Abstract
Objectives
Professionals in the health sector have higher stress than others. The aim of this study was to evaluate the stress levels of dentists while treating with children under clinical, deep sedation, and general anesthesia.
Materials and methods
Blood pressure (systolic, diastolic), pulse value, and O2 saturations were measured. Saliva samples were taken by the dentists 10 min before the treatment, at the 25th min of the treatment, and 30 min after the treatment under clinical, deep sedation, and general anesthesia. Salivary cortisol was measured by the electrochemiluminescence method. All data were analyzed statistically.
Results
Cortisol values under the sedation were higher than clinical and general anesthesia (P < 0.05). As a result of the applied Dentist Job Stress Questionnaire, the stress level of dentists under sedation was higher than the clinical and general anesthesia (P < 0.05). Under sedation, systolic and diastolic blood pressures measured during the procedure were found to be high (P < 0.05).
Conclusions
Dentists who care for pediatric patients are more stressed when applying treatment under deep sedation. The results suggest the need for more training and practice to strengthen the education given on general anesthesia/sedation in pediatric dentistry training.
Clinical revelance
To increase the health and treatment quality of the dentists, who spend most of the day with the dental treatment of children, should be taken precautions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress is commonly defined as occurring when an individual’s high expectations force their capacity to adapt [1]. Occupational stress, defined as when the resources of an individual are not sufficient to cope with the needs of a situation, is a leading modern health and safety challenge [2].
Health sector professionals have higher stress than other professionals, and it is usually caused by workload and patient‒doctor relationships [3,4,5,6]. Dentistry professions constantly require a high level of skill and attention. Especially in pediatric dentistry, behavior management problems in children, parental expectations, and parental behaviors can be more stressful and exhausting in practice [7,8,9,10]. General dental practitioners report that they are very stressed due to anxious children and their behaviors that prevent clinical procedures [11, 12]. Additionally, parents’ inability to understand the difficulties of treating anxious children and their high expectations are among the reasons that increase the stress of dental practitioners even more [13].
A child’s level of cooperation and general behavior is critical for a dentist to choose the most suitable behavioral management approaches, such as tell-show-do, sedation, and general anesthesia [14, 15]. There are some treatment complications with both deep sedation and general anesthesia. Ensuring and maintaining airway patency is vital in the application of sedation. In the application of anesthesia, deep sedation is challenging in dental procedures due to the anatomical proximity of the surgical area to the airway and the risk of microaspiration of water, blood, saliva, and small particles of filling material when working in the open mouth [16]. Dental treatment with general anesthesia is seen as a stressful situation for practitioners since some complications, such as neurological damage, cardiac and respiratory arrest, and even death, may occur [17].
In response to any stress factors in humans, two biological systems are activated: the sympathetic nervous system in the period immediately after exposure to the factor and then the hypothalamic‒pituitary‒adrenal system [18].
In healthy individuals, stimulation of the sympathetic nervous system at the beginning of the stress response begins with the secretion of epinephrine and norepinephrine from the adrenal medulla. These catecholamines cause the characteristic features of sympathetic nervous system activity, such as an increase in heart rate, mydriasis in the pupils, and acceleration of breathing. For this reason, sympathetic activity is measured by various evaluation methods, such as heart rate, blood pressure, and O2 saturation [19]. On the other hand, salivary cortisol has been accepted as a reliable biomarker of the hypothalamus–pituitary–adrenal system as a delayed stress response [20].
A literature review showed that very few studies have investigated occupational stress related to pediatric dentistry [21, 22]. Furthermore, no study was found in which the stress situation in the three treatment protocols (clinical sedation, deep sedation, general anesthesia) was evaluated and compared. In the present study, we aimed to evaluate the stress experienced by dentists while treating children in all three treatment protocols by using objective and subjective (Dentists’ Stress Questionnaire) findings [23]. The null hypothesis (H0) of this study was that there is a statistically significant difference between the stress levels of dentists while treating children with the different treatment protocols.
Materials and methods
Study design
This study was carried out in the University Pediatric Dentistry Department, Oral and Maxillofacial Surgery Operating Room, and Medicine Faculty, Biochemistry Department.
According to the power analysis, the estimated number of samples was determined to be 9 patients in each group (α = 0.05 and 1-β = 0.80). Each dentist treated 27 patients with 3 different treatment approaches, and the study resulted in a total of 108 patients.
Inclusion and exclusion criteria
Dentist standardization
-
- Four dentists, who started their specialization training simultaneously at the Erciyes University Faculty of Dentistry, Department of Pediatric Dentistry, with equal clinical experience and training.
-
- Women
-
- Between the ages of 30 and 33 years
-
- Weight of 52–55 kg
-
- No systemic disease
-
- Dentists who had actively treated patients for at least 2 years in a clinic with deep sedation and general anesthesia were included.
Patient standardization
Children with positive or definitely positive (Frankl 3, 4) behavior according to the Frankl Scale [24], with the data observed in the first session, were included in the clinical treatment group. According to the clinical examination of these patients, 36 healthy children aged 5–6 years who did not require pulpal treatment and whose caries level was 1–4 according to the ICDAS (International Caries Detection and Assessment System) [25] were selected. The type of treatment was determined as compomer fillings applied to 2 primary molars after local anesthesia, and the duration of the treatment was limited to 30–60 min.
Children aged 48–72 months and children with negative or absolutely negative behavior (Frankl 1, 2) according to the Frankl Scale were provided treatment under deep sedation. To provide standardization among patients suitable for sedation, 36 children whose dmft (decayed, missing, filled teeth index) score was less than their age and for whom the duration of the procedure was limited to between 30 and 40 min were included in the study. For general anesthesia, 36 healthy children whose dmft score was equal to or higher than their age were included. In addition, patients whose treatment time was limited to 30–60 min were included.
The patients were randomly assigned to the dentists, and their treatment was carried out. The study did not include children with general health problems or children whose parents refused treatment with general anesthesia/sedation.
For the general anesthesia and deep sedation group, after a minimum of 6 h of fasting, all patients were given midazolam for premedication before they were taken to the operating room. In the operating room, noninvasive standard monitoring was performed for all patients, including heart rate, noninvasive MAP, electrocardiogram, and SpO2.
For the general anesthesia group, 2.5 mg/kg propofol, 0.6 mg/kg rocuronium, and 1 μg/kg fentanyl were used to induce the anesthesia. The most appropriate cuffed endotracheal tube was used for the intubation procedure. Sevoflurane (1 MAC) and a 50% oxygen-air mixture were applied to maintain general anesthesia.
In the deep sedation group, anesthesia was initiated with propofol at a dose of 2 mg/kg. A nasal mask was applied to all patients in this group. The pressure mod of ventilatör was used for noninvasive ventilation during the deep sedation procedure. Additional intermittent propofol was used to achieve the appropriate sedation depth at which the dental treatment and ventilation could be performed comfortably.
Noninvasive mean arterial blood pressure (MAP) and peripheral oxygen saturation (SpO2) were measured by Dräger Fabius Plus (Dräger Medical GmbH, Lübeck, Germany) and recorded 10 min before the dental treatment, at the 25th min of the treatment, and 30 min after the treatment for all three treatment approaches. Also, saliva samples were taken from 4 dentists in the same time intervals for the study. The dentists’ measurement scores compared to each other.
The Saliva Swab Sample Collection (SpeciMAX™, Cat. No. A50696, Thermo Fisher Scientific Inc.) kit was used to collect saliva samples. The swab was placed under the tongue for 2 min, and it was ensured that the swab absorbed the saliva. Afterward, the swab was centrifuged and placed in saliva storage tubes with a perforated chamber for separating saliva and the remaining dry swab. Samples were centrifuged at 3000 rpm for 15 min; the saliva was cleared of debris and then poured into the bottom of the storage tube. Then, the saliva in the plastic saliva storage tube was stored at − 80 °C in an upright position until measurements were made [26]. After the saliva samples were thawed at room temperature on the day of the measurements, they were taken to the University Medical Faculty Central Biochemistry Laboratory for analysis.
Cortisol measurement protocol
Salivary cortisol was measured by the electrochemiluminescence (ECLIA) method using the Cobas Cortisol ll kit (Roche Diagnostics GmbH; Mannheim, Germany).
At the end of each patient’s treatment, after the samples were taken and the measurements were made, the dentists were asked to fill out the “Dentist Job Stress Questionnaire,” consisting of 6 questions reflecting their current stress [23]. In the questionnaire, questions were asked to measure the physician’s current degree of work stress, and they were asked to choose the most suitable option for them.
Statistics
In the study, the analyses were made with the SPSS 25.0 program. Histograms, q–q plots, and Shapiro‒Wilk’s test were applied to assess data normality. Descriptive statistics are presented as the mean and standard deviation. The Kruskal‒Wallis test was performed to examine the differences in measurements according to the dentists and treatment approaches. The Mann‒Whitney U test was used to reveal the evaluation causing the difference. The Friedman test was used to examine the differences among the measurements in the treatment approaches before, during, and after the procedures. The Wilcoxon method was used to determine the time causing the difference. To test the reliability levels of the question groups in the study, the Co. Alpha analysis was applied. Spearman correlation analysis was applied to determine the relationship between stress levels and biological parameters. P values less than 0.05 were considered statistically significant in the study.
Results
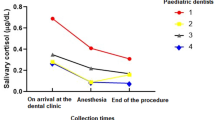
When the findings were evaluated according to the measurement times, systolic and diastolic blood pressure measurements for all dentists before the procedure were similar in the clinical, general anesthesia, and deep sedation groups (P > 0.05). Both systolic and diastolic blood pressure measurements were found to be higher in the deep sedation group (P < 0.05). It was determined that the systolic blood pressure measurements after treatment did not differ among the clinical, general anesthesia, or deep sedation groups (P > 0.05), but the diastolic blood pressure measurements did. The measurements of the deep sedation group were higher than those of the clinical sedation and general anesthesia groups (P < 0.05). Heart rate and oxygen saturation measurements before, during, and after the treatment did not differ among the clinical sedation, general anesthesia, and deep sedation groups (P > 0.05). It was observed that cortisol measurements before and during treatment were not at different levels among the clinical sedation, general anesthesia, and deep sedation groups (P > 0.05). After treatment, the cortisol measurements in the deep sedation group were higher than those in the clinical and general anesthesia groups (P < 0.05) (Table 1).
When the systolic and diastolic blood pressure measurements were examined according to the procedure times, it was observed that the systolic and diastolic blood pressure measurements were similar before, during, and after treatment in the clinical and general anesthesia groups (P > 0.05). In the deep sedation group, systolic and diastolic blood pressures measured during the procedure were shown to be high.
The heart rate measurements were at similar levels before, during, and after treatment in the clinical and general anesthesia groups (P > 0.05). In the deep sedation group, it was determined that the heart rate measurements during the procedure were higher than those before and after the procedure (P < 0.05).
When the authors evaluated the oxygen saturation measurements, the oxygen saturation value during the procedure was lower than that before and after the procedure (P < 0.05).
Cortisol measurements were found to be at different levels according to the processing times shown in Table 2 (P < 0.05).
It was determined that the stress levels obtained by using the applied questionnaire differed among the clinical sedation, general anesthesia, and deep sedation groups. It was observed that the stress level of the dentists in the deep sedation group was higher than that of dentists in the clinical sedation and general anesthesia groups (P < 0.05).
In this study, there was a correlation between the stress level and systolic blood pressure values of the dentists in the clinical sedation, general anesthesia, and deep sedation groups before and after the procedure (P < 0.05). According to the survey results, the preprocedural systolic blood pressures of the dentists reporting high stress levels were higher.
It was determined that the stress level of dentists during the protocols and the systolic blood pressure and heart rate measurements were moderately strong and positively correlated (P < 0.05) (Table 3).
The relationship between the stress level of the dentists and oxygen saturation and cortisol values are shown in Table 4.
The study showed that systolic and diastolic blood pressure values and heart rate measurements differed among dentists before, during, and after treatment. It was observed that the difference was because dentist-1 had higher systolic and diastolic blood pressure values and heart rate measurements than all the other dentists (P < 0.05). Oxygen saturation and salivary cortisol measurements before, during, and after treatment were found to be at similar levels in all dentists (P > 0.05) (Table 5).
Discussion
Several studies related to occupational stress have been conducted among dentists [26, 27]. In healthy individuals, some physiological changes occur due to exposure to stress, with the secretion of adrenaline at the beginning of stress, and various values such as heart rate and blood pressure increase [19].
On the other hand, salivary cortisol is accepted as a reliable biomarker of the hypothalamus–pituitary–adrenal system as a delayed stress response [20]. In addition, cortisol measurements have advantages such as noninvasiveness of the measurement, easy sampling during an individual’s daily activities, and no long preliminary preparation phase for the samples [28].
Anabuki et al. used cortisol measurements in stress evaluation in addition to questionnaire evaluations in their study of providing treatment with moderate sedation [21]. Compared to the previous study, in which the stress levels that pediatric dentists were exposed to while providing treatment with 3 different treatment approaches were measured, in the present study, we aimed to make additional measurements that determined stress occurring during treatment via objective data.
In the literature, although some studies have measured the occupational stress and burnout of dentists [7, 23], no studies have investigated the effects of different treatment approaches on stress. Therefore, comparing the present study with related research is not easy. For example, in the study by Ronneberg et al. [22], which evaluated the stress levels of dentists during the application of various procedures and treatments for patients, they stated that dentists were more stressed when treating pediatric patients. Therefore, dentists specializing in the treatment of pediatric patients were included in the study.
When the results were examined, it was observed that the O2 saturation values of the dentists in all 3 treatment approach groups decreased during the procedure. In the literature, it is reported to be difficult for dentists to work with reinforced protective equipment during the pandemic [28]. Therefore, in this study, we assumed that the decrease in O2 saturation values may be because the study was carried out during the COVID-19 pandemic since dentists worked with extra protective equipment such as N95 masks, surgical masks, glasses, and shields.
In the current study, different results were obtained regarding the cortisol values of the dentists in the 3 treatment approach groups. It was found that the postprocedure salivary cortisol values of the dentists were lower than the values obtained before and during treatment while caring for patients in the clinic. Gomes et al. showed that even if pediatric patients have no dental experience, they become stressed, and their cortisol levels increase even with noninvasive treatments such as professional dental prophylaxis. Professional dental prophylaxis increases salivary cortisol in children with dental behavioral management problems: a longitudinal study [29]. In addition, the difficulties experienced while treating a pediatric patient may not always be related to dental anxiety. It has been shown that children, even under midazolam sedation, may not cooperate with a dental procedure without experiencing dental anxiety. Oral midazolam reduces cortisol levels during local anesthesia in children: a randomized controlled trial [30]. Ronnenberg et al. reported that the negative behaviors of pediatric patients during treatment caused stress for dentists [22]. Additionally, in studies, dentists and students stated that they were stressed while applying local anesthesia and restorative treatment in a clinic [31]. In this study, we think that the dentists were stressed before and during the procedure because they did not know what kind of patient they would encounter before providing treatment in the clinic. They were worried that the treatment would be unsuccessful due to the unexpected reactions of the pediatric patients. The compatibility of the pediatric patients can be seen as a reason for the decrease in posttreatment cortisol values. For this reason, stress at the end of the treatment may have decreased since no adverse events occurred during the procedures.
When the patients were treated under general anesthesia, it was observed that the salivary cortisol values before treatment were higher than the values obtained during and after treatment. It is thought that the decrease in the salivary cortisol value during treatment with general anesthesia is because this treatment approach is safer for the dentist treating the pediatric patient: the dentist can work without the requirement of giving commands, since the patient is completely under control.
Anabuki et al. [21] concluded in their study that the salivary cortisol values of pediatric dentists using moderate sedation decreased during treatment. The reason for this decrease was explained by the fact that although the dentists included in the study stated that they were stressed in the questionnaire, they did not give physiological responses as a result of getting used to their work routines. In this study, when the salivary cortisol values were examined for moderate sedation, it was determined that this value increased during the procedure. This result demonstrates that dentists are more stressed when applying treatment with moderate sedation. Rasmussen et al. [31], Davidovich et al. [32], and Ronnenberg et al. [33] reported that experience is an important factor in reducing stress. Dentists specializing in pediatric dentistry were included in this study, while specialist dentists were evaluated in the study of Anabuki et al. The difference in the experience of the pediatric dentists may have led to these different results [21].
Song et al. revealed that general occupational stress in dentists stems from interpersonal relationships with patients and that a specialist’s responsibilities, rather than their workload, have a significant relationship with stress [23]. This study determined that dentists were more nervous during sedation treatment according to the survey results, consistent with the objective results. Since compatible patients were selected for clinical sedation in the study, we think that there was no stress arising from the relationship with the patient. However, as Song et al. [23] mentioned in their study, stress may occur when using general anesthesia and especially deep sedation due to the burden of responsibility for the patient.
Occupational stress and factors affecting burnout are related to personal factors as well as external factors such as workload and workplace [34]. Considering the results obtained in this study, the authors observed that the stress symptoms of dentist-1, measured before, during, and after treatment with all treatment protocols, were higher than those of the other included dentists. Although standardization was attempted in the study, the reason why the values of one of the dentists were higher than those of the other dentists can be explained by the fact that the stress factor is personal, although it also depends on the treatment approach and additional factors.
This study should be evaluated in light of some limitations. The first is that including more dentists with different training and experience in the study may have led to different results. Second, measuring the daily stress values of the dentists (e.g., trait anxiety, chronic stress) may contribute to the reliability of the results.
Within the scope of the study, compatible children were included in the clinical treatment group in terms of standardization of the treatment duration, but it is a limitation that a noncompatible group was not included in the study.
In conclusion, it has been determined that dentists who care for pediatric patients are more stressed when providing treatment under deep sedation.
The study provides information on the stress caused by routine treatment approaches in the practice of pediatric dentistry. Therefore, the stress of pediatric dentists is clinically important. It is known that occupational stress also affects functional abilities. To reduce stress, it is important to first determine in which situation and treatment approach it occurs more. In this way, measures can be taken to increase the health and treatment quality of dentists, who spend most of the day providing dental treatment for children.
References
Contrada R, Baum A (eds) (2011). Springer Publishing Company
Basu S, Qayyum H, Mason S (2017) Occupational stress in the ED: a systematic literature review. Emerg Med J 34(7):441–447. https://doi.org/10.1136/emermed-2016-205827. (PMID: 27729392)
Riley GJ (2004) Understanding the stresses and strains of being a doctor. Med J Aust 181(7):350–353. https://doi.org/10.5694/j.1326-5377.2004.tb06322.x. (PMID: 15462646)
Kansoun Z, Boyer L, Hodgkinson M, Villes V, Lançon C, Fond G (2019) Burnout in French physicians: a systematic review and meta-analysis. J Affect Disord 246:132–147. https://doi.org/10.1016/j.jad.2018.12.056. (PMID: 30580199)
Williams ES, Rathert C, Buttigieg SC (2020) The personal and professional consequences of physician burnout: a systematic review of the literature. Med Care Res Rev 77(5):371–386. https://doi.org/10.1177/1077558719856787. (PMID: 31216940)
Quick JC, Henderson DF (2016) Occupational stress: preventing suffering, enhancing wellbeing. Int J Environ Res Public Health 13(5):459. https://doi.org/10.3390/ijerph13050459. (PMID: 27136575; PMCID:PMC4881084)
O’Shea RM, Corah NL, Ayer WA (1984) Sources of dentists’ stress. J Am Dent Assoc 109(1):48–51. https://doi.org/10.14219/jada.archive.1984.0282. (PMID: 6589290)
Gale EN (1998) Stress in dentistry. N Y State Dent J 64(8):30–34 (PMID: 9828615)
Hakanen JJ, Bakker AB, Demerouti E (2005) How dentists cope with their job demands and stay engaged: the moderating role of job resources. Eur J Oral Sci 113(6):479–487. https://doi.org/10.1111/j.1600-0722.2005.00250.x. (PMID: 16324137)
Klingberg G, Berggren U, Carlsson SG, Noren JG (1995) Child dental fear: cause-related factors and clinical effects. Eur J Oral Sci 103(6):405–412. https://doi.org/10.1111/j.16000722.1995.tb01865.x. (PMID: 8747678)
Lowe O (2013) Communicating with parents and children in the dental office. J Calif Dent Assoc 41(8):597–601 (PMID: 24073498)
Diercke K, Ollinger I, Bermejo JL, Stucke K, Lux CJ, Brunner M (2012) Dental fear in children and adolescents: a comparison of forms of anxiety management practised by general and paediatric dentists. Int J Paediatr Dent 22(1):60–67. https://doi.org/10.1111/j.1365263X.2011.01158.x. (Epub 2011 Jul 18. PMID: 21762409)
Rada RE, Johnson-Leong C (2004) Stress, burnout, anxiety and depression among dentists. J Am Dent Assoc. 135(6):788–794. https://doi.org/10.14219/jada.archive.2004.0279. (PMID: 15270165.)
American Academy on Pediatric Dentistry (2008) American Academy of Pediatrics Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent 30(7Suppl):40–43 (PMID: 19216381)
Wilson S, Nathan JE (2011) A survey study of sedation training in advanced pediatric dentistry programs: thoughts of program directors and students. Pediatr Dent 33(4):353–360 (PMID: 21903005)
Coté CJ, Wilson S (2019) Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures. Pediatr Dent 41(4):26–52 (PMID: 31439094)
Lee HH, Milgrom P, Starks H, Burke W (2013) Trends in death associated with pediatric dental sedation and general anesthesia. Paediatr Anaesth 23(8):741–746. https://doi.org/10.1111/pan.12210. (Epub 2013 Jun 14. PMID:23763673; PMCID: PMC3712625)
Chrousos GP (2009) Stress and disorders of the stress system. Nat Rev Endocrinol 5(7):374–381. https://doi.org/10.1038/nrendo.2009.106. (Epub 2009 Jun 2. PMID: 19488073)
Skosnik PD, Chatterton RT Jr, Swisher T, Park S (2000) Modulation of attentional inhibition by norepinephrine and cortisol after psychological stress. Int J Psychophysiol 36(1):59–68. https://doi.org/10.1016/s0167-8760(99)00100-2. (PMID: 10700623)
Kirschbaum C, Hellhammer DH (2007) Salivary cortisol. In: Fink G (ed) Encyclopedia of Stress, 2nd edn. Academic Press, New York, pp 405–409
Anabuki AA, Corrêa-Faria P, Batista AC, Costa LR (2021) Paediatric dentists’ stress during dental care for children under sedation: a cross-sectional study. Eur Arch Paediatr Dent 22(2):301–306. https://doi.org/10.1007/s40368-020-00565-3
Ronneberg A, Strøm K, Skaare AB, Willumsen T, Espelid I (2015) Dentists’ self-perceived stress and difficulties when performing restorative treatment in children. Eur Arch Paediatr Dent 16(4):341–347. https://doi.org/10.1007/s40368-014-0168-2. (PMID: 25628090)
Song KW, Kim HK (2019) Job stress and its related factors among Korean dentists: an online survey study. Int Dent J 69(6):436–444. https://doi.org/10.1111/idj.12513. (PMID: 31388997)
Riba H, Al-Zahrani S, Al-Buqmi N, Al-Jundi A (2017) A review of behavior evaluation scales in pediatric dentistry and suggested modification to the Frankl scale. EC Dent Sci 16:269–75
Ismail AI, Sohn W, Tellez M et al (2007) The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol 35(3):170–178. https://doi.org/10.1111/j.1600-0528.2007.00347.x
Elbuken G, Tanriverdi F, Karaca Z et al (2015) Comparison of salivary and calculated free cortisol levels during low and standard dose of ACTH stimulation tests in healthy volunteers. Endocrine 48(2):439–443. https://doi.org/10.1007/s12020-014-0378-8. (Erratum in: (2015) Endocrine. Dec;50(3):830. PMID: 25115637)
Choy HB, Wong MC (2017) Occupational stress and burnout among Hong Kong dentists. Hong Kong Med J 23(5):480–488. https://doi.org/10.12809/hkmj166143. (PMID: 28839120)
Erickson MM, Richardson ES, Hernandez NM, Bobbert DW 2nd, Gall K, Fearis P (2020) Helmet modification to PPE with 3D printing during the COVID-19 pandemic at Duke University Medical Center: a novel technique. J Arthroplasty 35(7):23–27. https://doi.org/10.1016/j.arth.2020.04.035.PMID:32354536;PMCID:PMC7166108
Gomes HS, Vieira LA, Costa PS, Batista AC, Costa LR (2016) Professional dental prophylaxis increases salivary cortisol in children with dental behavioural management problems: a longitudinal study. BMC Oral Health 16(1):74. https://doi.org/10.1186/s12903-016-0273-1. (PMCID: PMC4989520)
Gomes HS, Corrêa-Faria P, Silva TA et al (2015) Oral midazolam reduces cortisol levels during local anaesthesia in children a randomised controlled trial. Braz Oral Res 29:S1806-S8.32420150001003E16. https://doi.org/10.1590/1807-3107BOR-2015.vol29.0125. (PMID: 26892359)
Rasmussen JK, Frederiksen JA, Hallonsten AL, Poulsen S (2005) Danish dentists’ knowledge, attitudes and management of procedural dental pain in children: association with demographic characteristics, structural factors, perceived stress during the administration of local analgesia and their tolerance towards pain. Int J Paediatr Dent 15(3):159–168. https://doi.org/10.1111/j.1365-263X.2005.00635.x. (PMID: 15854111)
Davidovich E, Pessov Y, Baniel A, Ram D (2015) Levels of stress among general practitioners, students and specialists in pediatric dentistry during dental treatment. J Clin Pediatr Dent 39(5):419–422. https://doi.org/10.17796/1053-4628-39.5.419. (PMID: 26551363)
Ronneberg A, Strøm K, Skaare AB, Willumsen T, Espelid I (2015) Dentists’ self-perceived stress and difficulties when performing restorative treatment in children. Eur Arch Paediatr Dent 16(4):341–347. https://doi.org/10.1007/s40368-014-0168-2. (PMID: 25628090)
Kelly M, Soles R, Garcia E, Kundu I (2020) Job stress, burnout, work-life balance, well-being, and job satisfaction among pathology residents and fellows. Am J Clin Pathol 153(4):449–469. https://doi.org/10.1093/ajcp/aqaa013. (PMID: 32080717)
Author information
Authors and Affiliations
Contributions
EK conceived the idea for the research, prepared samples for analyses, wrote the initial framework, and drafted the manuscript as the principal author. FK, TM, SM, and KK prepared samples for analyses, wrote the initial framework, and revised the manuscript. SM made the biochemistry analysis and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained from the Clinical Research Ethics Committee in Erciyes University School of Medicine (ethics number: 2021/32). The written consent was obtained from all the parents confirming that they would provide their children’s extracted primary teeth for the research, and they would allow it to be published.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kızılcı, E., Kızılay, F., Mahyaddinova, T. et al. Stress levels of a group of dentists while providing dental care under clinical, deep sedation, and general anesthesia. Clin Oral Invest 27, 3601–3609 (2023). https://doi.org/10.1007/s00784-023-04973-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04973-9