Abstract
Objectives
The gingival thickness (GT) and keratinized tissue (KT) height are defined as the gingival phenotype. Both the modified coronally advanced tunnel technique (MCAT) and free gingival grafts (FGG) are used in modifying the gingival phenotype. This study aims to compare MCAT and FGG in gingival phenotype modification.
Materials and methods
One hundred and forty recessions in 50 patients with thin and insufficient keratinized tissue at the anterior mandible were treated with either MCAT or FGG. GT, KT height, recession depth, recession width, probing depth, and clinical attachment level were evaluated at baseline and 6 weeks, 6 months, and 12 months. GT change, KT change, root coverage (RC), clinical attachment gain, and complete root coverage (CRC) were calculated. The wound healing index, tissue appearance, patient expectations, aesthetic, and dentin hypersensitivity were assessed at baseline and 6 months.
Results
All periodontal variables showed significant change from baseline to 12 months in both groups (p < 0.05). While FGG resulted in more KT change (p < 0.001), all MCAT sites showed at least 2 mm KT change in 12 months. MCAT resulted in greater GT change (p < 0.05) and RC (p < 0.003). In contrast, there was no significant inter-group CRC difference (p = 0.523). All patient-based variables were favorable to MCAT (p < 0.05), except dentin hypersensitivity (p = 0.225).
Conclusions
Both techniques were successful in terms of gingival phenotype modification in the anterior mandible. Additional GT increase, RC, and patient-based outcomes favored MCAT, though KT change proved greater with FGG.
Clinical relevance
Clinicians may choose MCAT for higher GT increase whereas FGG for more KTC.
Trial registration number: NCT04690140 and date: 12/26/2020.



Similar content being viewed by others
References
Jepsen S, Caton JG, Albandar JM, et al (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89https://doi.org/10.1002/JPER.17-0733
Hwang D, Wang H-L (2006) Flap thickness as a predictor of root coverage: a systematic review. Journal of Periodontology 77https://doi.org/10.1902/jop.2006.060107
John V, Langer L, Rasperini G, et al (2015) Periodontal soft tissue non–root coverage procedures: practical applications from the AAP Regeneration Workshop. Clinical Advances in Periodontics 5https://doi.org/10.1902/cap.2015.140051
Chambrone L, Tatakis DN (2016) Long-term outcomes of untreated buccal gingival recessions: a systematic review and meta-analysis. Journal of Periodontology 87https://doi.org/10.1902/jop.2016.150625
Ji JJ, Li XD, Fan Q, et al (2019) Prevalence of gingival recession after orthodontic treatment of infraversion and open bite. Journal of Orofacial Orthopedics 80https://doi.org/10.1007/s00056-018-0159-8
Ericsson I, Lindhe J (1984) Recession in sites with inadequate width of the keratinized gingival an experimental study in the dog. Journal of Clinical Periodontology 11https://doi.org/10.1111/j.1600-051X.1984.tb00837.x
Stetler KJ, Bissada NF (1987) Significance of the width of keratinized gingiva on the periodontal status of teeth with submarginal restorations. Journal of Periodontology 58https://doi.org/10.1902/jop.1987.58.10.696
Kennedy JE, Bird WC, Palcanis KG, Dorfman HS (1985) A longitudinal evaluation of varying widths of attached gingiva. Journal of Clinical Periodontology 12https://doi.org/10.1111/j.1600-051X.1985.tb00938.x
Barootchi S, Tavelli L, Zucchelli G, et al (2020) Gingival phenotype modification therapies on natural teeth: a network meta-analysis. Journal of Periodontology 91
Deeb JG, Deeb GR (2020) Oral soft tissue grafting. Oral and Maxillofacial Surgery Clinics of North America 32
Cevallos CAR, de Resende DRB, Damante CA, et al (2020) Free gingival graft and acellular dermal matrix for gingival augmentation: a 15-year clinical study. Clinical Oral Investigations 24https://doi.org/10.1007/s00784-019-02983-0
Paolantonio M (1997) Subpedicle connective tissue graft versus free gingival graft in the coverage of exposed root surfaces a 5-year clinical study. Journal of Clinical Periodontology 24https://doi.org/10.1111/j.1600-051x.1997.tb01184.x
Zuhr O, Bäumer D, Hürzeler M (2014) The addition of soft tissue replacement grafts in plastic periodontal and implant surgery: critical elements in design and execution. Journal of Clinical Periodontology 41
Zucchelli G, Marzadori M, Mounssif I, et al (2014) Coronally advanced flap + connective tissue graft techniques for the treatment of deep gingival recession in the lower incisors. A controlled randomized clinical trial. Journal of Clinical Periodontology 41.https://doi.org/10.1111/jcpe.12269
Pietruska M, Skurska A, Podlewski Ł, et al (2019) Clinical evaluation of Miller class I and II recessions treatment with the use of modified coronally advanced tunnel technique with either collagen matrix or subepithelial connective tissue graft: a randomized clinical study. Journal of Clinical Periodontology 46https://doi.org/10.1111/jcpe.13031
Chambrone L, Avila-Ortiz G (2021) An evidence-based system for the classification and clinical management of non-proximal gingival recession defects. Journal of Periodontology 92
Thoma DS, Buranawat B, Hämmerle CHF, et al (2014) Efficacy of soft tissue augmentation around dental implants and in partially edentulous areas: a systematic review. Journal of Clinical Periodontology 41
Windisch P, Molnar B (2019) Surgical management of gingival recession using autogenous soft tissue grafts. Clinical Dentistry Reviewed 3https://doi.org/10.1007/s41894-019-0058-4
Cairo F, Nieri M, Pagliaro U (2014) Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. Journal of Clinical Periodontology 41
Zucchelli G, Tavelli L, McGuire MK, et al (2020) Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. Journal of Periodontology 91
Cortellini P, Pini Prato G (2012) Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience. Periodontol 2000 59.https://doi.org/10.1111/j.1600-0757.2011.00434.x
Tatakis DN, Chambrone L, Allen EP, et al (2015) Periodontal soft tissue root coverage procedures: a consensus report from the AAP Regeneration Workshop. Journal of Periodontology 86https://doi.org/10.1902/jop.2015.140376
Aroca S, Molnár B, Windisch P, et al (2013) Treatment of multiple adjacent Miller class I and II gingival recessions with a modified coronally advanced tunnel (MCAT) technique and a collagen matrix or palatal connective tissue graft: a randomized, controlled clinical trial. Journal of Clinical Periodontology 40https://doi.org/10.1111/jcpe.12112
Azaripour A, Kissinger M, Farina VSL, et al (2016) Root coverage with connective tissue graft associated with coronally advanced flap or tunnel technique: a randomized, double-blind, mono-centre clinical trial. Journal of Clinical Periodontology 43https://doi.org/10.1111/jcpe.12627
Zuhr O, Fickl S, Wachtel H, et al (2007) Covering of gingival recessions with a modified microsurgical tunnel technique: case report. Int J Periodontics Restorative Dent 27:
Aichelmann-Reidy ME, Yukna RA, Evans GH, et al (2001) Clinical evaluation of acellular allograft dermis for the treatment of human gingival recession. Journal of Periodontology 72https://doi.org/10.1902/jop.2001.72.8.998
Kloukos D, Koukos G, Gkantidis N, et al (2021) Transgingival probing: a clinical gold standard for assessing gingival thickness. Quintessence International 52https://doi.org/10.3290/j.qi.b937015
Huang L-H, Neiva REF, Soehren SE, et al (2005) The effect of platelet-rich plasma on the coronally advanced flap root coverage procedure: a pilot human trial. Journal of Periodontology 76https://doi.org/10.1902/jop.2005.76.10.1768
Yates RJ, Newcombe RG, Addy M (2004) Dentine hypersensitivity: a randomised, double-blind placebo-controlled study of the efficacy of a fluoride-sensitive teeth mouthrinse. Journal of Clinical Periodontology 31https://doi.org/10.1111/j.1600-051X.2004.00581.x
Zucchelli G, Mele M, Stefanini M, et al (2010) Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialized grafts: a comparative randomized-controlled clinical trial. Journal of Clinical Periodontology 37https://doi.org/10.1111/j.1600-051X.2010.01550.x
Keceli HG, Sengun D, Berberoǧlu A, Karabulut E (2008) Use of platelet gel with connective tissue grafts for root coverage: a randomized-controlled trial. Journal of Clinical Periodontology 35https://doi.org/10.1111/j.1600-051X.2007.01181.x
Hatipoǧlu H, Keĉeli HG, Güncü GN, et al (2007) Vertical and horizontal dimensional evaluation of free gingival grafts in the anterior mandible: a case report series. Clinical Oral Investigations 11https://doi.org/10.1007/s00784-006-0084-x
Zucchelli G, Felice P, Mazzotti C, et al (2018) 5-year outcomes after coverage of soft tissue dehiscence around single implants: a prospective cohort study. European Journal of Oral Implantology 11:
Pini-Prato GP, Cairo F, Nieri M, et al (2010) Coronally advanced flap versus connective tissue graft in the treatment of multiple gingival recessions: a split-mouth study with a 5-year follow-up. Journal of Clinical Periodontology 37https://doi.org/10.1111/j.1600-051X.2010.01559.x
Agudio G, Nieri M, Rotundo R, et al (2009) Periodontal conditions of sites treated with gingival-augmentation surgery compared to untreated contralateral homologous sites: a 10- to 27-year long-term study. Journal of Periodontology 80https://doi.org/10.1902/jop.2009.090122
Lang NP, Löe H (1972) The relationship between the width of keratinized gingiva and gingival health. Journal of Periodontology 43https://doi.org/10.1902/jop.1972.43.10.623
McGuire MK, Scheyer ET, Nevins ML, et al (2011) Living cellular construct for increasing the width of keratinized gingiva: results from a randomized, within-patient, controlled trial. Journal of Periodontology 82https://doi.org/10.1902/jop.2011.100671
Allen EP (2021) Soft tissue grafting with the tunnel technique in the mandibular anterior: myths and realities. Journal of Esthetic and Restorative Dentistry 33https://doi.org/10.1111/jerd.12712
Prato GP, Clauser C, Cortellini P (1995) Periodontal plastic and mucogingival surgery. Periodontol 2000 9:.https://doi.org/10.1111/j.1600-0757.1995.tb00058.x
Agudio G, Nieri M, Rotundo R, et al (2008) Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. Journal of Periodontology 79https://doi.org/10.1902/jop.2008.070414
Cosgarea R, Miron R, Bora R, et al (2021) Long-term results after treatment of multiple adjacent gingival recessions with the modified coronally advanced tunnel and a porcine acellular dermal matrix. Quintessence International 52https://doi.org/10.3290/j.qi.a45171
Bhatavadekar N, Gharpure A, Chambrone L (2019) Long-term outcomes of coronally advanced tunnel flap (CATF) and the envelope flap (mCAF) plus subepithelial connective tissue graft (SCTG) in the treatment of multiple recession-type defects: a 6-year retrospective analysis. The International Journal of Periodontics & Restorative Dentistry 39 https://doi.org/10.11607/prd.4026
Guiha R, Khodeiry S el, Mota L, Caffesse R (2001) Histological evaluation of healing and revascularization of the subepithelial connective tissue graft. Journal of Periodontology 72https://doi.org/10.1902/jop.2001.72.4.470
Nobuto T, Tokioka T, limai H, et al (1987) Microvascularization of gingival wound healing using corrosion casts. Journal of Periodontology 58https://doi.org/10.1902/jop.1987.58.4.240
Zuhr O, Rebele SF, Schneider D, et al (2014) Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: a RCT using 3D digital measuring methods. Part I. Clinical and patient-centred outcomes. Journal of Clinical Periodontology 41:.https://doi.org/10.1111/jcpe.12178
Górski B, Górska R, Wysokińska-Miszczuk J, Kaczyński T (2020) Tunnel technique with enamel matrix derivative in addition to subepithelial connective tissue graft compared with connective tissue graft alone for the treatment of multiple gingival recessions: a randomized clinical trial. Clinical Oral Investigations 24https://doi.org/10.1007/s00784-020-03312-6
Bassetti RG, Stähli A, Bassetti MA, Sculean A (2016) Soft tissue augmentation procedures at second-stage surgery: a systematic review. Clinical Oral Investigations 20
Santamaria MP, Neves FL da S, Silveira CA, et al (2017) Connective tissue graft and tunnel or trapezoidal flap for the treatment of single maxillary gingival recessions: a randomized clinical trial. Journal of Clinical Periodontology 44https://doi.org/10.1111/jcpe.12714
Cairo F, Barootchi S, Tavelli L, et al (2020) Aesthetic-and patient-related outcomes following root coverage procedures: a systematic review and network meta-analysis. Journal of Clinical Periodontology 47
Tavelli L, Barootchi S, Majzoub J, et al (2021) Prevalence and risk indicators of midfacial peri-implant soft tissue dehiscence at single site in the esthetic zone: a cross-sectional clinical and ultrasonographic study. Journal of Periodontologyhttps://doi.org/10.1002/JPER.21-0402
Rojo E, Stroppa G, Sanz-Martin I, et al (2020) Soft tissue stability around dental implants after soft tissue grafting from the lateral palate or the tuberosity area – a randomized controlled clinical study. Journal of Clinical Periodontology 47https://doi.org/10.1111/jcpe.13292
Acknowledgements
The authors express their gratitude to Ege Nadir Aytac and Ayhan Parmaksiz for their significant contribution and support to the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The Hacettepe University Clinical Research Ethics Committee provided ethical approval for the project (02.05.2019, KA-19047). The trial (clinical trials no.: NCT04690140) was conducted in accordance with the principles of the Declaration of Helsinki (1975, revision Tokyo, 2004).
Informed consent
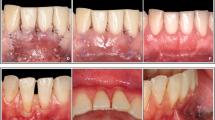
Informed consent was obtained from all individual participants included in the study. The authors affirm that human research participants provided informed consent for publication of the images in Fig. 1.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yilmaz, B.T., Comerdov, E., Kutuk, C. et al. Modified coronally advanced tunnel versus epithelialized free gingival graft technique in gingival phenotype modification: a comparative randomized controlled clinical trial. Clin Oral Invest 26, 6283–6293 (2022). https://doi.org/10.1007/s00784-022-04580-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04580-0