COVID-19: a systematic review. Int J Clin Pract 75:e14357. https://doi.org/10.1111/ijcp.14357
Thompson RC, Simons NW, Wilkins L, Cheng E, Del Valle DM, Hoffman GE, Cervia C, Fennessy B, Mouskas K, Francoeur NJ, Johnson JS, Lepow L, Le Berichel J, Chang C, Beckmann AG, Wang YC, Nie K, Zaki N, Tuballes K, Barcessat V, Cedillo MA, Yuan D, Huckins L, Roussos P, Marron TU, Mount Sinai C-BT, Glicksberg BS, Nadkarni G, Heath JR, Gonzalez-Kozlova E, Boyman O, Kim-Schulze S, Sebra R, Merad M, Gnjatic S, Schadt EE, Charney AW, Beckmann ND (2022) Molecular states during acute COVID-19 reveal distinct etiologies of long-term sequelae. Nat Med. https://doi.org/10.1038/s41591-022-02107-4
Rafalowicz B, Wagner L, Rafalowicz J (2022) Long COVID oral cavity symptoms based on selected clinical cases. Eur J Dent 16:458–463. https://doi.org/10.1055/s-0041-1739445
Fabi M, Filice E, Biagi C, Andreozzi L, Palleri D, Mattesini BE, Rizzello A, Gabrielli L, Ghizzi C, Di Luca D, Caramelli F, De Fanti A, Lanari M (2021) Multisystem inflammatory syndrome following SARS-CoV-2 infection in children: one year after the onset of the pandemic in a high-incidence area. Viruses 13. https://doi.org/10.3390/v13102022
Miller AD, Zambrano LD, Yousaf AR, Abrams JY, Meng L, Wu MJ, Melgar M, Oster ME, Godfred Cato SE, Belay ED, Campbell AP, Group M-CSA (2022) Multisystem inflammatory syndrome in children-United States, February 2020-July 2021. Clin Infect Dis 75:e1165–e1175. https://doi.org/10.1093/cid/ciab1007
Belay ED, Godfred Cato S, Rao AK, Abrams J, Wyatt Wilson W, Lim S, Newton-Cheh C, Melgar M, DeCuir J, Webb B, Marquez P, Su JR, Meng L, Grome HN, Schlaudecker E, Talaat K, Edwards K, Barnett E, Campbell AP, Broder KR, Bamrah Morris S (2022) Multisystem inflammatory syndrome in adults after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and coronavirus disease 2019 (COVID-19) vaccination. Clin Infect Dis 75:e741–e748. https://doi.org/10.1093/cid/ciab936
Lai CC, Hsu CK, Hsueh SC, Yen MY, Ko WC, Hsueh PR (2022) Multisystem inflammatory syndrome in adults: characteristics, treatment, and outcomes. J Med Virol. https://doi.org/10.1002/jmv.28426
Bullard J, Dust K, Funk D, Strong JE, Alexander D, Garnett L, Boodman C, Bello A, Hedley A, Schiffman Z, Doan K, Bastien N, Li Y, Van Caeseele PG, Poliquin G (2020) Predicting infectious severe acute respiratory syndrome coronavirus 2 from diagnostic samples. Clin Infect Dis 71:2663–2666. https://doi.org/10.1093/cid/ciaa638
Sung A, Bailey AL, Stewart HB, McDonald D, Wallace MA, Peacock K, Miller C, Reske KA, O’Neil CA, Fraser VJ, Diamond MS, Burnham CD, Babcock HM, Kwon JH (2022) Isolation of SARS-CoV-2 in viral cell culture in immunocompromised patients with persistently positive RT-PCR results. Front Cell Infect Microbiol 12:804175. https://doi.org/10.3389/fcimb.2022.804175
Woodbridge Y, Amit S, Huppert A, Kopelman NM (2022) Viral load dynamics of SARS-CoV-2 delta and omicron variants following multiple vaccine doses and previous infection. Nat Commun 13:6706. https://doi.org/10.1038/s41467-022-33096-0
Abasiyanik MF, Flood B, Lin J, Ozcan S, Rouhani SJ, Pyzer A, Trujillo J, Zhen C, Wu P, Jumic S, Wang A, Gajewski TF, Wang P, Hartley M, Ameti B, Niemiec R, Fernando M, Aydogan B, Bethel C, Matushek S, Beavis KG, Agrawal N, Segal J, Tay S, Izumchenko E (2020) Sensitive detection and quantification of SARS-CoV-2 in saliva. medRxiv. https://doi.org/10.1101/2020.12.04.20241059
Abasiyanik MF, Flood B, Lin J, Ozcan S, Rouhani SJ, Pyzer A, Trujillo J, Zhen C, Wu P, Jumic S, Wang A, Gajewski TF, Wang P, Hartley M, Ameti B, Niemiec R, Fernando M, Mishra V, Savage P, Aydogan B, Bethel C, Matushek S, Beavis KG, Agrawal N, Segal J, Tay S, Izumchenko E (2021) Sensitive detection and quantification of SARS-CoV-2 in saliva. Sci Rep 11:12425. https://doi.org/10.1038/s41598-021-91835-7
Okoturo E, Amure M (2022) SARS-CoV-2 saliva testing using RT-PCR: a systematic review. Int J Infect Dis 121:166–171. https://doi.org/10.1016/j.ijid.2022.05.008
Carrouel F, Gadea E, Esparcieux A, Dimet J, Langlois ME, Perrier H, Dussart C, Bourgeois D (2021) Saliva quantification of SARS-CoV-2 in real-time PCR from asymptomatic or mild COVID-19 adults. Front Microbiol 12:786042. https://doi.org/10.3389/fmicb.2021.786042
Kornhaber MS, Florence T, Davis T, Kingsley K (2022) Assessment of oral human papillomavirus prevalence in pediatric and adult patients within a multi-ethnic clinic population. Dent J (Basel) 10. https://doi.org/10.3390/dj10040054
Menezes FDS, Latorre M, Conceicao GMS, Curado MP, Antunes JLF, Toporcov TN (2020) The emerging risk of oropharyngeal and oral cavity cancer in HPV-related subsites in young people in Brazil. PLoS One 15:e0232871. https://doi.org/10.1371/journal.pone.0232871
Nielsen KJ, Jakobsen KK, Jensen JS, Gronhoj C, Von Buchwald C (2021) The effect of prophylactic HPV vaccines on oral and oropharyngeal HPV infection-a systematic review. Viruses 13. https://doi.org/10.3390/v13071339
Smith DH, Raslan S, Samuels MA, Iglesias T, Buitron I, Deo S, Daunert S, Thomas GR, Califano J, Franzmann EJ (2021) Current salivary biomarkers for detection of human papilloma virus-induced oropharyngeal squamous cell carcinoma. Head Neck 43:3618–3630. https://doi.org/10.1002/hed.26830
Tsushima Y, Uno N, Sasaki D, Morinaga Y, Hasegawa H, Yanagihara K (2015) Quantitative RT-PCR evaluation of a rapid influenza antigen test for efficient diagnosis of influenza virus infection. J Virol Methods 212:76–79. https://doi.org/10.1016/j.jviromet.2014.10.019
Yamayoshi S, Sakai-Tagawa Y, Koga M, Akasaka O, Nakachi I, Koh H, Maeda K, Adachi E, Saito M, Nagai H, Ikeuchi K, Ogura T, Baba R, Fujita K, Fukui T, Ito F, Hattori SI, Yamamoto K, Nakamoto T, Furusawa Y, Yasuhara A, Ujie M, Yamada S, Ito M, Mitsuya H, Omagari N, Yotsuyanagi H, Iwatsuki-Horimoto K, Imai M, Kawaoka Y (2020) Comparison of rapid antigen tests for COVID-19. Viruses 12. https://doi.org/10.3390/v12121420
Yap T, Khor S, Kim JS, Kim J, Kim SY, Kern JS, Martyres R, Varigos G, Chan HT, McCullough MJ, Thomas ML, Scardamaglia L (2021) Intraoral human herpes viruses detectable by PCR in majority of patients. Oral Dis 27:378–387. https://doi.org/10.1111/odi.13523
To KKW, Yip CCY, Lai CYW, Wong CKH, Ho DTY, Pang PKP, Ng ACK, Leung KH, Poon RWS, Chan KH, Cheng VCC, Hung IFN, Yuen KY (2019) Saliva as a diagnostic specimen for testing respiratory virus by a point-of-care molecular assay: a diagnostic validity study. Clin Microbiol Infect 25:372–378. https://doi.org/10.1016/j.cmi.2018.06.009
Galar A, Catalan P, Vesperinas L, Miguens I, Munoz I, Garcia-Espona A, Sevillano JA, Andueza JA, Bouza E, Munoz P (2021) Use of saliva swab for detection of influenza virus in patients admitted to an emergency department. Microbiol Spectr 9:e0033621. https://doi.org/10.1128/Spectrum.00336-21
To KK, Lu L, Yip CC, Poon RW, Fung AM, Cheng A, Lui DH, Ho DT, Hung IF, Chan KH, Yuen KY (2017) Additional molecular testing of saliva specimens improves the detection of respiratory viruses. Emerg Microbes Infect 6:e49. https://doi.org/10.1038/emi.2017.35
Shen L, Niu J, Wang C, Huang B, Wang W, Zhu N, Deng Y, Wang H, Ye F, Cen S, Tan W (2019) High-throughput screening and identification of potent broad-spectrum inhibitors of coronaviruses. J Virol 93. https://doi.org/10.1128/JVI.00023-19
Meyers C, Robison R, Milici J, Alam S, Quillen D, Goldenberg D, Kass R (2021) Lowering the transmission and spread of human coronavirus. J Med Virol 93:1605–1612. https://doi.org/10.1002/jmv.26514
Bernstein D, Schiff G, Echler G, Prince A, Feller M, Briner W (1990) In vitro virucidal effectiveness of a 0.12%-chlorhexidine gluconate mouthrinse. J Dent Res 69:874–876. https://doi.org/10.1177/00220345900690030901
Mukherjee PK, Esper F, Buchheit K, Arters K, Adkins I, Ghannoum MA, Salata RA (2017) Randomized, double-blind, placebo-controlled clinical trial to assess the safety and effectiveness of a novel dual-action oral topical formulation against upper respiratory infections. BMC Infect Dis 17:74. https://doi.org/10.1186/s12879-016-2177-8
Sethuraman N, Jeremiah SS, Ryo A (2020) Interpreting diagnostic tests for SARS-CoV-2. JAMA 323:2249–2251. https://doi.org/10.1001/jama.2020.8259
Funding
Special issue including the proceedings of the symposium “What has dentistry learned from the pandemic?” held on 15th of September 2022 at the Pan European Region of the International Association for Dental Research (PER-IADR) Oral Health Research Congress, in Marseille, France. This symposium and these proceedings were made possible by a grant from DENTAID SL (Cerdanyola, Spain). The corresponding author received personal honoraria from Dentaid Research Center.
Author information
Authors and Affiliations
Contributions
DH searched and reviewed the literature. He has written the entire manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable
Competing interests
Dieter Hoffmann received lecture and consultation honoraria from DENTAID SL (Cerdanyola, Spain).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoffmann, D. The role of the oral cavity in SARS-CoV-2- and other viral infections. Clin Oral Invest 27 (Suppl 1), 15–22 (2023). https://doi.org/10.1007/s00784-023-05078-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05078-z