Abstract
Objective
To determine the effect of medium-chain fatty acids (MCFA) on the severity of denture stomatitis (DS) and the counts of Candida spp. in older people (OP) wearing removable prostheses (RP).
Materials and methods
This randomized, controlled and triple-blind study included forty-three OP presenting DS. The control group was treated with 0.12% chlorhexidine (CHX) and the experimental group with MCFA, 2 × /day for 15 days. Intraoral examination and counts of Candida spp. were performed at 0, 7, and 15 days. The differences between both groups in the decrease of the severity of DS and the viability of Candida spp. were determined clinically and microbiologically, respectively.
Results
OP carriers of RP treated with MCFA presented remission of the clinical signs of DS, but the Candida spp. counts only decreased significantly in the CHX-treated group at 7 days of treatment (p < 0.05). Besides, MCFA was shown to reduce the clinical signs of DS after the first week of application, while CHX after the second week.
Conclusions
The MCFA is effective in reducing the clinical signs of DS associated with oral candidiasis in subjects with RP. Both treatments showed a significant decrease in severity, for MCFA after the first week and for CHX two weeks after starting the corresponding treatment.
Clinical relevance
The MCFA is an effective, harmless, and accessible treatment alternative against DS, since it manages to reduce the severity of the lesion in the milder cases of DS in the oral mucosa of OP carriers of RP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Denture stomatitis (DS) is a chronic inflammatory process of the mucosa adjacent to the RP. Its presence ranges from 20 to 67% of patients with RP [1]. In Chile, the prevalence in OP has been little studied. In 2018, a cross-sectional study determined a prevalence of 45.5% of DS in subjects with RP [2]. Other studies have described a prevalence of 67.5% of oral mucosal lesions and 37.1% of DS [3]. DS is generally asymptomatic and its diagnosis is fundamentally clinical. DS is classified according to severity: Type I: simple and localized inflammatory lesion; Type II: simple generalized inflammatory lesion; and Type III: chronic inflammatory lesion with granulomatous papillary hyperplasia [4].
The multifactorial etiology of DS identifies local and systemic predisposing factors [5]. Within the local factors, those of mechanical-traumatic origin are highlighted especially by the continuous use of RP, which produces micro traumatic lesions, decreases salivary flow and pH, and hinders the arrival of salivary antibodies and mechanical tongue sweeping, favoring the appearance of an acidic and anaerobic microenvironment that allows the proliferation of opportunistic bacteria and fungi. In relation to the hygienic-infectious factor, poor oral and prosthetic hygiene allows the rapid development and accumulation of biofilms on the prosthetic surface, producing adhesion of species of the genus Candida, Staphylococcus aureus, Streptococcus mutans, and Lactobacillus spp., increasing the risk of DS [6,7,8].
In a review of the literature on the treatment of oral candidiasis, 24 articles on the antifungal therapy for this condition were analyzed [9]. The pharmacological agents included in these studies were itraconazole, miconazole, ketoconazole, and nystatin, among others. But these antifungals should be used only for infections in debilitated or immunosuppressed subjects due to their high systemic toxicity [10]. In the case of infections of mild or moderate severity, mechanical elements are used for oral and prosthetic hygiene, with the prescription of special brushes depending on the case. In relation to the mouthwashes that are usually indicated, the first choice is the one with 0.12% Chlorhexidine (CHX). CHX is a cationic bisguanidine, used as a broad-spectrum antimicrobial because of its bacteriostatic and bactericidal power, depending on the concentration. Within this spectrum, is the antifungal topical effect, since it can inhibit the adhesion of Candida spp., both to mucous membranes and to inert surfaces, such as RP [11]. But its prolonged use causes adverse effects on oral tissues—teeth and mucous membranes—in addition to causing staining in the restorations present in the mouth [9].
In recent times, antibiotic resistance, adverse effects, and toxicity of medications and mouthwashes have promoted the study of natural products of plant origin, with few or no adverse reactions, but with high antimicrobial properties. Among these products are the oils that have a high concentration of medium-chain fatty acids, such as sesame, olive, and coconut oil. The latter, coconut oil in its virgin state (VCO), has a higher concentration of these fatty acids, giving it a greater antimicrobial capacity, especially in yeasts of the Candida genus [12,13,14].
Most of the plants that contain edible oils have long-chain fatty acids; VCO is an exception as it contains both short and medium chains, which is why it has been classified as a medium-chain triglyceride, with chains of 6 to 12 carbons. VCO contains caproic acid (C6), caprylic acid (C8), capric acid (C10), and lauric acid (LA; C12). The latter is present at fifty percent in its composition. The high proportion of LA gives it its antimicrobial property, including antifungal. Studies have focused on Candida albicans, the most prevalent species of the genus [15]. In an in vitro study, it was observed that capric acid and LA can inhibit the growth of C. albicans, even at low concentrations.
There is little evidence available comparing the antimicrobial effect between CHX and VCO, but there is enough of each of them separately [16]. A study was conducted in children with early childhood caries, where one of the agents involved in its severity was C. albicans. When using these and other antimicrobials, it was observed that CHX and VCO presented similar antifungal activity, comparable to that obtained with ketoconazole. Other studies have also determined a significant reduction in plaque index, gingival index, and S. mutans counts. Besides, CHX and VCO affected negatively S. mutans and C. albicans biofilms in vitro [17]. The antimicrobial effect—including the anti-Candida action—has also been showed by using various short and medium-chain fatty acids, concluding that the latter can cause disruption of their cell membranes, producing their lysis. At micromolar concentration, fatty acids have a direct effect on the enzymatic activity that occurs in the cell membrane. An autoxidation would then take place with the production of peroxides and radicals [18,19,20].
To date, there are no studies analyzing the effect of VCO or other medium-chain triglycerides in the treatment of DS, despite their antifungal effect, both clinically and in vitro [13, 14, 21]. In the present clinical trial, VCO was used as an antifungal agent for the treatment of DS associated with oral candidiasis in older people with removable prostheses. It is proposed as an alternative antifungal treatment, with no or low toxicity, no side effects, and low cost, which helps to recover the oral-dental health of older people [21, 22].
Materials and methods
Volunteers
This study lasted 6 months (from September 2021 to March 2022) with different recruitment periods. 621 elders (Chilean women and men), users and beneficiaries of oral health programs of one Municipality located very close to the Faculty of Dentistry of our University, were invited to participate. Many of them were unable to participate for reasons such as the complex health context due to the COVID-19 pandemic, which limited their mobilization; their employment, when their availability did not coincide with the days or schedules of the intraoral examination and sample taking; OP who moved out of the commune; OP who could not use their removable prosthesis because it had a fracture or functional defect, or caused discomfort, or the abutment teeth or the prosthesis were lost; and external factors such as illness, domestic accidents, and scheduled surgeries. Finally, forty-three volunteers formed the sample. The sample size was calculated using the calculator of the Ministry of Health, Chile. A 20% oversample was made, in case of possible losses of follow-up, and a power of 80% (http://www.supersalud.gob.cl/observatorio/671/w3-article-7652.html).
The inclusion criteria were older people (≥ 60 years), self-reliant, healthy or with chronic diseases controlled by a medical doctor, removable prosthesis users (metal or acrylic base), with presence of clinical signs of denture stomatitis type I or II and who agreed to participate in the study through an informed consent signed by them. The exclusion criteria were volunteers with allergy or intolerance to chlorhexidine or virgin coconut oil, use of antibiotics or antifungals two weeks before participating, with severe dependence or institutionalized, with cognitive damage, or not accepting to be included in the study. All of them were not considered in the study, and the information obtained was eliminated. The study design and protocol were approved by the ethics committee for research on human beings of the Faculty of Medicine, University of Chile (June 12, 2020), and the study was performed in accordance with the postulates of the Declaration of Helsinki and international ethical guidelines for biomedical research in humans CIOMS 2016.
Study design
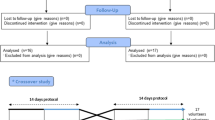
This study is a randomized, controlled, and triple-blind trial, using simple randomization, with a parallel design and an “intention-to-treat” modality of analysis. After the follow-up and sampling period, each participant was given an oral hygiene kit that included a toothbrush and a toothpaste.
The volunteers were randomly assigned to two groups: the control group (\(N=21\)) and the intervention group (\(N=22\)). The control group was treated with 0.12% CHX (commercially obtained) by rinsing with 15 mL for 5 min twice a day (morning and night) for two weeks. The intervention group was treated with the VCO (commercially obtained and certified by the manufacturer as 100% virgin) oil pulling technique, rinsing in the mouth a teaspoon with approx. 5 g for 5 min with the same frequency as the control group. Both groups were instructed to rinse without the prosthesis in the mouth, eliminate all the liquid without digesting it, and perform adequate prosthetic hygiene according to the examiner’s instructions. The field coordinator was responsible for the delivery of the vials of 0.12% CHX or VCO for the fourteen days of treatment. Each participant was assigned a numerical code to identify them, which was unknown to the examiners, the researchers who processed the saliva samples for microbiological analysis and those who analyzed the data (triple blind).
Intraoral clinical examination
Three similar intraoral examinations were carried out for each volunteer: at the beginning of the study (T0, prior to the treatment), one week after starting the treatment (T1) with either of the two rinses, and two weeks after starting the treatment (T2). Two dentists were calibrated as intra and interexaminer to determine prevalence and clinical severity of DS in the three times mentioned with a Kappa index of 0.72, according to the WHO criteria described by Espinoza et al. [23]. A previously designed and validated clinical record was used for this study as an instrument for data collection. The severity of DS was determined according to the classification of Newton [24] in type I and type II. The saliva sample was also taken at the three times mentioned (T0, T1, and T2). Gloves, KN95 respirator, bibs, disposable caps, face shield, examination instruments, and dental chairs located in primary health centers of the commune were used to perform the intraoral examination, respecting the biosecurity protocols for COVID-19 contingency.
Sampling, processing, and counts of Candida spp.
The volunteers attended the intraoral examination and the sampling while fasting, without smoking and without prior oral hygiene. After the clinical examination, they were asked to deposit 2 mL of unstimulated saliva in a sterile bottle. The samples were kept refrigerated at 4 °C until microbiological processing (less than 4 h). Saliva samples were homogenized and diluted to a 1:10 concentration in 0.9% NaCl. Subsequently, aliquots of 100 μL of diluted and undiluted saliva were seeded in duplicate in Sabouraud dextrose agar medium supplemented with chloramphenicol at a final concentration of 20 μg/mL. The plates were incubated at 37 °C for 48 h in an incubator (WTC model Binder) under aerobic conditions for the development of Candida spp. yeasts colonies. The counts of colonies compatible with the genus Candida (by macroscopic and microscopic visualization) were expressed in CFU/mL.
Data analysis
In the description of the data with categorical variables, frequencies and percentages were used. For data with quantitative variables, median and range were used, according to their distribution. The Shapiro Wilk test was used to analyze the type of data distribution, which resulted in a non-normal distribution. For the comparative analysis of the severity of DS in the three times of the study and for the colony count, the Wilcoxon test was used for paired data. Odds ratio was used to associate the decrease in severity with the microbiological count of yeast colonies. To evaluate the association between treatment and remission of DS severity, relative risk was used. Data were analyzed using STATA/SE 14.0 software. An alpha error equal to or less than 0.05 and a confidence interval of 95% were determined as statistical differences.
Results
Sample characterization
Among the forty-three volunteers included in the sample, the prevalence of DS was 54.4%; 93% were women (\(n=40\)) and 7% men (\(n=3\)). The average age of the total sample was 67 years.
DS was classified according to Newton, with 54% corresponding to type I and 46% to type II. It was also observed that the palate was the most frequent location of the oral lesion in 72% of the cases, followed by 19% in the alveolar ridge and 9% in both. In 10% of the cases, DS was associated with other oral mucosal lesions: angular cheilitis (5%), pseudomembranous candidiasis (2.5%), and traumatic ulcer (2.5%).
Of the sample, 65% had maxillary and mandibular removable prostheses, and 35% only maxillary prostheses. Ninety-five percent were acrylic and 5% metal-acrylic. Fifty-four percent of the sample mentioned daytime use of the appliances, 44% daytime and nighttime use, and 2% only used them in social contexts. Nineteen percent had been using their prosthesis for less than one year, 67% two to five years, and 14% more than five years. Twenty-three percent of the OP reported prosthetic maladjustment and discomfort in the use of the appliances due to the lack of retention, support, or stability.
Effects on the severity of DS in subjects treated with CHX or VCO
The forty-three subjects were randomly distributed into the two study groups. Ten patients did not complete their treatment, so they were not considered in the study and the information obtained was eliminated. The final sample was made up of 33 subjects, 32 women and 1 man. Fifteen participants conformed to the control group (treatment with CHX) and 18 to the intervention group (treatment with VCO). Tables 1 and 2 show the evolution of DS in the three times of the study in subjects treated with CHX or VCO.
The Wilcoxon statistical test was applied to both groups to compare the DS severity according to the three attention times. Between T0 and T1, there was no statistical difference in the control group (\(p=0.317\)), but there was one in the intervention group (\(p=0.045\)). Between T1 and T2, there was a statistical difference in both groups, with \(p=0.046\) in the control group and \(p=0.025\) in the intervention group. Finally, between T0 and T2, there was also a statistical difference in both groups, with a value of \(p=0.014\) in the control group and \(p=0.002\) in the intervention group.
Effects on the Candida spp. viability in subjects treated with CHX or VCO
Candida spp. counts were performed in CFU/mL from the saliva samples of the 33 subjects at each of the attention times in both groups, as shown in Table 3. When comparing both groups, according to the time of attention, no statistical difference was found at any time (\(p=0.502\), \(p=0.854\), and \(p=0.633\) at T0, T1, and T2, respectively). In addition, the Candida spp. counts of the saliva samples were compared in the three times, and a statistical difference was found only in the control group in T0 vs. T1 (Table 4).
Association between mouthwash use and DS remission
Relative risk was used in both groups to determine the association between the indicated treatment (CHX or VCO mouthwashes) and changes in the severity of DS, according to the attention times studied, showing a remission of the disease as a treatment benefit. The data showed a slight association, without statistical difference, between all times analyzed.
Association between DS severity and Candida spp. counts
Odds ratio was used to establish the association between DS severity and the Candida spp. counts in the attention times studied. In the control group, a minimal association without statistical difference was observed in the three times (OR 1.00004, \(p=0.475\)). On the other hand, in the intervention group, there was a minimal association only in time T2 (OR 1.00004, \(p=0.259\)).
Discussion
The present clinical study compared the effectiveness of medium-chain fatty acids (VCO) in the treatment of the severity of DS and its effect on the microbiological counts of Candida spp. in OP aged 60 years or more, carriers of RP, with the effectiveness of a treatment with 0.12% CHX.
Epidemiological data
The diagnosis of DS is eminently clinical and is frequently associated with the high presence of Candida yeasts. However, its etiology is of multifactorial origin, since traumatic, hygienic-infectious, and systemic conditions can have implications in its appearance. The prevalence of DS in this study was 54.4%, like the figures published by Ley-Sifontes et al. [25], who mention that the prevalence of this disease in Chile is 53% in patients with prostheses.
Kulak-Ozkan et al. [26] mentioned that daily hygiene allows removing food remains, as well as bacteria and fungi present, reducing the risk of DS. In the case of our participants, a large percentage mentioned using toothbrushing as a daily hygiene method, but only a low percentage used a complement such as dental floss, interproximal brushes, or mouthwashes. Considering strictly denture hygiene elements, more than half of the subjects mentioned using a denture brush. However, a non-negligible percentage used the same toothbrush to sanitize their dentures. Besides, almost half of the volunteers wore their prosthesis overnight.
Regarding the above, Gendreau et al. [7] mention that the use of dental prostheses overnight is associated with the development of DS. The lack of oral and denture hygiene habits, in addition to their constant use overnight, maintain relatively anaerobic and low pH conditions between the dentures and the mucosa, which can promote excessive growth of opportunistic pathogenic yeasts such as Candida spp., causing the appearance of DS. For this reason, it is important to consider these aspects when treating this disease. In the 43 subjects, DS was most frequently localized in the palate and maxillary alveolar ridge; these locations would be the most frequent as indicated by the definition given by Brevis et al. [27]. This study showed that, according to Newton’s classification, type I DS was the most prevalent in the group of hospitalized subjects, similar to the results obtained in the study by Gutierrez et al. [28], who observed DS in a population of OP carriers of RP.
Other diseases or lesions of the oral mucosa observed were angular cheilitis, pseudomembranous candidiasis, and traumatic ulcer. In the case of angular cheilitis, as reported by Martori et al. [29], this lesion is likely to be observed together with DS associated with Candida spp.
Regarding the material of the prostheses, almost all the volunteers (95%) wore acrylic prostheses, a material that, according to various authors, favors the adhesion of Candida spp., due to its porosity that constitutes a reservoir to cause this type of injury. With respect to the antiquity of the prosthesis, it was observed that more than half of the admitted cases had them for 2 to 5 years and even 12.5% of the cases had prostheses made more than 5 years ago. The above agrees with Gutiérrez et al. [28], who established that there is a higher prevalence of DS in older RP.
Regarding mechanical-traumatic factors of the same prosthesis, some volunteers mentioned suffering from these imbalances and prosthetic trauma due to misaligned prostheses, generating epithelial cell ruptures reducing the epithelial barrier and favoring the penetration of microbial antigens that constitute an important element for the appearance of DS. Hannah et al. [30] mentioned that approximately half of the users of poorly adjusted removable prostheses had DS type I, so attention must be paid to maximizing the support, retention, and stability of the prosthesis to prevent DS.
Experimental data
When the severity of DS was compared in the three times studied, a significant reduction was observed in both groups (control and intervention) between T0 and T2, so it was shown that both treatments are effective in reducing the severity of DS in two weeks of treatment. When comparing T0 and T1, there was only a significant reduction in the intervention group, indicating that VCO was more effective than CHX after one week of treatment.
In the control group, there was remission in 33% of the cases, presenting a similar decrease in both types of DS, with 13% and 20% in types I and II, respectively. Therefore, CHX treatment is effective in both types of DS. On the other hand, in the intervention group, the prevalence decreased in 50% of the cases, of which 38% were type I and 12% type II. This suggests that VCO treatment is more effective in mild cases of DS than in moderate cases.
Regarding the Candida spp. counts, the medians at T0 were 261.5 CFU/mL for the CHX group and 631 CFU/mL for the VCO group. Between T0 and T1, a decrease in the median was observed in both groups, but it was only significant in CHX. Then, at T2, the median of both groups increased. However, these data are not enough to demonstrate the effectiveness of the treatment on Candida spp. counts, since the median represents the central value of a very heterogeneous data set in a small sample. Therefore, when analyzing the data of the volunteers individually according to group and care time, the CHX group showed a significant decrease between T0 and T1, which suggests that this treatment has a greater antimicrobial effect during the first week with respect to VCO. However, between T0 and T2, no significant differences were observed in the counts of the samples of the volunteers 2 weeks after starting treatment, suggesting that none of the treatments was effective in reducing the amount of Candida yeasts.
The median counts obtained at T0 for both groups were similar to those obtained by Urzúa et al. [31], under similar conditions, but including the three types of DS according to Newton. The same study tested the effect of miconazole on Candida spp. counts in patients with DS and indicated that there was no statistically significant association between posttreatment yeast counts, systemic diseases, severity of DS, and intraoral conditions. In addition, it was observed that even though all patients remitted the clinical signs of DS after treatment, 56.2% had persistent high Candida yeasts counts.
Another observational study made by Taebunpakul and Jirawechwongsakul [32] determined the counts in the palatal mucosa of patients with DS, unlike this research that measured the salivary counts. They found no association between the Candida yeasts counts and the severity of DS. Although the counts of Candida spp. were greater in patients with DS than in healthy patients, this difference was not significant.
It should be noted that Candida spp. was present in 82% of the study participants, while 18% had a zero count; that is, they did not have these yeasts. The latter may be explained by the fact that the method used to determine the yeasts counts did not detect them. As mentioned by Farah et al. [33], C. albicans is a commensal microorganism of the oral cavity present in 45% to 65% of the healthy population. Thus, the presence of Candida spp. does not necessarily indicate prevalence of disease associated with these fungi. Also, there are patients with DS not associated with the presence of yeast of the genus Candida.
The odds ratio was used to determine if there was an association between Candida spp. counts and DS severity. It showed that there is a mathematical association (OR > 1) at T2 in both groups. However, this value is minimal, so for practical purposes it is not possible to establish whether there is an association. Furthermore, these values were not statistically significant, so the results cannot be extrapolated to the population, probably because the sample used was too small. However, another possible explanation lies in the potential synergistic effect of VCO to produce, in addition to a fungicidal effect, a local anti-inflammatory activity in the affected tissues, as has been documented. It has been described that the presence of medium-chain fatty acids, such as lauric acid and capric acid, some of the main components of VCO, has suppressive activity on gene expression of the proinflammatory cytokines IL-8 and TNF-α [34], which gives it, in addition to its antimicrobial capacity, a local anti-inflammatory effect. This could explain the marked drop in the severity of the clinical expression of DS at 7 days, despite presenting a fungicidal effectiveness relatively similar to CHX in the yeast counts of Candida spp. during the same period of time.
It is important to mention that not all the species of Candida involved in the etiology of DS were considered during the study. In other studies, apart from C. albicans detected in patients affected by this disease, other species were found, such as C. tropicalis, C. parapsilosis, C. glabrata, C. guilliermondii, and C. rugosa, which suggests that C. albicans is not the only species responsible for the appearance and development of this disease. Also, as mentioned by Baena et al. [35], it has been suggested that DS may be due to bacteria that are usually present in the oral cavity, such as Streptococcus spp. and Staphylococcus spp., or a combination of bacteria such as S. mutans and C. albicans.
As previously mentioned, the etiology of DS is multifactorial, so it is not only directly related to the presence and quantity of Candida spp., but also to the prosthetic quality [36], which includes factors that were not analyzed here, such as prosthetic stability, prosthetic hygiene, night use of appliances, prosthetic design, occlusal stability, and masticatory force.
According to the data obtained, the oil pulling technique with medium-chain fatty acids (VCO) is an effective alternative treatment against DS associated or not with oral candidiasis, since it manages to reduce the severity of the oral mucosa lesion in OP with RP. However, this treatment does not reduce the Candida yeasts counts in these subjects.
Limitations
-
Sample size: for this work, we had an initial population of 621 OP invited to participate in the study. However, this number could not be maintained due to multiple complications associated with the context in which this research was carried out, that is, the COVID-19 pandemic. This fact limited the elaboration of associations and significances from the data since more individuals (more than 33) were needed to ensure a representative distribution to be extrapolated to the population.
-
Lack of previous research on the subject: to date, there is no available literature of clinical studies on the oil pulling technique and the use of VCO for the treatment of DS. However, the justification for carrying out this work is based on references of in vitro studies on the effect of VCO and its medium-chain triglycerides against C. albicans and the formation of bacterial plaque.
Conclusions
The evidence of this research work shows that the oil pulling technique with medium-chain fatty acids (VCO) is effective in reducing the clinical signs of DS associated with oral candidiasis in subjects with RP, in less time than CHX, which is only effective after the second week of use.
However, neither the oil pulling technique with medium-chain fatty acids (VCO) nor the use of CHX were effective in reducing the counts of Candida spp. after the treatments were finished. Furthermore, this study showed that the Candida yeasts counts alone are not sufficient to be associated with the presence and severity of DS.
References
Gual-Vaqués P, Jané-Salas E, Egido-Moreno S, Ayuso-Montero R, Marí-Roig A, López-López J (2017) Inflammatory papillary hyperplasia: a systematic review. Med Oral Patol Oral Cir Bucal 22:e36–e42. https://doi.org/10.4317/medoral.21405
Lozano C, Vergara C, Lee X (2018) Prevalence of oral lesions and chronic non –communicable diseases in a simple of Chilean institutionalized versus non-institutionalized elderly. J Oral Res 7:108–113. https://doi.org/10.17126/joralres.2018.025
Cueto A, Martínez R, Niklander S (2013) Prevalence of oral mucosal lesions in an elderly population in the city of Valparaiso, Chile. Gerodontol 30:201–206. https://doi.org/10.1111/j.1741-2358.2012.00663.x
Koeck B (2007) Prótesis completas. 4a edn. Urban & Fischer, pp 344–346
Emami E, Taraf H, de Grandmont P (2012) The association of denture stomatitis and partial removable dental prostheses: a systematic review. Int J Prosthodont 25:113–119
Shimizu C, Kuriyama T, Williams D (2008) Association of oral yeast carriage with specific host factors and altered mouth sensation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:445–451. https://doi.org/10.1016/j.tripleo.2007.11.030
Gendreau L, Loewy Z (2011) Epidemiology, and etiology of denture stomatitis. J Prosthodont 20:251–260. https://doi.org/10.1111/j.1532-849X.2011.00698.x
Hoshi N, Mori H, Taguchi H (2011) Management of oral candidiasis in denture wearers. J Prosthodont Res 55:48–52. https://doi.org/10.1016/j.jpor.2010.03.004
Hilgert JB, Giordani JM, de Souza RF, Wendland EM, D’Avila OP, Hugo FN (2016) Interventions for the management of denture stomatitis: a systematic review and meta-analysis. J Am Geriatr Soc 64:2539–2545. https://doi.org/10.1111/jgs.14399
Fang J, Huang B, Ding Z (2021) Efficacy of antifungal drugs in the treatment of oral candidiasis: a Bayesian network meta-analysis. J Prosthet Dent 125:257–265. https://doi.org/10.1016/j.prosdent.2019.12.025
Williams D, Lewis M (2011) Pathogenesis and treatment of oral candidosis. J Oral Microbiol 3:1–11. https://doi.org/10.3402/jom.v3i0.5771
Arjunkumar R, Balagopal S (2013) Chlorhexidine: the gold standard antiplaque agent. J Pharmac Sci Res 5:270–274
Abbas A, Assikong E, Akeh M, Upla P, Tuluma T (2017) Antimicrobial activity of coconut oil and its derivate (Lauric acid) on some selected clinical isolates. Int J Med Sci Clin Invent 4:3173–3177. https://doi.org/10.18535/ijmsci/v4i8.12
Nur A, Zurainie A, Anil A, Intan A, Wan N (2018) Virgin coconut oil and its antimicrobial properties against pathogenic microorganisms: a review. Adv Health Sci Res 8:192–199. https://doi.org/10.2991/idcsu-17.2018.51
Gbinigie O, Onakpoya I, Spencer E, McCall M, Heneghan C (2016) Effect of oil pulling in promoting oro dental hygiene: a systematic review of randomized clinical trials. Complement Ther Med 26:47–54. https://doi.org/10.1016/j.ctim.2016.02.011
Beena S, Faizal P, Shyamala J, Gufran B, Soni K, Deepak J (2016) Comparison of antimicrobial activity of chlorhexidine, coconut oil, probiotics, and ketoconazole on Candida albicans isolated in children with early childhood caries: an in vitro study. Scientifica 216:7061587. https://doi.org/10.1155/2016/7061587
Siripaiboonpong N, Matangkasombut O, Pengcharoen H, Boonchaiyapluk B, Rujiraprasert P, Suphanantachat S (2022) Microbiological effects of virgin coconut oil pulling in comparison with palm oil pulling as an adjunctive oral hygiene care for patients with gingival inflammation: a randomized controlled clinical trial. J Indian Soc Periodontol 26:58–63. https://doi.org/10.4103/jisp.jisp_768_20
Salian V, Shetty P (2018) Coconut oil and virgin coconut oil. An insight into its oral and overall health benefits. J Clin Diag Res 12:ZE01–ZE03. https://doi.org/10.7860/JCDR/2018/31409.11051
Satheesh N (2015) Review on production and potential applications of virgin coconut oil. Annals Food Sci and Tech 16:116–126
Huang C, Alimova Y, Myers T, Ebersole J (2011) Short-and medium-chain fatty acids exhibit antimicrobial activity for oral microorganisms. Arch Oral Biol 56:650–654. https://doi.org/10.1016/j.archoralbio.2011.01.011
Woolley J, Gibbons T, Patel K, Sacco R (2020) The effect of oil pulling with coconut oil to improve dental hygiene and oral health: a systematic review. Heliyon 6:e04789. https://doi.org/10.1016/j.heliyon.2020.e04789
Anagnostou K (2017) Coconut allergy revisited. Children 4:85. https://doi.org/10.3390/children4100085
Espinoza I, Rojas R, Aranda W, Gamonal J (2003) Prevalence of oral mucosal lesions in elderly people in Santiago, Chile. J Oral Pathol Med 32:571–575. https://doi.org/10.1034/j.1600-0714.2003.00031.x
Newton AV (1962) Denture sore mouth. A possible etiology. British Dent J 112:357–360
Ley-Sifontes L, Silva Y, Martín Reyes O, Paz E, Landrián C (2008) Eficacia del aceite de girasol ozonizado en el tratamiento de la estomatitis subprótesis grado I y II. AMC 12:1–10
Kulak-Ozkan Y, Kazazoglu E, Arikan A (2002) Oral hygiene habits, denture cleanliness, presence of yeasts and stomatitis in elderly people. J Oral Rehabil 29:300–304. https://doi.org/10.1046/j.1365-2842.2002.00816.x
Brevis A, Cancino M, Cantín L (2008) Estomatitis subprótesis: estudio clínico y microbiológico de Candida. Int J Odontostomat 2:101–108
Gutiérrez C, Bustos L, Sánchez M, Zaror L, Zambrano M (2013) Denture stomatitis in patients of the IX region, Chile. Int J Odontostomat 7:207–213
Martori E, Ayuso-Montero R, Martinez-Gomis J, Viñas M, Peraire M (2014) Risk factors for denture-related oral mucosal lesions in a geriatric population. J Prosthet Dent 111:273–279. https://doi.org/10.1016/j.prosdent.2013.07.015
Hannah VE, O’Donnell L, Robertson D, Ramage G (2017) Denture stomatitis: causes, cures and prevention. Prim Dent J 6:46–51. https://doi.org/10.1308/205016817822230175
Urzúa-Orellana B, Palma-Fluxá P, Salinas-Flores J, Lee-Muñoz X, Cortés-Coloma A, Vergara-Núñez C (2018) Efecto de miconazol sobre el recuento de levaduras en candidiasis asociada a estomatitis protésica. Rev Clin Periodoncia Implantol Rehabil Oral 11:102–105. https://doi.org/10.4067/S0719-01072018000200202
Taebunpakul P, Jirawechwongsakul P (2021) Palatal inflammation and the presence of Candida in denture-wearing patients. J Int Soc Prev Community Dent 11:272–280. https://doi.org/10.4103/jispcd.JISPCD_368_20
Farah CS, Lynch N, McCullough MJ (2010) Oral fungal infections: an update for the general practitioner. Aust Dent J 55(Suppl 1):48–54. https://doi.org/10.1111/j.1834-7819.2010.01198.x
Huang WC, Tsai TH, Chuang LT, Li YY, Zouboulis CC, Tsai PJ (2014) Anti-bacterial and anti-inflammatory properties of capric acid against Propionibacterium acnes: a comparative study with lauric acid. J Dermatol Sci 73:232–240. https://doi.org/10.1016/j.jdermsci.2013.10.010
Baena-Monroy T, Moreno-Maldonado V, Franco-Martínez F, Aldape-Barrios B, Quindós G, Sánchez-Vargas LO (2005) Candida albicans, Staphylococcus aureus and Streptococcus mutans colonization in patients wearing dental prosthesis. Med Oral Patol Oral Cir Bucal 10(Suppl 1):27–39
Lee X, Cajas N, Gómez L, Vergara C, Ivankovic M, Astorga E (2015) Ocurrencia de levaduras del género Candida y estomatitis protésica antes y después del tratamiento rehabilitador basado en prótesis removible. Rev Clin Periodoncia Implantol Rehabil Oral 8:31–37. https://doi.org/10.1016/j.piro.2015.02.005
Funding
This investigation was funded by grant FONIS SA19I0025 from the Chilean National Research and Development Agency (ANID), the Chilean Government. Thanks to Mr. Juan Fernández, from the language and Translation Services of the Faculty of Dentistry, University of Chile, for kindly proofreading and checking the spelling and grammar of this manuscript.
Author information
Authors and Affiliations
Contributions
X.L.M. and C.P.L. conceived the idea and designed the experiments. J.J.F. was the field coordinator. C.V.N. processed and analyzed the data. X.L.M., C.V.N. and C.P.L. drafted the first manuscript. C.P.L. wrote the final manuscript. All authors revised and approved the final version of the article.
Corresponding author
Ethics declarations
Ethics approval
The study design and protocol were approved by the ethics committee for research on human beings of the Faculty of Medicine, University of Chile (June 12, 2020), and the study was performed in accordance with the postulates of the Declaration of Helsinki and international ethical guidelines for biomedical research in humans CIOMS 2016.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee Muñoz, X., Vergara Núñez, C., Jerez Fuentes, J. et al. Medium-chain fatty acids as an alternative treatment for denture stomatitis in older people. Clin Oral Invest 27, 3713–3720 (2023). https://doi.org/10.1007/s00784-023-04987-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04987-3