Abstract
Objectives
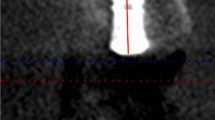
This study aimed to analyze the effect of the apex coverage by the bone graft, including exposure and coverage less than or greater than 2 mm on implant survival rate and peri-implant bone and soft tissue remodeling.
Materials and methods
A total of 264 implants in 180 patients who had undergone transcrestal sinus floor elevation (TSFE) with simultaneous implant placement were included in this retrospective cohort study. Radiographic assessment was used to categorize the implants into three groups based on apical implant bone height (ABH): ≤ 0 mm, < 2 mm, or ≥ 2 mm. The implant survival rate, peri-implant marginal bone loss (MBL) during short-term (1–3 years) and mid- to long-term (4–7 years) follow-up, and clinical parameters were used to evaluate the effect of implant apex coverage after TSFE.
Results
Group 1 had 56 implants (ABH ≤ 0 mm), group 2 had 123 implants (ABH > 0 mm, but < 2 mm), and group 3 had 85 implants (ABH ≥ 2 mm). There was no significant difference in the implant survival rate between groups 2 and 3 compared to group 1 (p = 0.646, p = 0.824, respectively). The MBL during short-term and mid- to long-term follow-up indicated that apex coverage could not be considered a risk factor. Furthermore, apex coverage did not have a significant effect on other clinical parameters.
Conclusions
Despite limitations, our study found that implant apex coverage by the bone graft, including exposure and coverage levels less than or greater than 2 mm, did not significantly affect implant survival, short-term or mid- to long-term MBL, or peri-implant soft tissue outcomes.
Clinical relevance
Based on 1- to 7-year data, the study suggests that implant apical exposure and coverage levels of less than or greater than 2 mm bone graft are both valid options for TSFE cases.



Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Starch-Jensen T, Mordenfeld A, Becktor JP, Jensen SS (2018) Maxillary sinus floor augmentation with synthetic bone substitutes compared with other grafting materials: a systematic review and meta-analysis. Implant Dent 27:363–374. https://doi.org/10.1097/id.0000000000000768
Farina R, Franceschetti G, Travaglini D, Consolo U, Minenna L, Schincaglia GP, Riccardi O, Bandieri A, Maietti E, Trombelli L (2018) Morbidity following transcrestal and lateral sinus floor elevation: a randomized trial. J Clin Periodontol 45:1128–1139. https://doi.org/10.1111/jcpe.12985
Lozada JL, Goodacre C, Al-Ardah AJ, Garbacea A (2011) Lateral and crestal bone planing antrostomy: a simplified surgical procedure to reduce the incidence of membrane perforation during maxillary sinus augmentation procedures. J Prosthet Dent 105:147–153. https://doi.org/10.1016/s0022-3913(11)60020-6
Lang NP, Berglundh T, Giannobile WV and Sanz M (2021) Clinical Periodontology and Implant Dentistry, 2 Volume Set, 7th Edition. John Wiley and Sons, Inc, Chichester, West Sussex; Ames, Iowa.
Shi QH, Luo Y, Cheng YT, Huo H, Wu C, Liao J (2022) The prognostic outcome of transalveolar sinus floor elevation with or without grafting materials: a meta-analysis. Int J Oral Maxillofac Implants 37:869–878. https://doi.org/10.11607/jomi.9758
Pjetursson BE, Ignjatovic D, Matuliene G, Brägger U, Schmidlin K, Lang NP (2009) Transalveolar maxillary sinus floor elevation using osteotomes with or without grafting material. Part II: Radiographic tissue remodeling. Clin Oral Implants Res 20:677–683. https://doi.org/10.1111/j.1600-0501.2009.01721.x
Paik JW, Cha JK, Song YW, Thoma DS, Jung RE, Jung UW (2022) Effect of Schneiderian membrane integrity on bone formation in sinus augmentation: an experimental study in rabbits. J Clin Periodontol 49:76–83. https://doi.org/10.1111/jcpe.13562
Tan WC, Lang NP, Zwahlen M, Pjetursson BE (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. Part II: Transalveolar technique. J Clin Periodontol 35:241–254. https://doi.org/10.1111/j.1600-051X.2008.01273.x
Huang J, Ban C, Liu L, Ye Y (2021) Dynamics and risk indicators of intrasinus elevation height following transalveolar sinus floor elevation with immediate implant placement: a longitudinal cohort study. Int J Oral Maxillofac Surg 50:109–115. https://doi.org/10.1016/j.ijom.2020.04.020
Franceschetti G, Farina R, Minenna L, Riccardi O, Stacchi C, Di Raimondo R, Maietti E, Trombelli L (2020) The impact of graft remodeling on peri-implant bone support at implants placed concomitantly with transcrestal sinus floor elevation: a multicenter, retrospective case series. Clin Oral Implants Res 31:105–120. https://doi.org/10.1111/clr.13541
Ueno D, Banba N, Hasuike A, Ueda K, Kodama T (2019) A sinus floor reaugmentation technique around an apically exposed implant into the maxillary sinus. J Oral Implantol 45:213–217. https://doi.org/10.1563/aaid-joi-D-18-00271
Brägger U, Gerber C, Joss A, Haenni S, Meier A, Hashorva E, Lang NP (2004) Patterns of tissue remodeling after placement of ITI dental implants using an osteotome technique: a longitudinal radiographic case cohort study. Clin Oral Implants Res 15:158–166. https://doi.org/10.1111/j.1600-0501.2004.00988.x
Levin L, Herzberg R, Dolev E, Schwartz-Arad D (2004) Smoking and complications of onlay bone grafts and sinus lift operations. Int J Oral Maxillofac Implants 19:369–373
Park WB, Park W, Han JY, Kang P (2022) Successful management of apically exposed implants in the maxillary sinus and associated sinus pathologies. J Oral Implantol. https://doi.org/10.1563/aaid-joi-D-21-00081
Tabrizi R, Amid R, Taha Özkan B, Khorshidi H, Langner NJ (2012) Effects of exposing dental implant to the maxillary sinus cavity. J Craniofac Surg 23:767–769. https://doi.org/10.1097/SCS.0b013e31824dbd19
Nedir R, Nurdin N, Abi Najm S, El Hage M, Bischof M (2017) Short implants placed with or without grafting into atrophic sinuses: the 5-year results of a prospective randomized controlled study. Clin Oral Implants Res 28:877–886. https://doi.org/10.1111/clr.12893
O’Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43:38. https://doi.org/10.1902/jop.1972.43.1.38
Vagia P, Papalou I, Burgy A, Tenenbaum H, Huck O, Davideau JL (2021) Association between periodontitis treatment outcomes and peri-implantitis: a long-term retrospective cohort study. Clin Oral Implants Res 32:721–731. https://doi.org/10.1111/clr.13741
Schmidlin K, Schnell N, Steiner S, Salvi GE, Pjetursson B, Matuliene G, Zwahlen M, Brägger U, Lang NP (2010) Complication and failure rates in patients treated for chronic periodontitis and restored with single crowns on teeth and/or implants. Clin Oral Implants Res 21:550–557. https://doi.org/10.1111/j.1600-0501.2009.01907.x
Harlos MM, da Silva TB, Montagner PG, Teixeira LN, Gomes AV, Martinez EF (2022) Histomorphometric evaluation of different graft associations for maxillary sinus elevation in wide antral cavities: a randomized controlled clinical trial. Clin Oral Investig 26:1–9. https://doi.org/10.1007/s00784-022-04515-9
Khaled H, Atef M, Hakam M (2019) Maxillary sinus floor elevation using hydroxyapatite nano particles vs tenting technique with simultaneous implant placement: a randomized clinical trial. Clin Implant Dent Relat Res 21:1241–1252. https://doi.org/10.1111/cid.12859
Pjetursson BE (2000) Lang NP (2014) Sinus floor elevation utilizing the transalveolar approach. Periodontol 66:59–71. https://doi.org/10.1111/prd.12043
Beck-Broichsitter BE, Gerle M, Wiltfang J, Becker ST (2020) Perforation of the Schneiderian membrane during sinus floor elevation: a risk factor for long-term success of dental implants? Oral Maxillofac Surg 24:151–156. https://doi.org/10.1007/s10006-020-00829-8
Tavelli L, Borgonovo AE, Saleh MH, Ravidà A, Chan HL, Wang HL (2020) Classification of sinus membrane perforations occurring during transcrestal sinus floor elevation and related treatment. Int J Periodontics Restorative Dent 40:111–118. https://doi.org/10.11607/prd.3602
Stumbras A, Krukis MM, Januzis G, Juodzbalys G (2019) Regenerative bone potential after sinus floor elevation using various bone graft materials: a systematic review. Quintessence Int 50:548–558. https://doi.org/10.3290/j.qi.a42482
Arosio P, Greco GB, Zaniol T, Iezzi G, Perrotti V, Di Stefano DA (2018) Sinus augmentation and concomitant implant placement in low bone-density sites. A retrospective study on an undersized drilling protocol and primary stability. Clin Implant Dent Relat Res 20:151–159. https://doi.org/10.1111/cid.12558
Liu Y, Chen Y, Chu C, Qu Y, Xiang L, Man Y (2020) A prospective cohort study of immediate implant placement into posterior compromised sockets with or without primary wound closure of reactive soft tissue. Clin Implant Dent Relat Res 22:13–20. https://doi.org/10.1111/cid.12845
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E, Hämmerle CHF, Heitz-Mayfield LJA, Huynh-Ba G, Iacono V, Koo KT, Lambert F, McCauley L, Quirynen M, Renvert S, Salvi GE, Schwarz F, Tarnow D, Tomasi C, Wang HL, Zitzmann N (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 45(Suppl. 20):S286–S291. https://doi.org/10.1111/jcpe.12957
Mendoza-Azpur G, Lau M, Valdivia E, Rojas J, Muñoz H, Nevins M (2016) Assessment of marginal peri-implant bone-level short-length implants compared with standard implants supporting single crowns in a controlled clinical trial: 12-month follow-up. Int J Periodontics Restorative Dent 36:791–795. https://doi.org/10.11607/prd.3026
Jung RE, Al-Nawas B, Araujo M, Avila-Ortiz G, Barter S, Brodala N, Chappuis V, Chen B, De Souza A, Almeida RF, Fickl S, Finelle G, Ganeles J, Gholami H, Hammerle C, Jensen S, Jokstad A, Katsuyama H, Kleinheinz J, Kunavisarut C, Mardas N, Monje A, Papaspyridakos P, Payer M, Schiegnitz E, Smeets R, Stefanini M, Ten Bruggenkate C, Vazouras K, Weber HP, Weingart D, Windisch P (2018) Group 1 ITI consensus report: the influence of implant length and design and medications on clinical and patient-reported outcomes. Clin Oral Implants Res 29(Suppl 16):69–77. https://doi.org/10.1111/clr.13342
Yu Y, Jiang Q, Zhang Z, Yu X, Deng F (2021) Influence of implant protrusion length on non-grafting osteotome sinus floor elevation with simultaneous implant: a 3- to 9-year retrospective study. Int J Implant Dent 7:22. https://doi.org/10.1186/s40729-021-00304-3
Comuzzi L, Tumedei M, Piattelli A, Tartaglia G, Del Fabbro M (2022) Radiographic analysis of graft dimensional changes in transcrestal maxillary sinus augmentation: a retrospective study. Materials 15:2964. https://doi.org/10.3390/ma15092964
Cehreli MC, Akkocaoglu M, Comert A, Tekdemir I, Akca K (2007) Bone strains around apically free versus grafted implants in the posterior maxilla of human cadavers. Med Biol Eng Comput 45:395–402. https://doi.org/10.1007/s11517-007-0173-2
Desai SR, Singh R, Karthikeyan I (2013) 2D FEA of evaluation of micromovements and stresses at bone-implant interface in immediately loaded tapered implants in the posterior maxilla. J Indian Soc Periodontol 17:637–643. https://doi.org/10.4103/0972-124x.119283
Chen Y, Yuan S, Zhou N, Man Y (2017) Transcrestal sinus floor augmentation with immediate implant placement applied in three types of fresh extraction sockets: a clinical prospective study with 1-year follow-up. Clin Implant Dent Relat Res 19:1034–1043. https://doi.org/10.1111/cid.12529
Kolhatkar S, Bhola M, Thompson-Sloan TN (2011) Sinus floor elevation via the maxillary premolar extraction socket with immediate implant placement: a case series. J Periodontol 82:820–828. https://doi.org/10.1902/jop.2010.100557
Ekhlasmandkermani M, Amid R, Kadkhodazadeh M, Hajizadeh F, Abed PF, Kheiri L, Kheiri A (2021) Sinus floor elevation and simultaneous implant placement in fresh extraction sockets: a systematic review of clinical data. J Korean Assoc Oral Maxillofac Surg 47:411–426. https://doi.org/10.5125/jkaoms.2021.47.6.411
Marconcini S, Giammarinaro E, Derchi G, Alfonsi F, Covani U, Barone A (2018) Clinical outcomes of implants placed in ridge-preserved versus nonpreserved sites: a 4-year randomized clinical trial. Clin Implant Dent Relat Res 20:906–914. https://doi.org/10.1111/cid.12682
Apostolopoulos P, Darby I (2017) Retrospective success and survival rates of dental implants placed after a ridge preservation procedure. Clin Oral Implants Res 28:461–468. https://doi.org/10.1111/clr.12820
Park SH, Song YW, Sanz-Martín I, Cha JK, Lee JS, Jung UW (2020) Clinical benefits of ridge preservation for implant placement compared to natural healing in maxillary teeth: a retrospective study. J Clin Periodontol 47:382–391. https://doi.org/10.1111/jcpe.13231
Pozzi A, Agliardi E, Tallarico M, Barlattani A (2014) Clinical and radiological outcomes of two implants with different prosthetic interfaces and neck configurations: randomized, controlled, split-mouth clinical trial. Clin Implant Dent Relat Res 16:96–106. https://doi.org/10.1111/j.1708-8208.2012.00465.x
Yamanishi Y, Yamaguchi S, Imazato S, Nakano T, Yatani H (2012) Influences of implant neck design and implant-abutment joint type on peri-implant bone stress and abutment micromovement: three-dimensional finite element analysis. Dental Materials 28:1126-1133.https://doi.org/10.1016/j.dental.2012.07.160
Koller CD, Pereira-Cenci T, Boscato N (2016) Parameters associated with marginal bone loss around implant after prosthetic loading. Braz Dent J 27:292–297. https://doi.org/10.1590/0103-6440201600874
Alhammadi SH, Burnside G, Milosevic A (2021) Clinical outcomes of single implant supported crowns versus 3-unit implant-supported fixed dental prostheses in Dubai Health Authority: a retrospective study. BMC Oral Health 21:171. https://doi.org/10.1186/s12903-021-01530-2
Castellanos-Cosano L, Carrasco-García A, Corcuera-Flores JR, Silvestre-Rangil J, Torres-Lagares D, Machuca-Portillo G (2021) An evaluation of peri-implant marginal bone loss according to implant type, surgical technique and prosthetic rehabilitation: a retrospective multicentre and cross-sectional cohort study. Odontology 109:649–660. https://doi.org/10.1007/s10266-020-00587-9
Kohal RJ, Spies BC, Vach K, Balmer M, Pieralli S (2020) A prospective clinical cohort investigation on zirconia implants: 5-year results. J Clin Med 9. https://doi.org/10.3390/jcm9082585
Liang F, Wu MJ, Zou LD (2021) Clinical observation of the curative effect after 5-year follow-up of single tooth implant-supported restorations in the posterior region. Beijing Da Xue Xue Bao Yi Xue Ban 53:970–976. https://doi.org/10.19723/j.issn.1671-167X.2021.05.027
Mumcu E, Beklen A (2019) The effect of smoking on the marginal bone loss around implant-supported prostheses. Tob Induc Dis 17:43. https://doi.org/10.18332/tid/109279
Chen CJ, Papaspyridakos P, Guze K, Singh M, Weber HP, Gallucci GO (2013) Effect of misfit of cement-retained implant single crowns on crestal bone changes. Int J Prosthodont 26:135–137. https://doi.org/10.11607/ijp.3137
Katsoulis J, Takeichi T, Sol Gaviria A, Peter L, Katsoulis K (2017) Misfit of implant prostheses and its impact on clinical outcomes Definition, assessment and a systematic review of the literature. Eur J Oral Implantol 10(Suppl 1):121–138
Saaby M, Karring E, Schou S, Isidor F (2016) Factors influencing severity of peri-implantitis. Clin Oral Implants Res 27:7–12. https://doi.org/10.1111/clr.12505
de Araújo NM, Mano Azul A, Rocha E, Maló P (2015) Risk factors of peri-implant pathology. Eur J Oral Sci 123:131–139. https://doi.org/10.1111/eos.12185
Hatta K, Takahashi T, Sato H, Murakami S, Maeda Y, Ikebe K (2021) Will implants with a fixed dental prosthesis in the molar region enhance the longevity of teeth adjacent to distal free-end edentulous spaces? Clin Oral Implants Res 32:242–248. https://doi.org/10.1111/clr.13695
Ataol M, Kilinc A, Saruhan N, Gundogdu M (2019) Finite element analysis of two different implant applicable for vertical bone deficiency at maxillary sinus. J Biomater Tissue Eng 9:315–321. https://doi.org/10.1166/jbt.2019.1978
Ibañez C, Catena A, Galindo-Moreno P, Noguerol B, Magán-Fernández A, Mesa F (2016) Relationship between long-term marginal bone loss and bone quality, implant width, and surface. Int J Oral Maxillofac Implants 31:398–405. https://doi.org/10.11607/jomi.4245
Naseri R, Yaghini J, Feizi A (2020) Levels of smoking and dental implants failure: a systematic review and meta-analysis. J Clin Periodontol 47:518–528. https://doi.org/10.1111/jcpe.13257
Hasegawa M, Hotta Y, Hoshino T, Ito K, Komatsu S, Saito T (2016) Long-term radiographic evaluation of risk factors related to implant treatment: suggestion for alternative statistical analysis of marginal bone loss. Clin Oral Implants Res 27:1283–1289. https://doi.org/10.1111/clr.12734
Park WB, Kang KL, Han JY (2019) Factors influencing long-term survival rates of implants placed simultaneously with lateral maxillary sinus floor augmentation: a 6- to 20-year retrospective study. Clin Oral Implants Res 30:977–988. https://doi.org/10.1111/clr.13505
Funding
This work was financially supported by the National Natural Science Foundation of China (No. 81870801) and the Sichuan Science and Technology Program grant (No. 2022YFS0041).
Author information
Authors and Affiliations
Contributions
Yili Qu and Yi Man conceived the ideas. Jiayu Gao and Xiangqi Zhao collected the data. Jiayu Gao, Xiangqi Zhao, and Yili Qu analyzed the data and conducted the writing. All authors gave final approval and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This retrospective study involving human participants was performed in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval was granted by the Ethics Committee of Sichuan University (ethics registration number: WCHSIRB-CT-2021–504). Informed consent was obtained from all individual participants included in the study. Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiayu Gao and Xiangqi Zhao are joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, J., Zhao, X., Man, Y. et al. Effect of the implant apical exposure and coverage < or ≥ 2 mm bone graft on transcrestal sinus floor elevation: a 1- to 7-year retrospective cohort study. Clin Oral Invest 27, 3611–3626 (2023). https://doi.org/10.1007/s00784-023-04974-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04974-8