Abstract
Objectives
Stability values of mini-implants (MIs) are ambiguous. Survival data for MIs as supplementary abutments in reduced dentitions are not available. The aim of this explorative research was to estimate the 3-year stability and survival of strategic MIs after immediate and delayed loading by existing removable partial dentures (RPDs).
Material and methods
In a university and three dental practices, patients with unfavorable tooth distributions received supplementary MIs with diameters of 1.8, 2.1, and 2.4 mm. The participants were randomly allocated to group A (if the insertion torque ≥ 35 Ncm: immediate loading by housings; otherwise, immediate loading by RPD soft relining was performed) or delayed loading group B. Periotest values (PTVs) and resonance frequency analysis (RFA) values were longitudinally compared using mixed models.
Results
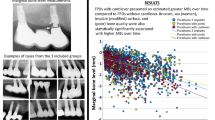
A total of 112 maxillary and 120 mandibular MIs were placed under 79 RPDs (31 maxillae). The 1st and 3rd quartile of the PTVs ranged between 1.7 and 7.8, and the RFA values ranged between 30 and 46 with nonrelevant group differences. The 3-year survival rates were 92% in group A versus 95% in group B and 99% in the mandible (one failure) versus 87% in the maxilla (eleven failures among four participants).
Conclusions
Within the limitations of explorative analyses, there were no relevant differences between immediate and delayed loading regarding survival or stability of strategic MIs.
Clinical relevance
The stability values for MIs are lower than for conventional implants. The MI failure rate in the maxilla is higher than in the mandible with cluster failure participants.
Clinical trial registration
German Clinical Trials Register (Deutsches Register Klinischer Studien, DRKS-ID: DRKS00007589, www.germanctr.de), January 15, 2015.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In jaws with few remaining teeth or unfavorable distribution between quadrants, strategic dental implants can serve as supplementary abutments for a symmetric support and more stability of removable partial dentures (RPD) [1,2,3,4,5]. Posterior-placed implants are also used to support distal extension RPDs [6,7,8,9]. Implants can be placed either before the fabrication of the new prosthesis [1, 2] or under an existing RPD [3, 5,6,7,8,9]. Latter studies showed improvements of the RPD function, i.e., chewing efficiency [3, 6, 9], and of patient-immanent factors such as satisfaction with the denture [3, 7, 8], quality of life [5], or nutrient intake [6]. The connection of teeth and implants is still considered as controversial due to the different movement behaviors of natural and artificial abutments, particularly under fixed prostheses [4]. However, this combination is a reliable and predictable treatment modality in RPDs even when different attachments, e.g., double crowns or clasps on teeth and ball attachment on implants, are used [4, 8, 10]. A systematic literature review of combined teeth and implant-retained RPDs revealed implant survival rates between 91.7 and 100% after 2 to 10 years of observation [10]. In a meta-analysis of studies with double crown-retained RPDs supported by implants and teeth, the overall survival rate of implants was 98.7% (95% confidence interval [95% CI]: 97–99.8%) after at least 3 years [11].
Unfortunately, conventional two-piece implants are cost-intensive and sometimes require bone augmentation procedures in narrow alveolar ridges. One-piece mini-implants (MIs) with diameters of 1.8 to 2.9 mm are mainly indicated in atrophied ridges with insufficient width to stabilize removable dentures. Thus, MIs may reduce the invasiveness of the surgical intervention with subsequently less postoperative morbidity and the primary treatment cost [12]. Therefore, MIs are especially suitable for medically compromised and/or financially restricted patients [12,13,14,15]. Hereby, especially elderly patients who refuse complex interventions could be encouraged to choose implant-supported rehabilitations [13].
Because of the one-piece design, a total no-load secondary osseointegration is not possible in the edentulous jaws as their main indication. However, this design should prevent microbiological leakage into the surrounding implant tissue [16, 17].
Primary stability seems to be a key factor for successful osseointegration, especially for immediately loaded implants [18]. Therefore, the assessment of MI stability could be a supplementary tool to other clinical or radiographic examination to monitor successful primary and secondary osseointegration [19]. Previous stability data of mandibular MIs using the Periotest device were inconsistent. The mean Periotest values (PVTs) were either in the range of two-piece standard-diameter implants, i.e., < 0 [20, 21], or ranged between + 2 and + 7 [22, 23].
According to some reviews, MI-supported overdentures are a viable and safe treatment option for edentulous mandibular arches with mid-term survival rates > 90%, which is similar to standard-diameter implants [12, 13, 24, 25]. However, the results for immediate loaded MIs to support maxillary overdentures are unfavorable, with survival rates below 80% [13, 14]. Another progressive loading concept involves an initial soft relining of the dentures for 3 to 6 months followed by the connection with the matrices [15, 26]. The survival rates of maxillary MIs were 82.3% after 3 years in a prospective study [26] and 94.3% after 4 years in a retrospective analysis [15]. Prospective studies of strategic MIs under RPDs are extremely rare [13, 27]. There are some short-time observations of MIs for the anterior fixation of free-end RPDs [28, 29].
Meanwhile, a 3-year randomized clinical trial (RCT) was completed, comparing immediate with delayed loading of strategic MIs under existing RPDs with unfavorable tooth distribution [30]. The primary outcome was the radiological bone level change at MIs. First evaluations found marked improvements in the chewing efficiency [31] and patient satisfaction with their RPDs [32]. The improvements occurred faster after immediate loading than delayed MI loading.
The aims of the present explorative analyses were (1) to describe the longitudinal stability values for MIs under different loading conditions, (2) to estimate the MI survival rates, and (3) to evaluate whether PTVs can predict MI losses. We hypothesized less initial MI stability and more MI failures in the immediate than in the delayed loading group as in the study protocol [30].
Material and methods
Study procedures
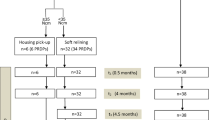
This multicenter RCT in a university hospital and three dental practices was approved by the Ethics Committee of the Greifswald University (BB 058/13A). All participants gave their written informed consent prior to inclusion in the study. Participants were patients with an RPD in one or both jaws with comparably unfavorable tooth distributions, i.e., one quadrant was edentulous (class 0), or one/both quadrants had either only anterior teeth (class 1), one (class 2), or at most two posterior teeth (class 3) and no canine (Fig. 1). The quadrant with the lowest class number determines the classification of the study jaw. The sample size calculation is based on bone level changes as the primary outcome and resulted in 26 participants per group. One-piece MIs (Mini Dental Implant, MDI, Manufacturer in the past 3 M ESPE and now Condent, Germany) with diameters of 1.8, 2.1, and 2.4 mm; lengths of 10, 13, and 15 mm; and ball attachments were inserted according to the quality and quantity of the available jaw bone. The participants received as many MIs from experienced dentists until either two abutments per quadrant (teeth plus MI) in the mandible or three abutments per quadrant in the maxilla were in place (Figs. 1 and 2). The higher maxillary abutment number corresponds with recommendations of researchers, clinicians, and manufacturers for MIs in the edentulous jaws [14].
The RPD was hollowed out over the ball abutments. Thereafter, the participants were allocated to the immediate loading group A or the delayed loading group B according to the 1:1 randomization ratio stratified by jaw and center. A sealed opaque envelope with the randomization detail was usually opened by the treatment coordinator. The surgeon was informed per telephone about the group allocation after implant placement. According to previous good experiences [15] and to the manufacturer guideline, immediate loading with matrices (O-ring housings) was only performed provided ≥ 35 Ncm insertion torque of all MIs. Alternatively, the RPD was soft relined, embracing the MI balls. In group B, the MIs were kept without loading for 4 months. Subsequently, the O-ring housings were picked-up in both group B and the soft relined RPDs in group A (Fig. 2).
Data assessment
An independent expert dentist examined the patients before the surgery (T−1), after 2 weeks (T1), 4 months (T2), 4.5 months (T3, after housing pick-up for the patients with soft relined RPDs of group A and all patients of group B), 1 year (T4), 2 years (T5), and 3 years (T6). Additionally, the stability values just after MI placement (T0) were measured in the university hospital since there was only one trained examiner with the calibrated devices attended at the time of surgery.
Implants that soundly maintained their function were considered to have survived. Removals or spontaneous losses of implants were defined as failure [33].
The Periotest instrument (Medizintechnik Gulden, Bensheim, Germany) was used to measure MI stability [34, 35]. A percussion rod impacts at right angles to the middle of the MI ball attachment 16 times for 4 s (Fig. 3).
The more stable the bone anchorage, the quicker the percussion is. The instrument measures the time that the percussion rod is in contact, with a shorter contact time indicating more stability. The computer converts the information to the Periotest value (PTV) on a scale between − 8 and + 50. PTVs below 0 are intended to be indicative for osseointegrated conventional implants [34].
Resonance frequency analysis (RFA) with the Osstell device (Osstell, Gothenburg, Sweden) was additionally used to measure MI stability [19, 34, 35]. The former manufacturer of the MI system for this study developed a SmartPeg prototype. The SmartPeg was put on the MI and fixed below the ball equator with a lateral screw (Fig. 3). The probe of a handpiece stimulates the SmartPeg that produces lateral stress in increasing frequency until the implant vibrates. The resonance was recorded and displayed by the measuring device. The implant stability quotient (ISQ) indicates the resonance frequency on a scale of 1–100. ISQ and implant stability are positively correlated. Most of the studies found mean RFA values of > 60 for conventional implants at surgery followed by a slight increase over time [19].
Statistical analyses
Continuous variables are represented as median (1st–3rd quartile) because of asymmetric data distributions. To compare stability values between the treatment groups, mixed models were used on three levels, namely person, tooth site, and time as continuous variable [36]. The interaction between treatment and time was adjusted for sex, age, jaw, tooth site, and center [37]. Deviations from linearity for “time” were modeled by restricted cubic splines with three knots [38]. The tolerance limits of non-inferiority of immediately loaded MI versus delayed loaded MI were set at + 1 unit PTV and at − 2.5 units ISQ.
The Kaplan–Meier analyses were performed as descriptive statistics assuming independent observations. However, the Cox regression considered dependence among implants from the same patient by robust variances [33]. Defined α-levels were not regarded, and 95% CIs are primary presented to follow the recommendations of the American Statistical Association [39]. All statistical analyses were performed using Stata (Stata, Version 16.1; Stata Corporation, College Station, TX, USA).
Results
Participant’s characteristics
Because one of the participating surgeons had a long-term illness, 12 participants received no MI in the study period (Fig. 4).
The recruitment period ranged between January 2014 and July 2015. The study ended in July 2018. The new or optimized RPDs of the 79 study jaws (31 maxillae) were either double crown-retained (n = 52), retained by double crowns and clasps (n = 15), clasp-retained (n = 10), or precision attachment-retained (n = 2) which were worn for at least 2 months. The median of the residual teeth was two in the maxilla (1st quartile = 2; 3rd quartile = 4) and three in the mandible (1st quartile = 2; 3rd quartile = 5). Participants with study maxillae showed on the opposing jaw: RPDs (n = 19), fixed dental prostheses (n = 9), or natural dentition (n = 3). Participants with study mandibles showed on the opposing jaw: complete dentures (n = 10), RPDs (n = 30), or fixed dental prostheses (n = 8). A total of 112 maxillary (median 3 per jaw) and 120 mandibular (median 2 per jaw) MIs were placed. Three participants received MIs in the maxilla and mandible. As seen in the flow chart (Fig. 4), each 38 participants were allocated to groups A (mean age 66.4 years, 22 women) and B (mean age 65.4 years, 25 women). In group A, 12 maxillary and 22 mandibular RPDs were primarily soft relined because the insertion torque of at least one MI was < 35 Ncm. The MIs of three maxillae and three mandibles were immediately loaded with housings (insertion torque ≥ 35 Ncm). The MIs of 16 maxillae and 23 mandibles in group B were delayed loaded. A total of six participants in group A (16%) and seven participants in group B (18%) were lost to follow-up in the whole study period, among them each two per group until the second year. Figure 5 shows the distribution by tooth site and MI diameter. In the maxilla, MIs with a diameter of 2.4 mm were predominantly placed, whereas in the mandible, the diameter of 2.1 mm and 1.8 mm predominated.
Mini-implants stability
The median of maximum insertion torque of 222 MI was 25 Ncm (1st quartile, 20 Ncm; 3rd quartile, 35 Ncm). The different number of stability measurements and the higher number of PTVs compared with RFA values (total number 1270 versus 897), especially after the first year, has several reasons (Table 1).
First, the response rate for visits of the participants varied between follow-up points. Second, just after surgery (T0), stability values were available in the university hospital exclusively. Third, if the mucosa covered the MI insertion square, a safe fixation of the SmartPeg and subsequent measurement was sometimes impossible. Fourth, during the second year of the study, the manufacturer transferred the fabrication of the MI system to another company, and supplies of SmartPegs were stopped. Therefore, 3-year RFA measurements were not conducted contrary to the original study protocol. According to Table 1, primary PTV and RFA values from the university hospital suggest the highest MI stability at the day of placement.
The adjusted values and 95% CIs of the follow-ups by groups in Figs. 6 and 7 correspond with women, age of 65 years, mandible, first premolar site, and first study center. Assuming a tolerance limit of + 1 for PTVs, the immediately loaded MI of group A showed no inferiority compared with delayed loaded MIs of group B (Fig. 6), and the differences between groups are statistically not significant (P = 0.788). The 95% CI after 3 years is compatible with effects between − 1.4 (in behalf of group B) and 1.9 (in behalf of A). Similar results were obtained for the RFA values (Fig. 6). The 95% CI after 2 years is compatible with effects between − 5.2 (in behalf of group B) and 2.0 (in behalf of A) without a statistically significant difference (P = 0.390). However, in the first year of observation, PTVs tended to be higher, and RFA values tended to be lower with wide overlapping 95% CIs for the immediately loaded MIs of group A compared to group B. The values of the groups converged after the first year.
The Spearman correlation of rs = − 0.83 between PTV und RFA values (n = 887) suggests a high negative correlation on condition of independent observations. The negative correlation of the maximum insertion torque with PTVs was weak (rs = − 0.15), whereas the positive correlation with RFA values was moderate (rs = 0.24) as seen in Fig. 8.
Figure 9 shows the PTVs by MI diameter and length in the maxilla and mandible at the 1-year follow-up. The diameters of 1.8 and 2.1 mm are pooled because of the low number of the thinnest MIs. The stability of 2.4 mm MIs was higher (mean PTV for all lengths together: 4.1 in the maxilla and − 0.3 in the mandible) than the stability of MIs with lower diameters (mean PTV for all lengths together: 9.8 in the maxilla and 4.7 in the mandible). The differences between MI lengths were negligible.
Mini-implants survival rate
A total of 8 failures were registered in three participants of group A versus 5 failures in two participants of group B, which resulted in cumulative 3-year survival rates of 92% versus 95% (Fig. 10). In group A, one maxillary MI was misplaced and could not be covered by the RPD because of its buccal malposition. This MI was immediately removed. All other MI failed due to lost osseointegration. Each three losses in three maxillae, two losses in one other maxilla, the malpositioned MI, and another loss in one mandible yield MI survival rates of 87% for maxillary and 99% for mandibular MIs (Fig. 11).
According to Cox regression analyses considering dependent observations within one person, the 95% CI for the difference between the groups was 0.1 to 3.4 (hazard ratio [HR] = 0.6, P = 0.554). The 95% CI for the difference between the jaws was 1.6–142.2 (HR = 15.3; P = 0.017). Participants with MI losses wore either RPDs with multiple abutments (n = 3) or had natural dentitions (n = 2) in the opposing jaw. One patient with three MI losses was a current heavy smoker, and the other patients with MI losses were never smokers. The lost mandibular MI was placed in a fresh extraction socket contrary to all other MIs. MI failures were either spontaneous losses during removing the RPD at home (n = 6) or MI loosenings (n = 6) with subsequent removal without any severe inflammatory reaction of the peri-implant tissue or pronounced bone defects.
Periotest values and implant survival
The majority of PTVs for failed MIs (8 out of 12) showed an increase between 2 weeks after placement (T1) and the follow-up before the loss (Table 2). According to Cox regression analyses, plus one unit PTV increases the failure risk (HR = 1.23; 95% CI = 1.15–1.31; P < 0.001). An increase of 5, 10, and 15 units of PTV results in HRs of 1.8, 7.9, and 22.0. Transformed in curves, the 3-year survival rate probability decreased from 97% in a PTV difference of 5 to 92% in a difference of 10 units (Fig. 12).
Discussion
The primary outcome of this randomized trial was bone level changes of either immediately loaded MI in group A or delayed loaded MI in group B as supplementary abutments under existing RPDs. The assessment of bone heights at MIs on the panoramic radiographs are more sophisticated than expected, and the analyses are still pending. Thus, the present findings are descriptive and explorative in nature and not based on formal statistical hypothesis testing. The outcomes suggest no relevant differences between immediate and delayed loading regarding the survival rate and the stability of strategic MIs contrary to our hypotheses. The median of MI PTVs was higher, and the median of RFA values was lower than the stability values of standard-diameter implants whereby MI PTVs and RFA values strongly correlated. The correlation between insertion torque of MIs and their measured primary stability was rather moderate. The 3-year survival rate of mandibular MIs was markedly higher than of maxillary MIs (99% versus 87%, respectively). The expected relationship between increasing PTVs and the risk of implant loss was confirmed.
Some limitations of the trial besides participant`s response merit consideration. First, both upper and lower jaws with various tooth distributions were included. However, it was given that the few remaining teeth provided insufficient and/or imbalanced support for the RPD. Second, the different loading procedures dependent on insertion torque of MIs in group A limit a sound comparison with group B. We would reduce the risk of implant failures in the maxilla as seen in studies in which all maxillary MIs were immediately loaded with the housings [40, 41]. Third, the selection of the respective MI for every individual site depended on the bone height regarding the length. The quality and thickness of the bone determined the MI diameter as in clinical routine. Therefore, the thickest MIs with wide thread flanks were more frequently used in the spongier maxilla and thinner MIs predominated in the more cortical mandible according to the manufacturer instructions and to a number of studies [13, 14]. Thus, MI stability comparisons between maxillae and mandibles are less conclusive. Furthermore, different treatment strategies for maxilla and mandible were evaluated by using survival estimations since the MI number and their dimensions varied by jaw. However, the loading conditions of the MIs between patients should be comparable since the total number and distribution of RPD abutments were similar after MI placement. Fourth, our SmartPeg prototype was not validated, and after the second year, new SmartPegs were no longer available. Therefore, we dispensed with 3-year RFA measurements altogether.
Overall, this is the first estimation of mid-term survival rate and stability data for strategic MIs stabilizing RPDs with unfavorable distribution of natural abutments. Because of the multicenter design (one university hospital and three private practices), a multifaceted patient cohort was treated by experienced dental practitioners and examined by one trained investigator who was not involved in the treatment. The MIs were placed without knowing the loading modus up to the participant’s allocation. For MI stability assessments, two different methods were used whose values strongly negatively correlated.
As hypothesized in the design paper [30], there was a trend for lower stability of immediately loaded MIs compared to delayed loaded MIs in the first year of observation. This could be explained by the occlusal and lateral forces of the RPDs on the MI in the bone remodeling period [18]. As seen by overlapping 95% CIs, any difference between the groups could not be proven by the present data. After the first year, the values of group A conformed to group B. The slight increase of the RFA values in both groups and the decrease of the PTVs in group A correspond with prospective studies using conventional implants [19]. In observational studies using immediately loaded MI in edentulous mandibles, the PTVs remained either relatively constant [20] or increased in the first 4 months followed by a slight decrease [23].
The reference levels for the stability of conventional implants in a successful osseointegration are PTVs < 1 and RFA values > 60 [19, 35]. In the present study, the median PTV of 4.5 after 3 years and the median ISQ of 41.5 after 2 years indicate an insufficient stability for prosthetic loading. Because of their deflection during the measuring procedure, MIs may have other stability values than two-piece implants with diameters ≥ 3 mm. This conjecture is supported by the trend for a higher stability of the thicker MI in our trial and by two other studies with mandibular MIs of similar dimensions. The studies showed mean PTVs of 6 ± 6 [23] and 2.1 after 1 year [22]. Contrary results were published in two more prospective studies. The researchers reported on PTVs of − 1.4 after 6 months [21] or − 4.2 after 3 years [20]. Exact descriptions of the measurement procedure in the studies mentioned above are lacking. In an animal study, another SmartPeg prototype was developed for the same MI system used in the present study [42]. The MIs were inserted into the tibia/femur of rabbits. The median ISQs were 53.3 at insertion and 60.5 after 6 months. The higher values could be explained by the better bone quality in rabbit limbs and the more stable anchorage mechanism of the SmartPeg embracing the MI insertion square. In a randomized clinical trial, the researchers compared two immediate loaded two-piece implants with a diameter of 3 mm referred to as MI with two immediate loaded conventional implants (diameter 3,75 mm) to retain 30 free-end RPDs in mandibular Kennedy Class I dentitions [29]. They found identical 1-year survival rates of 93.3% and similar mean ISQ (70 versus 77.6, respectively). However, 3 mm diameter implants should be rather assigned to diameter-reduced or narrow conventional implants [13, 14].
The possible association between implant diameter and their stability was confirmed by our explorative evaluations of PTVs by MI diameter. The analyses were separated to jaw levels because of the possible differences in the bone quality between the maxilla and the mandible [18, 35]. Since 2.4 mm MIs were mainly inserted in the maxilla and the 2.1/1.8 mm MIs were mainly used in the mandible, the results would be otherwise biased. The difference of 0.3 and 0.6 mm and the differences in the screw threads design between the highest and the other MI diameters were most likely the reasons for the higher PTVs of the thinner MIs. This assumption is supported by a study comparing the PTVs of two other one-piece MI systems [22]. After 1 year, the MIs with diameters of 2.1 and 2.4 mm had a higher mean PTV (+ 2) than MIs with a diameter of 2.8 mm (− 1.6).
An expected trend of more MI failures in the immediate loading group A than in the delayed loading group B (8 versus 5 failures or 8% versus 5% 3-year failure rate) was not statistically verifiable. It should be noted that one MI in group A was removed before loading because of its malposition. Immediate loading of conventional implants with mandibular overdentures are poorly documented and result in more implant failures than delayed loading, whereas comparable data for the maxilla are missing [43]. In the only randomized 3-year comparison in 4-MI mandibular overdenture, immediate loading with housings had a lower MI survival rate than the delayed loading group (91.7% versus 96.7%, respectively) [44]. In the latter group, the MIs remained unloaded for 2 weeks, and thereafter, the overdentures were soft relined similar to our study. After 3 months, the housings were picked up.
The present MI survival rate of 99% in the mandible corresponds with results from strategic conventional implants (93–100%) [10, 11] and with the survival rate of MIs stabilizing complete mandibular dentures (92–100%) [12,13,14]. In a study, each two MIs with diameters of 2.0 or 2.5 mm were placed to retain 38 mandibular free-end RPDs. Before loading two MIs were lost, and the patients were excluded. This was classified as surgical survival rate of 97.4%. All loaded MIs survived at least 6 months [28].
Despite soft relining of RPDs in the case of insertion torque < 35 Ncm in group A and the no-load osseointegration in group B, eleven maxillary MIs were lost, and the survival rate probability was only 87% including the misplaced MI. All were multiple losses occurring in four patients and could be caused by the following reasons. First, two of the participants wore double crown-retained RPDs with multiple abutments in the mandible, and two participants had a natural mandibular dentition. A high occlusal load from the opposing jaw is a suspected cause of MI failures for some researchers [27, 29]. One participant with two MI losses was a heavy smoker. Smoking is a proven risk factor for implant complications [33]. The main reason for the high maxillary failure rate is probably the poorer bone quality with more trabecular and lesser cortical bone than in the mandible [19, 35, 45]. Last of all, one MI loss may cause further losses by compounding overload to the remaining abutments, similar to a domino effect.
A comparable failure rate of 82.3% in a 2-year prospective cohort study was reported. The study sample size was 31 patients with edentulous maxillae, each received 6 MIs. All overdentures were soft relined for 6 months before the housings were picked-up [26]. There were 32 failures in 16 patients, among them one patient with 5 and another with 6 failures. One patient was a heavy smoker with natural teeth in the mandible, and the other was a non-smoker with a mandibular implant overdenture. Seventeen MIs in ten patients were replaced, contrary to our trial in which some of the patients received MIs after the 3-year period. Other researchers reported unacceptable failure rates between 20 and 45% and sometimes clustered failures within one patient if all maxillary MIs under overdentures were immediately loaded with matrices [40, 41]. Overloading results in micro-movements of > 150 Ncm that can hinder secondary osseointegration [18].
Indeed, the predictive value of longitudinal RFA or Periotest measurements for implant failures is feasible, but the evidence is still weak and lacking for MIs [19, 34]. In the present study, the crude PTVs in eight of twelve lost MIs noticeably increased compared to the baseline values after 2 weeks, and the PTVs in six MIs were at least 20 just before the failure. The Cox regression analyses confirmed the suspected association with a 1.2- to 2.8-fold failure risk for a difference of 1–5 PTV units. According to systematic literature reviews, some but not all researchers found a relationship between falling RFA or increasing PTVs and conventional implants failure. However, single readings using any of the measurement techniques are of limited clinical relevance [19, 34].
Conclusions
Measured stability of MIs as supplementary abutments under existing RPDs is lower than of conventional implants without any relevant differences between immediate and delayed loading. There was a strong negative correlation between RFA values and PTVs, whereas the correlation between insertion torque and both measures of the primary stability was rather weak to moderate. MIs of 2.4 mm diameter showed lower PTVs than those of 1.8 to 2.1 mm diameter. The differences in the survival rates between the loading groups were slight (immediate loading: 95% and delayed loading: 92%, respectively). However, the MI survival rate in the maxilla was lower than in the mandible (87% versus 99%, respectively) with clustered observations in the maxilla (11 losses in 4 participants). Increasing PTVs can predict failing MIs. More studies are required to verify the present explorative analyses.
Data availability
Data are available on request from the corresponding author.
References
Rammelsberg P, Bernhart G, Lorenzo Bermejo J, Schmitter M, Schwarz S (2014) Prognosis of implants and abutment teeth under combined tooth-implant-supported and solely implant-supported double-crown-retained removable dental prostheses. Clin Oral Implants Res 25:813–818. https://doi.org/10.1111/clr.12197
Rinke S, Ziebolz D, Ratka-Kruger P, Frisch E (2015) Clinical outcome of double crown-retained mandibular removable dentures supported by a combination of residual teeth and strategic implants. J Prosthodont 24:358–365. https://doi.org/10.1111/jopr.12214
Wolfart S, Wolf K, Brunzel S, Wolfart M, Caliebe A, Kern M (2016) Implant placement under existing removable dental prostheses and its effect on masticatory performance. Clin Oral Investig 20:2447–2455. https://doi.org/10.1007/s00784-016-1746-y
Marotti J, Gatzweiler B, Wolfart M, Sasse M, Kern M, Wolfart S (2019) Implant placement under existing removable dental prostheses and the effect on follow-up and prosthetic maintenance. J Prosthodont 28:e752–e763. https://doi.org/10.1111/jopr.12943
Wolfart S, Moll D, Hilgers RD, Wolfart M, Kern M (2013) Implant placement under existing removable dental prostheses and its effect on oral health-related quality of life. Clin Oral Implants Res 24:1354–1359. https://doi.org/10.1111/clr.12030
Campos CH, Goncalves TM, Rodrigues Garcia RC (2014) Implant retainers for free-end removable partial dentures affect mastication and nutrient intake. Clin Oral Implants Res 25:957–961. https://doi.org/10.1111/clr.12165
de Freitas RF, de Carvalho DK, da Fonte Porto Carreiro A, Barbosa GA, Ferreira MA, (2012) Mandibular implant-supported removable partial denture with distal extension: a systematic review. J Oral Rehabil 39:791–798. https://doi.org/10.1111/j.1365-2842.2012.02326.x
Zancope K, Abrao GM, Karam FK, Neves FD (2015) Placement of a distal implant to convert a mandibular removable Kennedy class I to an implant-supported partial removable Class III dental prosthesis: a systematic review. J Prosthet Dent 113(528–533):e523. https://doi.org/10.1016/j.prosdent.2014.12.011
Goncalves TM, Campos CH, Goncalves GM, de Moraes M, Rodrigues Garcia RC (2013) Mastication improvement after partial implant-supported prosthesis use. J Dent Res 92:189S-194S. https://doi.org/10.1177/0022034513508556
Bassetti RG, Bassetti MA, Kuttenberger J (2018) Implant-assisted removable partial denture prostheses: a critical review of selected literature. Int J Prosthodont 31:287–302. https://doi.org/10.11607/ijp.5227
Lian M, Zhao K, Feng Y, Yao Q (2018) Prognosis of combining remaining teeth and implants in double-crown-retained removable dental prostheses: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 33:281–297. https://doi.org/10.11607/jomi.5796
Park JH, Lee JY, Shin SW (2017) Treatment outcomes for mandibular mini-implant-retained overdentures: a systematic review. Int J Prosthodont 30:269–276. https://doi.org/10.11607/ijp.4929
Goiato MC, Sonego MV, Pellizzer EP, Gomes JML, da Silva EVF, Dos Santos DM (2018) Clinical outcome of removable prostheses supported by mini dental implants. A systematic review Acta Odontol Scand 76:628–637. https://doi.org/10.1080/00016357.2018.1499958
Lemos CA, Verri FR, Batista VE, Junior JF, Mello CC, Pellizzer EP (2017) Complete overdentures retained by mini implants: a systematic review. J Dent 57:4–13. https://doi.org/10.1016/j.jdent.2016.11.009
Mundt T, Schwahn C, Stark T, Biffar R (2015) Clinical response of edentulous people treated with mini dental implants in nine dental practices. Gerodontology 32:179–187. https://doi.org/10.1111/ger.12066
Ferrari Cagidiaco ECF, Parrini S, Doldo T, Nagni M, Nuti N, Ferrari M (2018) Functional implant prosthodontic score of a one-year prospective study on three different connections for single-implant restorations. J Osseointegr 10:130–135. https://doi.org/10.23805/JO.2018.10.04.04
Gherlone EF, Cappare P, Pasciuta R, Grusovin MG, Mancini N, Burioni R (2016) Evaluation of resistance against bacterial microleakage of a new conical implant-abutment connection versus conventional connections: an in vitro study. New Microbiol 39:49–56. https://www.ncbi.nlm.nih.gov/pubmed/26922985
Javed F, Romanos GE (2010) The role of primary stability for successful immediate loading of dental implants. A literature review J Dent 38:612–620. https://doi.org/10.1016/j.jdent.2010.05.013
Chen MH, Lyons KM, Tawse-Smith A, Ma S (2019) Clinical significance of the use of resonance frequency analysis in assessing implant stability: a systematic review. Int J Prosthodont 32:51–58. https://doi.org/10.11607/ijp.6048
Elsyad MA, Gebreel AA, Fouad MM, Elshoukouki AH (2011) The clinical and radiographic outcome of immediately loaded mini implants supporting a mandibular overdenture. A 3-year prospective study. J Oral Rehabil 38:827–834. https://doi.org/10.1111/j.1365-2842.2011.02213.x
Temizel S, Heinemann F, Dirk C, Bourauel C, Hasan I (2017) Clinical and radiological investigations of mandibular overdentures supported by conventional or mini-dental implants: a 2-year prospective follow-up study. J Prosthet Dent 117(239–246):e232. https://doi.org/10.1016/j.prosdent.2016.07.022
Park JH, Shin SW, Lee JY (2018) Two-step immediate loading of mandibular overdentures retained by mini-implants: a prospective clinical study. Int J Prosthodont 31:446–450. https://doi.org/10.11607/ijp.5776
Scepanovic M, Todorovic A, Markovic A, Patrnogic V, Milicic B, Moufti AM et al (2015) Immediately loaded mini dental implants as overdenture retainers: 1-Year cohort study of implant stability and peri-implant marginal bone level. Ann Anat 199:85–91. https://doi.org/10.1016/j.aanat.2013.12.005
Jawad S, Clarke PT (2019) Survival of mini dental implants used to retain mandibular complete overdentures: systematic review. Int J Oral Maxillofac Implants 34:343–356. https://doi.org/10.11607/jomi.6991
Marcello-Machado RM, Faot F, Schuster AJ, Nascimento GG, Del Bel Cury AA (2018) Mini-implants and narrow diameter implants as mandibular overdenture retainers: a systematic review and meta-analysis of clinical and radiographic outcomes. J Oral Rehabil 45:161–183. https://doi.org/10.1111/joor.12585
Van Doorne L, De Kock L, De Moor A, Shtino R, Bronkhorst E, Meijer G et al (2020) Flaplessly placed 2.4-mm mini-implants for maxillary overdentures: a prospective multicentre clinical cohort study. Int J Oral Maxillofac Surg 49:384–391. https://doi.org/10.1016/j.ijom.2019.08.015
Schwindling FS, Schwindling FP (2016) Mini dental implants retaining mandibular overdentures: a dental practice-based retrospective analysis. J Prosthodont Res 60:193–198. https://doi.org/10.1016/j.jpor.2015.12.005
Disha V, Celebic A, Rener-Sitar K, Kovacic I, Filipovic-Zore I, Persic S (2018) Mini dental implant-retained removable partial dentures: treatment effect size and 6-months follow-up. Acta Stomatol Croat 52:184–192. https://doi.org/10.15644/asc52/3/2
Threeburuth W, Aunmeungtong W, Khongkhunthian P (2018) Comparison of immediate-load mini dental implants and conventional-size dental implants to retain mandibular Kennedy class I removable partial dentures: a randomized clinical trial. Clin Implant Dent Relat Res 20:785–792. https://doi.org/10.1111/cid.12646
Mundt T, Al Jaghsi A, Schwahn B, Hilgert J, Lucas C, Biffar R et al (2016) Immediate versus delayed loading of strategic mini dental implants for the stabilization of partial removable dental prostheses: a patient cluster randomized, parallel-group 3-year trial. BMC Oral Health 17:30. https://doi.org/10.1186/s12903-016-0259-z
Mundt T, Schwahn C, Heinemann F, Schimmel M, Lucas C, Al Jaghsi A (2020) Stabilizing removable partial dentures by immediate or delayed loading of mini-implants: chewing efficiency in a randomized controlled clinical trial. Int J Oral Maxillofac Implants 35:178–186. https://doi.org/10.11607/jomi.7707
Al Jaghsi A, Heinemann F, Biffar R, Mundt T (2021) Immediate versus delayed loading of strategic mini-implants under existing removable partial dentures: patient satisfaction in a multi-center randomized clinical trial. Clin Oral Investig 25:255–264. https://doi.org/10.1007/s00784-020-03360-y
Chuang SK, Wei LJ, Douglass CW, Dodson TB (2002) Risk factors for dental implant failure: a strategy for the analysis of clustered failure-time observations. J Dent Res 81:572–577. https://doi.org/10.1177/154405910208100814
Aparicio C, Lang NP, Rangert B (2006) Validity and clinical significance of biomechanical testing of implant/bone interface. Clin Oral Implants Res 17(Suppl 2):2–7. https://doi.org/10.1111/j.1600-0501.2006.01365.x
Oh JS, Kim SG (2012) Clinical study of the relationship between implant stability measurements using Periotest and Osstell mentor and bone quality assessment. Oral Surg Oral Med Oral Pathol Oral Radiol 113:e35-40. https://doi.org/10.1016/j.tripleo.2011.07.003
Gelman A, Hill J (2006). Data analysis using regression and multilevel/hierarchical models: Cambridge university press.
Senn S (2013) Seven myths of randomisation in clinical trials. Stat Med 32:1439–1450. https://doi.org/10.1002/sim.5713
Greenland S (2008) Introduction to regression models. Modern epidemiology 381–417.
Wasserstein RL, Lazar NA (2016) The ASA Statement on p-values: context, process, and purpose. Am Stat 70:129–133. https://doi.org/10.1080/00031305.2016.1154108
Elsyad MA, Ghoneem NE, El-Sharkawy H (2013) Marginal bone loss around unsplinted mini-implants supporting maxillary overdentures: a preliminary comparative study between partial and full palatal coverage. Quintessence Int 44:45–52. https://doi.org/10.3290/j.qi.a28746
Preoteasa E, Imre M, Preoteasa CT (2014) A 3-year follow-up study of overdentures retained by mini-dental implants. Int J Oral Maxillofac Implants 29:1170–1176. https://doi.org/10.11607/jomi.3222
Dhaliwal JS, Albuquerque RF Jr, Fakhry A, Kaur S, Feine JS (2017) Customized SmartPeg for measurement of resonance frequency of mini dental implants. Int J Implant Dent 3:4. https://doi.org/10.1186/s40729-017-0066-6
Schimmel M, Srinivasan M, Herrmann FR, Muller F (2014) Loading protocols for implant-supported overdentures in the edentulous jaw: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 29 Suppl:271–286. https://doi.org/10.11607/jomi.2014suppl.g4.4
Maryod WH, Ali SM, Shawky AF (2014) Immediate versus early loading of mini-implants supporting mandibular overdentures: a preliminary 3-year clinical outcome report. Int J Prosthodont 27:553–560. https://doi.org/10.11607/ijp.3845
Fuh LJ, Huang HL, Chen CS, Fu KL, Shen YW, Tu MG et al (2010) Variations in bone density at dental implant sites in different regions of the jawbone. J Oral Rehabil 37:346–351. https://doi.org/10.1111/j.1365-2842.2010.02061.x
Acknowledgements
We thank Dr. Bernd Schwahn, Greifswald, and Dr. Janine Hilgert, Drensteinfurt, who treated study participants and provided their dental offices for the data collection.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was financially supported by the 3 M Deutschland GmbH, Germany. The company did not participate in the study design; data assessment and analysis; the decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
T.M., F.H., C.S., and A.A. had substantial contributions to the conception and design of the work and to the interpretation of data. T.M., F.H., and A.A. acquired the data. J.M. and C.S. controlled the data and checked their plausibility. C.S. provided the statistical analyses. T.M. and J.M. drafted the manuscript. F.H., C.S., and A.A. revised the paper critically. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study design was approved by the Ethics Committee of the Greifswald University (BB 058/13A).
Consent to participate and to publish
Informed consent was obtained from all individual participants included in the study. The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1 and 2.
Competing interests
T.M. and F.H. use the implant system and receive fees for lectures and further training on mini-implants, including the implant manufacturer. There are no conflicts of interest for the co-authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mundt, T., Heinemann, F., Müller, J. et al. Survival and stability of strategic mini-implants with immediate or delayed loading under removable partial dentures: a 3-year randomized controlled clinical trial. Clin Oral Invest 27, 1767–1779 (2023). https://doi.org/10.1007/s00784-022-04805-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04805-2