Abstract
Objectives
To evaluate t he long-term outcomes following treatment of RT 1 multiple adjacent gingival recessions (MAGR) using the modified coronally advanced tunnel (MCAT) with either a collagen matrix CM or a connective tissue graft (CTG).
Material and methods
Sixteen of the original 22 subjects included in a randomized, controlled split-mouth clinical trial were available for the 9-year follow-up (114 sites). Recessions were randomly treated by means of MCAT + CM (test) or MCAT + CTG (control). Complete root coverage (CRC), mean root coverage (MRC), gingival recession depth (GRD), probing pocket depth (PD), keratinized tissue width (KTW), and thickness (KGT) were compared with baseline values and with the 12-month results.
Results
After 9 years, CRC was observed in 2 patients, one in each group. At 9 years, MRC was 23.0 ± 44.5% in the test and 39.7 ± 35.1% in the control group (p = 0.179). The MRC reduction compared to 12 months was − 50.1 ± 47.0% and − 48.3 ± 37.7%, respectively. The upper jaw obtained 31.92 ± 43.0% of MRC for the test and 51.1 ± 27.8% for the control group (p = 0.111) compared to the lower jaw with 8.3 ± 46.9% and 20.7 ± 40.3%. KTW and KGT increased for both CM and CTG together from 2.0 ± 0.7 to 3.1 ± 1.0 mm (< 0.0001). There were no statistically significant changes in PD.
Conclusion
The present results indicate that (a) treatment of MAGR using MCAT in conjunction with either CM or CTG is likely to show a relapse over a period of 9 years, and (b) the outcomes obtained in maxillary areas seem to be more stable compared to the mandibular ones.
Clinical relevance
The mean root coverage at 12 months could not be fully maintained over 9 years. On a long-term basis, the results seem to be less stable in the mandible as compared to maxillary areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gingival recession (GR) is defined as the apical shift of the gingival margin with respect to the cemento-enamel junction (CEJ), associated with attachment loss and exposure of the root surface to the oral environment [1, 2]. GR is commonly observed, especially among young and middle-aged adults [3]. Besides aesthetic complaints, GR may also cause root hypersensitivity, risk for development of caries or non-carious cervical lesions, and difficulties to achieve optimal plaque control [4].
While most of the existing literature reports on the treatment of single gingival recessions [5, 6], frequently, root exposures affect multiple adjacent teeth and are considered a generalized condition [7, 8]. The treatment of multiple adjacent gingival recessions (MAGR) poses a challenge for the clinician while data is still scarce on these procedures [9]. In the last two decades, the modified coronally advanced flap (MCAF) has become one of the most popular techniques for the treatment of MAGR [10]. Another surgical approach which has provided successful outcomes in the treatment of MAGR is the modified coronally advanced tunnel (MCAT) consisting of a preparation without raising a mucosal or mucoperiosteal flap and keeping the papillae intact. Several studies have recently evaluated the treatment of single and multiple recessions with MCAT demonstrating comparable improvements to those following the use of MCAF [11,12,13,14].
MCAT with the absence of releasing incisions delivers aesthetic outcomes; other benefits are favorable wound healing, minimal postoperative morbidity, and optimal blood supply and graft nutrition [15].
Palatal connective tissue graft (CTG) is still the gold standard among the soft tissue grafts used for various soft tissue augmentation procedures, although limitations in the size, shape, and thickness homogeneity may be present [7]. However, CTG harvesting may be associated with prolonged surgical time, increased patient morbidity, and the possibility of postoperative complications. To overcome these inconveniences, there has been a strong demand to find an alternative soft tissue grafting material [16]. The use of a porcine xenogeneic collagen matrix (CM; Mucograft, Geistlich, Wolhusen, Switzerland) in recession coverage was first evaluated in a histological study in minipigs. CM can serve as a scaffold for cells to enhance blood clot stability and conduce the ingrowth of blood vessels. Allergic reactions and material exfoliations were not reported during the application of this CM for recession coverage [17]. Clinically, a case report [18] as well as randomized controlled clinical studies compared the treatment of Miller class I and II single [19] and later multiple recessions [15, 20]. Several articles have compared sites treated by gingival augmentation to untreated sites in long-term studies with 18–35-year follow-up. The long-term observations support the importance of attached gingiva in preventing recession development due to prolonged mechanical trauma, bacterial inflammation, and iatrogenic factors during aging [1, 21]. A study with a long-term follow-up showed that sites treated with autologous soft tissue graft transplantation showed coronal displacement of the gingival margin with recession reduction, whereas recessions at contralateral untreated sites increased, or new recessions were developed during an 18- to 35-year follow-up [21].
Despite the fact that CM was proven to be a realistic alternative to CTG on the short term (i.e., after a period of 12 months), long-term results are still missing in the literature.
Therefore, the aim of the present study was to evaluate the long-term outcomes (i.e., after a period of 9 years) following treatment of class 1 (previously Miller class I and II) MAGR by means of the MCAT and either CM or CTG.
Materials and methods
The CONSORT statement for improving the quality of reports of parallel RCT (http://www.consort-statement.org/) was followed in the preparation of this study.
Study design and patient demographics
This is a 9-year follow-up of a previously published randomized split-mouth study [15], involving twenty-two patients with a total of 156 sites of class 1 (previously Miller I and II) MAGR [22, 23]. The original study was conducted between July 2010 and November 2011 at the Department of Periodontology of the Semmelweis University, Budapest, Hungary, in accordance with the Helsinki Declaration of 1975, as revised in 2013. The study protocol was approved by the ethical committee of the Semmelweis University (protocol: 5242–0/2010-101SEKU; 365/PI/10). The detailed protocol of the study along with the outcomes obtained at 1 year has been published before [15]. Thus, in the following, only a summary of the study design and patient demographics is presented.
To detect a true difference for the primary outcome of 20% assuming a power of 80%, the sample size calculation requested a minimal sample size of 18 patients. A total of 22 patients were finally included.
Inclusion criteria
The inclusion criteria are the following: 18 years old or older, systemically healthy subjects with at least 3 adjacent Miller I and II recessions on both sides. Full-Mouth Plaque Score (FMPS) had to be under 25%.
Exclusion criteria
The exclusion criteria are the following: pregnancy or lactation, tobacco smoking, uncontrolled medical conditions, medications that can affect gingival conditions, infectious diseases, non-cooperative patients, failure to sign informed consent.
Surgical approach
All the 22 patients underwent full-mouth supragingival scaling and polishing; then, individualized oral hygiene instructions were given preoperatively. The modified coronally advanced tunnel technique (MCAT) was applied in all cases in conjunction with either CM or CTG in a randomized split-mouth design. The random allocation of groups was generated using a computer program. Thus, every patient had one side of the jaw treated by means of MCAT technique with a bioresorbable collagen matrix (Mucograft®, Geistlich, Wolhusen, Switzerland) as a test. The other side of the jaw was treated with CTG, which was harvested from the palate and this site was considered control. Both surgeries were performed by the same experienced surgeon (SA) in one session. The surgical technique was described in detail in a previous article [18]. In brief, resin bonding at the contact points of the adjacent teeth was performed immediately before the surgery for suspended suturing. Under local anesthesia, the exposed root surfaces were gently planed by hand instruments (Gracey Curettes, Hu-Friedy). The preparation of MCAT started with an intrasulcular incision around involved teeth using microsurgical tunneling knives (Stoma). Mucoperiosteal flaps were elevated first as an envelope flap subsequently interconnected in a tunnel preparation. Flap preparation was extended beyond the mucogingival junction in split thickness and lastly, interdental papillae were gently undermined to allow tension-free, passive mobilization to the coronal aspect. After tunnel preparation, the grafting procedure was carried out according to the randomization code. The collagen matrix was trimmed and adapted to the required length and size. A CTG was harvested from the palate by the single incision technique [24] or a modified distal wedge procedure [25]. To close the donor site, either cross-mattress sutures or modified mattress sutures were placed. The insertion of both grafts to the subperiosteal tunnel was started in the widest recession using horizontal mattress sutures at mesial and distal aspect of the grafts. Finally, suspended sutures were placed above the approximal composite stops, and the tunneled flap was positioned 1 mm coronally to the cemento-enamel junction (CEJ).
Post-surgical treatment
Patients were prescribed analgesics for 3 days (3 × 50 mg diclofenac, Cataflam, Novartis) and antibiotics (3 × 625 mg amoxicillin and clavulanic acid, Augmentin, GlaxoSmithKline) for 7 days for infection prophylaxis. In addition, patients were advised to rinse with a 0.2% chlorhexidine solution (2 × per day for 3 weeks) and to discontinue tooth brushing at the surgical sites until the suture removal (2 weeks). The composite stops at the contact points were removed after 3 weeks. Recall appointments were scheduled every 3 months in the first 1 year and every 6 months thereafter.
Measurements
Clinical assessments were performed at baseline, at 1 month, 3 months, 6 months, 12 months and 9 years after the surgery by the same masked investigator (BM). Assessed parameters were as follows: recession depth (RD), recession width [11], keratinized gingiva width (KGW) in the mid-buccal aspect, papilla-contact point distance (PCD), papilla width (PW), probing depth on 3 surfaces (PD). Keratinized tissue thickness (KT) was only measured at baseline, 6 months, 12 months, and 9 years via sterile K-files following local anesthesia at 3-mm apical distance from the gingival margin. A UNC 15 type periodontal probe was used for measurements (Hu-Friedy, Chicago, IL, USA) The examiner was calibrated as discussed in original article. During surgery, the length of the procedure was measured in minutes.
Statistical analysis was performed using commercially available software (Instats 2000, version 3.05, GraphPad Prism 9.0.0. Software Inc., San Diego, CA, USA). A patient-level analysis was performed for each parameter. Therefore, mean values and standard deviations [26] for the clinical variables were calculated for each patient per treatment. The primary outcome variable was complete root coverage (CRC); secondary outcomes were MRC, amount of KTT, KTW, GRD, PW, and PD, respectively.
Statistical analysis
For each clinical parameter, a patient-level analysis was performed; i.e., mean values and standard deviations were calculated for each outcome and patient, respectively. Due to the non-parametric distribution of the data, between-group comparisons including Bonferroni corrections were conducted using the Mann–Whitney U test for independent unpaired variables, the Wilcoxon signed rank test for paired, and the Friedman test for dependent variables. Significance was set at p < 0.05.
Results
Original study with 12-month results
Detailed demographics and description of the original study sample were reported in the original publication [15].
Data in the original article represented split mouth data of 22 patients with 156 recessions (78 treated with CTG and 78 with CM). Mean root coverage (MRC) was 71% on test and 90% on control sites at 12 months. Complete root coverage (CRC) of all treated teeth was achieved in 5 sides out of 22 in the test and in 13 sides out of 22 in the control, respectively. Three patients presented with CRC for all treated recessions. Mean KGW had increased from 2.1 ± 0.9 to 2.4 ± 0.7 mm on test sites and from 2.0 ± 0.7 to 2.7 ± 0.8 mm on the control sites. KGT had increased from 0.8 ± 0.3 to 0.95 ± 0.4 mm (test) and from 0.8 ± 0.4 to 1.3 ± 0.5 mm (control). PD had not changed.
Patients’ characteristics at 9-year follow-up
Sixteen out of 22 (72%) individuals were available for a 9-year recall with a total of 114 treated recessions (72 in the maxilla and 42 in the mandible). None of the patients had received restorations or lost any of the investigated teeth during the 9 years of follow-up (Table 1).
Clinical outcome after 9 years
MRC
Results are compiled in Table 2. Compared to 12 months, MRC decreased from 73.2 ± 21.0 to 23.0 ± 44.5% in the test and from 88.0 ± 20.9 to 39.7 ± 35.1% in the control among the 16 subjects who attended the 9-year follow-up. Differences in MRC between the groups were significant after 12 months (p = 0.021) but diminished after 9 years (p = 0.179). In the mandible, MRC decreased from 79.7 ± 18.9% at 12 months to 8.3 ± 46.9% at 9 years in the test group, and from 95.8 ± 6.6 to 20.7 ± 40.3% in the control group, respectively. In the maxilla, MRC decreased from 69.3 ± 22.2 to 31.9 ± 43.0% (test) and 83.4 ± 25.3 to 51.1 ± 27.8% (control). After 9 years, CRC was maintained on 32 teeth out of 114 treated recessions. There was one side in each group that reached CRC for all treated teeth of the quadrant.
Keratinized tissue gain compared to baseline
In terms of keratinized tissue volume gain (Table 3), KTW increased by 0.9 ± 1.1 mm for test and by 0.8 ± 1.0 mm for the control group (p = 0.7197) whereas KTT gained by 0.6 ± 0.3 mm in the test and 0.7 ± 0.3 mm in the control group (p = 0.8403). When splitting up the results for mandible and maxilla, in the mandible, the increase was 1.7 ± 0.26 mm for the test group and 1.3 ± 1.3 mm for the control group (p = 0.625) and in the maxilla 0.9 ± 1.3 mm and 0.47 ± 0.6 mm (p = 0.3047), respectively. Regarding KTT, in the mandible, the increase was 0.7 ± 0.3 mm and 0.7 ± 0.3 mm (p = 0.6562) for test and control. In the maxilla, KTT increased by 0.58 ± 0.4 mm for the test and 0.6 ± 0.28 mm for the control group (p > 0.9).
Keratinized tissue gain compared to 12 months
The average gain in KTW at 9 years was 0.6 ± 0.9 mm and 0.4 ± 0.6 mm for CM and CTG (p = 0.7168). KTT revealed an increase following both procedures of 0.5 ± 0.4 mm in the test and 0.2 ± 0.3 mm in the control with a significant difference between the groups (p = 0.0259).
In the mandible, KTW increased by 0.3 ± 0.7 mm in the test and 0.5 ± 0.6 mm in the control (p = 0.375). The corresponding values for the maxilla were 0.8 ± 1.0 mm for the test and 0.4 ± 0.6 mm for the control (p = 0.2969). In the mandible, KTT increased by 0.5 ± 0.3 mm in the test and 0.28 ± 0.3 mm in the control group (p = 0.0625). In the maxilla, for KTT, the increase from 12 months to 9 years were as follows: 0.47 ± 0.4 mm in the test, 0.17 ± 0.37 mm in the control group (p = 0.1992).
Measurements of papilla-contact point distance (PCD) and papilla width (PW)
PCD presented no differences between test and control for any timepoint whereas PW demonstrated a significant increase at 12 months compared to baseline for both groups. This difference was maintained over the 9 years (Table 3).
Pocket depth (PD)
No differences of pocket depths were found between the groups and timepoints.
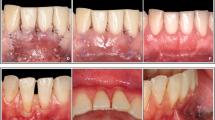
Clinical procedures and outcomes are represented in Fig. 1 and Fig. 2.
Discussion
The present study has evaluated the long-term outcomes following treatment of class 1 MAGR using the MCAT in conjunction with either CM or CTG. The results revealed that both graft materials may lead to positive aesthetic outcomes, which can be maintained over a period of 9 years. One important observation, however, is the statistically significantly lower MRC measured in the lower jaw, compared to the upper jaw in the group treated with CM. Interestingly, the increase of the KTT was similar in both groups; KTW showed only a slight difference favoring the CTG.
Most of the available literature compares different surgical techniques or reports on a single surgical technique alone and with one type of grafting material. There are only a few randomized, controlled clinical studies comparing the same surgical approach for the coverage of multiple gingival recessions using different grafting materials [15, 26,27,28].
The present study included multiple bilateral recessions both in the maxilla and mandible, also involving recession coverage at molars, which in turn may increase the risk of surgical difficulties and failures. Treatment of molars likely influenced the overall results because of the anatomical considerations: wide mesio-distal cervical contour, difficulties to access. Although recessions in the lateral zone may be of concern for patients with high lip lines or root hypersensitivity, they are still considered to be a major challenge for clinicians.
A recent systematic review has attempted to answer the question whether any 3D matrix biomaterial used for root coverage of localized class 1 defects may provide equivalent outcomes with CTG [29]. The results have shown that in terms of relative root coverage, no statistically significant differences were found among autogenous grafts, allografts, and xenogeneic materials. In terms of keratinized tissue width, on 2 mm recessions, CTG showed superiority above other biomaterials, but on 3 mm recessions, the results were the same. Interestingly, the percentage of recessions with CRC showed comparable results for all biomaterials.
McGuire et al. investigated the short- (up to 6 months) and the long-term outcomes (after 5 years) obtained with CM or CTG in conjunction with coronally advanced flap [30, 31] in single recessions. At 6 months, there were no statistically significant differences in terms of MRC (i.e., 97.5% for CTG and 89.5% for CM, respectively), while at 5 years the same values measured 95.5% for CTG and 77.6% for CM, respectively.
The results of the present long-term study are also in line with recent findings by Tonetti et al. [28], who have reported the 36-month follow-up of a trial comparing the adjunctive use of CM or CTG to CAF for the coverage of MAGR. At 3 years, the root coverage measured 1.5 ± 1.5 mm for CMX and 2.0 ± 1.0 mm for CTG (difference of 0.32 mm, 95% CI from − 0.02 to 0.65 mm) while the upper limit of the confidence interval was over the non-inferiority margin of 0.25 mm. Furthermore, no differences in the stability of root coverage were observed between groups over a period of 36 months. Taken together, the results suggested that CM was non-inferior to CTG for coverage of MAGR.
However, at present, to the best of our knowledge, there is no other long-term investigation which reports on data after a period of > than 5 years. In the present study, at 9 years, CRC was obtained in 2 out of the 16 patients. Interestingly, in both cases, the defects were located in the maxilla (i.e., one was treated with CM and the other one with CTG). Furthermore, in the lower jaw, only 4 out of the 42 sites showed CRC while the corresponding values for the upper jaw were 28 out of 72 sites. MRC amounted 23% in the test and 40% in the control group, respectively. The deterioration in terms of MRC and CRC measured in both the test and control group at 9 years as compared to the 12-month findings, may, on one hand, be explained by the increase in plaque levels or traumatic tooth brushing. On the other hand, it seems that the clinical outcomes are less stable in the mandibular area, compared to maxillary sites. This observation is in agreement with recent findings indicating that in cases of multiple mandibular adjacent gingival recessions, the treatment is frequently even more challenging due to difficulties related to the preparation of a tension-free flap or tunnel, stabilization of the graft and complete, and tension-free coverage of the graft and of the exposed root surfaces [32]. However, further research is needed in order to shed more light on the factors responsible for the differences in the outcomes between maxillary and mandibular recessions.
Conclusion
Within their limits, the present results indicate that (a) the results obtained in MAGR using MCAT in conjunction with either CM or CTG are likely to deteriorate over the course of 9 years, and (b) the outcomes obtained in maxillary areas seem to be more stable compared to the mandibular ones.
References
Pini PG (1999) Mucogingival deformities. Ann Periodontol 4(1):98–101
Cortellini P, Bissada NF (2018) Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol 89(Suppl 1):S204–S213
Sarfati A, Bourgeois D, Katsahian S, Mora F, Bouchard P (2010) Risk assessment for buccal gingival recession defects in an adult population. J Periodontol 81(10):1419–1425
Daprile G, Gatto MR, Checchi L (2007) The evolution of buccal gingival recessions in a student population: a 5-year follow-up. J Periodontol 78(4):611–614
Neves F, Augusto Silveira C, Mathias-Santamaria IF, Miguel MMV, Ferraz LFF, Casarin RCV et al (2020) Randomized clinical trial evaluating single maxillary gingival recession treatment with connective tissue graft and tunnel or trapezoidal flap: 2-year follow-up. J Periodontol 91:1018–1026
Sangiorgio JPM, Neves F, Rocha Dos Santos M, Franca-Grohmann IL, Casarin RCV, Casati MZ et al (2017) Xenogenous collagen matrix and/or enamel matrix derivative for treatment of localized gingival recessions: a randomized clinical trial. Part I: clinical outcomes. J Periodontol 88(12):1309–18
Tonetti MS, Cortellini P, Pellegrini G, Nieri M, Bonaccini D, Allegri M et al (2018) Xenogenic collagen matrix or autologous connective tissue graft as adjunct to coronally advanced flaps for coverage of multiple adjacent gingival recession: randomized trial assessing non-inferiority in root coverage and superiority in oral health-related quality of life. J Clin Periodontol 45(1):78–88
Zucchelli G (2000) Mounssif I (2015) Periodontal plastic surgery. Periodontol 68(1):333–68
Graziani F, Gennai S, Roldan S, Discepoli N, Buti J, Madianos P et al (2014) Efficacy of periodontal plastic procedures in the treatment of multiple gingival recessions. J Clin Periodontol 41(Suppl 15):S63-76
Zucchelli G, Mele M, Mazzotti C, Marzadori M, Montebugnoli L, De Sanctis M (2009) Coronally advanced flap with and without vertical releasing incisions for the treatment of multiple gingival recessions: a comparative controlled randomized clinical trial. J Periodontol 80(7):1083–1094
Cosgarea R, Kantarci A, Stavropoulos A, Arweiler N, Sculean A (2022) Soft tissue regeneration at natural teeth. Dent Clin North Am 66(1):87–101
Guldener K, Lanzrein C, Eliezer M, Katsaros C, Stahli A, Sculean A (2020) Treatment of single mandibular recessions with the modified coronally advanced tunnel or laterally closed tunnel, hyaluronic acid, and subepithelial connective tissue graft: a report of 12 cases. Quintessence Int 51(6):456–463
Lanzrein C, Guldener K, Imber JC, Katsaros C, Stahli A, Sculean A (2020) Treatment of multiple adjacent recessions with the modified coronally advanced tunnel or laterally closed tunnel in conjunction with cross-linked hyaluronic acid and subepithelial connective tissue graft: a report of 15 cases. Quintessence Int 51(9):710–719
Stähli A, Imber JC, Raptis E, Salvi GE, Eick S, Sculean A (2020) Effect of enamel matrix derivative on wound healing following gingival recession coverage using the modified coronally advanced tunnel and subepithelial connective tissue graft: a randomised, controlled, clinical study. Clin Oral Investig 24(2):1043–1051
Aroca S, Molnar B, Windisch P, Gera I, Salvi GE, Nikolidakis D et al (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. J Clin Periodontol 40(7):713–720
Mazzotti C, Stefanini M, Felice P, Bentivogli V, Mounssif I, Zucchelli G (2018) Soft-tissue dehiscence coverage at peri-implant sites. Periodontol 2000 77(1):256–72
Vignoletti F, Nunez J, Discepoli N, De Sanctis F, Caffesse R, Munoz F et al (2011) Clinical and histological healing of a new collagen matrix in combination with the coronally advanced flap for the treatment of Miller class-I recession defects: an experimental study in the minipig. J Clin Periodontol 38(9):847–855
Molnar B, Aroca S, Keglevich T, Gera I, Windisch P, Stavropoulos A et al (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with collagen matrix and the modified coronally advanced tunnel technique. Quintessence Int 44(1):17–24
Jepsen K, Jepsen S, Zucchelli G, Stefanini M, de Sanctis M, Baldini N et al (2013) Treatment of gingival recession defects with a coronally advanced flap and a xenogeneic collagen matrix: a multicenter randomized clinical trial. J Clin Periodontol 40(1):82–89
Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L (2014) Coronally advanced flap with and without a xenogenic collagen matrix in the treatment of multiple recessions: a randomized controlled clinical study. Int J Periodontics Restorative Dent 34(Suppl 3):s97-102
Agudio G, Chambrone L, Pini PG (2017) Biologic remodeling of periodontal dimensions of areas treated with gingival augmentation procedure: a 25-year follow-up observation. J Periodontol 88(7):634–642
Miller PD Jr (1985) A classification of marginal tissue recession. Int J Periodontics Restorative Dent 5(2):8–13
Cairo F, Nieri M, Cincinelli S, Mervelt J, Pagliaro U (2011) The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol 38(7):661–666
Hurzeler MB, Weng D (1999) A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent 19(3):279–287
Azzi R, Etienne D, Carranza F (1998) Surgical reconstruction of the interdental papilla. Int J Periodontics Restorative Dent 18(5):466–473
Cieslik-Wegemund M, Wierucka-Mlynarczyk B, Tanasiewicz M, Gilowski L (2016) Tunnel technique with collagen matrix compared with connective tissue graft for treatment of periodontal recession: a randomized clinical trial. J Periodontol 87(12):1436–1443
Pietruska M, Skurska A, Podlewski L, Milewski R, Pietruski J (2019) Clinical evaluation of Miller class I and II recessions treatment with the use of modified coronally advanced tunnel technique with either collagen matrix or subepithelial connective tissue graft: a randomized clinical study. J Clin Periodontol 46(1):86–95
Tonetti MS, Cortellini P, Bonaccini D, Deng K, Cairo F, Allegri M et al (2021) Autologous connective tissue graft or xenogenic collagen matrix with coronally advanced flaps for coverage of multiple adjacent gingival recession. 36-month follow-up of a randomized multicentre trial. J Clin Periodontol 48(7):962–9
De Carvalho FM, Nagasawa MA, Moraschini V, Ata-Ali J, Sculean A, Shibli JA (2020 Jul) Clinical efficacy of xenogeneic and allogeneic 3D matrix in the management of gingival recession: a systematic review and meta-analysis. Clin Oral Investig 24(7):2229–2245
McGuire MK, Scheyer ET (2010) Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 81(8):1108–1117
McGuire MK, Scheyer ET (2016) Long-term results comparing xenogeneic collagen matrix and autogenous connective tissue grafts with coronally advanced flaps for treatment of dehiscence-type recession defects. J Periodontol 87(3):221–227
Sculean A, Allen EP, Katsaros C, Stahli A, Miron RJ, Deppe H et al (2021) The combined laterally closed, coronally advanced tunnel for the treatment of mandibular multiple adjacent gingival recessions: surgical technique and a report of 11 cases. Quintessence Int 52(7):576–582
Funding
Open access funding provided by University of Bern
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Molnár, B., Aroca, S., Dobos, A. et al. Treatment of multiple adjacent RT 1 gingival recessions with the modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: 9-year results of a split-mouth randomized clinical trial. Clin Oral Invest 26, 7135–7142 (2022). https://doi.org/10.1007/s00784-022-04674-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04674-9