Abstract
Objectives
To compare the characteristics of mandibular asymmetry in patients with unilateral craniofacial microsomia (CFM) and class II asymmetry.
Materials and methods
Pretreatment cone-beam computed tomography of consecutive adults with Pruzansky-Kaban type I and IIA CFM (CFM group) was analyzed by 3D cephalometry. Fourteen mandibular landmarks and two dental landmarks were identified. The mandibular size and positional asymmetry were calculated by using landmark-based linear and volumetric measurements, in terms of asymmetry ratios (affected/non-affected side) and absolute differences (affected − non-affected side). Results were compared with non-syndromic class II with matched severity of chin deviation (Class II group). Statistical analyses included independent t test, paired t test, chi-square test, and ANOVA.
Results
CFM group (n, 21; mean age, 20.4 ± 2.5 years) showed significantly larger size asymmetry in regions of mandibular body, ramus, and condyle compared to Class II group (n, 21; mean age, 27.8 ± 5.9 years) (p < 0.05). The curvature of mandibular body was asymmetric in CFM. Regarding the positional asymmetry of mandibular body, while a comparable transverse shift and a negligible yaw rotation were found among the two groups, the roll rotation in CFM was significantly greater as well as the occlusal (6.06° vs. 4.17°) and mandibular (7.84° vs. 2.80°) plane cants (p < 0.05).
Conclusions
Mild CFM showed significantly more severe size asymmetry and roll rotation in mandible than non-CFM class II asymmetry.
Clinical relevance
To improve the mandibular size and positional asymmetry in CFM, adjunct hard tissue augmentation or reduction in addition to OGS orthodontics with a meticulous roll and yaw planning is compulsory, which is expected to be distinct from treating non-CFM class II asymmetry.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniofacial microsomia (CFM) features hypoplastic mandibular structures of the affected side and subsequently a significant facial asymmetry and class II malocclusion [1,2,3]. Mild CFM (Pruzansky-Kaban type I and IIA) shows mild to moderate mandibular hypoplasia with the presence of a functional temporomandibular joint [4, 5]. In type I and IIA CFM, the extents of the mandibular retrusion and chin deviation can be similar to those of non-syndromic patients with skeletal class II asymmetry. From this point of view, orthognathic surgery (OGS) has been recommended by many clinicians as the standard procedure to substantially treat the dysgnathia and maxillomandibular asymmetry in both groups [5,6,7,8,9,10].
On account of the aberrant mandibular hypoplasia and malposition, an ideal postsurgical result regarding restoring facial symmetry is often challenging to achieve in non-growing CFM [7, 10,11,12]. Previous studies revealed that OGS segment repositioning significantly improved the facial midline asymmetry and mandibular retrusion in CFM and non-syndromic class II patients with residual chin deviation of approximately 1 mm and 2.6 mm, respectively [10, 11, 13]. For non-syndromic class II patients, the contour asymmetry improved as well after the conventional OGS approach [13, 14]. However, for CFM patients, a more complex combination of surgical interventions (e.g., different osteotomy designs for affected and non-affected sides, autogenic or alloplastic grafts, patient-specific implant (PSI), bone shaving, myectomy) or a staged treatment protocol was usually proposed in order to obtain a satisfactory treatment outcome for facial contour symmetry [3, 9, 10]. No studies have systematically compared the mandibular morphology between the two groups. A thorough understanding of the similarities and differences in the mandibular shape (revealed by bilateral size differences) and malposition is essential to clarify the necessity of different treatment strategies among patients with mild CFM and asymmetric class II mandibular hypoplasia, and to optimize the treatment protocol for CFM.
The aim of this study was to compare the mandibular morphology affecting the facial asymmetry between subjects with mild CFM and non-syndromic skeletal class II asymmetry. The null hypothesis was that no difference existed in the mandibular characteristics between the two groups.
Materials and methods
Study population
Patients older than 16 years with unilateral CFM and skeletal class II asymmetry were enrolled in this retrospective study. CFM group (test group) consisted of consecutive patients who visited the Chang Gung Craniofacial Center between 2010 and 2018 for treatment by using the following inclusion criteria: (1) Pruzansky-Kaban type I or IIA CFM with a deviated chin toward the affected side, (2) availability of cone-beam computed tomography (CBCT) before the orthodontic or orthognathic treatment, (3) absence of craniofacial syndromes other than CFM, and (4) no history of maxillomandibular surgery or trauma. The subjects in Class II group (control group) were consecutively selected from non-syndromic skeletal class II (ANB angle > 4°) patients who visited the same center between 2010 and 2013 for treatment by matching the severity of chin deviation with that of CFM group. The same inclusion criteria were applied to Class II group.
Image acquisition and cephalometry
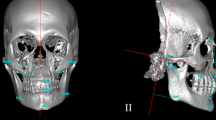
The head and neck of all subjects were scanned in the natural head position using an i-CAT 3D Dental Imaging System (Imaging Sciences International, Hatfield, PA, USA) with parameter settings of 120 kV, 0.4 mm voxel size, 40 s scan time, and 16 cm × 16 cm field of view. CBCT images were stored in the Digital Imaging and Communications in Medicine (DICOM) format and reconstructed to 3D head models using Maxilim® software (Medicim NV, Mechelen, Belgium). Additionally, all the condyle heads were carefully segmented, reconstructed, and integrated with the head models in Maxilim® [15]. The 3D head models were registered in a cephalometric reference frame based on the protocol of Swennen et al., using the landmarks orbitale and porion on the non-affected side, and further completed by the frontozygomatic points, nasion, and sella (Fig. 1) [16, 17]. The affected side was defined as the side to which the chin deviation was pointed to and where CFM was present.
The 3D cephalometric reference frame (a). A plane passing through sella and 6-degree below the sella-nasion plane was defined as the horizontal reference plane. A plane passing through sella and nasion and perpendicular to the horizontal reference plane was the midsagittal plane. A plane passing through sella and perpendicular to the horizontal and midsagittal planes was the coronal reference plane. Landmarks used for measurements of mandibular characteristics and facial asymmetry (b). Menton (Me), alveolar point at lower canine (AlvL3), alveolar point at lower first molar (AlvL6), mandibular lower border point at lower canine (LbL3), mandibular lower border point at lower first molar (LbL6), gonion (Go), anterior ramal point (Ant-Ra), posterior ramal point (Post-Ra), C-point (C), superior condylar point (Sup-Con), medial condylar point (Med-Con), lateral condylar point (Lat-Con), upper incisal embrasure (UIE), upper first molar (U6). Please refer to Table 1 for the definitions of landmarks
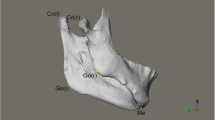
Multiple cephalometric landmarks and planes were used for measurements, which were identified on the 3D head model with the aid of multiplanar views (Tables 1 and 2, Figs. 1 and 2). A positive coordinate value indicated the anterior, inferior, and affected side. Teeth were removed at the level of the alveolar ridge from the 3D mandibular model before volumetric measurements were conducted (Fig. 2). To quantify the size asymmetry of mandible, asymmetry ratios of the mandibular measurements between bilateral sides were calculated (affected side/non-affected side). An asymmetry ratio of 1 indicated perfect symmetry in size. To determine the positional asymmetry of mandible, the difference in coordinates of the affected side minus the non-affected side was recorded.
Landmarks and planes used to define the different regions for volumetric measurements. The mandibular central plane was passing through IFD, GT, and Me. The C-plane was passing through the C-point and parallel to the horizontal reference plane. The posterior ramal point-gonion plane was passing through Post-Ra and Go and perpendicular to the mandibular central plane. The gonion-menton plane was passing through Me and Go and perpendicular to the mandibular central plane. The mandibular angle plane was the mid-angular plane between the posterior ramal point-gonion plane and gonion-menton plane. Please refer to Table 1 for the definitions of landmarks
The primary outcome variables were the occlusal plane cant, the mandibular plane cant, and the size and positional asymmetry of the mandible. The primary predictor variable was the type of mandibular asymmetry (CFM vs. class II asymmetry).
To assess the intra-investigator reliability, the CBCT segmentation and measurements were conducted by one investigator (YFC) for 10 randomly chosen patients twice, with an interval of two weeks. To assess the inter-investigator reliability, a second investigator (SV) independently conducted the same process for the same CBCT dataset.
Statistical analysis
To determine the sample size, the G-Power software (version 3.1.9.7; Franz Faul, University of Kiel, Kiel, Germany) was used. A minimum of 17 subjects per group was estimated based on our previous studies [17, 18] by setting an effect size of 1.0, a significance level of 5% (p < 0.05), and a power of 80%.
The Statistical Package for Social Sciences for Windows 24 (SPSS 24, IBM Corp., NY, USA) was used for statistical analyses. All descriptive statistics are presented as mean ± standard deviation. Demographical data of the two groups (CFM and Class II) were compared using an independent t test or chi-square test where indicated. The groups were matched by the severity of chin deviation. A paired t test was used to compare the difference of CBCT measurements between the affected and non-affected sides. A repeated measures ANOVA with the Bonferroni post hoc test was used to detect significant differences in the CBCT measurements between three locations along the lower border of the mandibular body. Intra-class correlation (absolute, two-way mixed) was calculated to assess the intra- and inter-observer reliability. All statistical tests were two sided, and p < 0.05 considered statistically significant.
Results
Subject characteristics
Based on the inclusion and exclusion criteria, 21 subjects with unilateral CFM (14 females and 7 males; mean age, 20.4 ± 2.5 years; age range, 17.3–27.0 years) and 21 subjects with non-syndromic class II asymmetry (14 females and 7 males; mean age, 27.8 ± 5.9 years; age range, 19.0–47.0 years) were enrolled. There was no difference in ANB (p = 0.580) and SNB (p = 0.265) between the groups. However, the SNA of CFM group was significantly lower than Class II group, 78.36° ± 4.32° vs. 82.02° ± 2.73°, respectively (p = 0.002) (Table 3).
Measurement reliability
Intra-observer reliability, analyzed by the intraclass correlation coefficient (ICC), was excellent (mean ICC, 0.999; 95%CI, 0.979–1.000). Inter-observer reliability was excellent (mean ICC, 0.999; 95%CI, 0.972–1.000).
Facial asymmetry
The occlusal plane cant (6.06° ± 3.36° vs. 4.17° ± 2.12°, p = 0.040) and mandibular plane cant (7.84° ± 4.10° vs. 2.80° ± 2.90°, p < 0.001) were significantly more severe in CFM group than in Class II group (Table 4).
Mandibular size asymmetry
In CFM group, all the mandibular parameters showed significant size asymmetry (all the values of mandibular size parameters on the affected side were significantly lower than those on the non-affected side). Additionally, the posterior mandibular body height was significantly more asymmetric than the anterior mandibular body height (AlvL6-LbL6 vs. AlvL3-LbL3 = 84.30 ± 12.38% vs. 91.47 ± 7.31%, p = 0.002). In Class II group, only gonial width, length, and volume of mandibular body, ramal height, and height and volume of condyle showed significant size asymmetry (Table 5).
Compared to Class II group, CFM group showed significantly more severe asymmetry (lower asymmetry ratio) for all the mandibular parameters except gonial width (Table 4).
Mandibular positional asymmetry
For both groups, LbL3 point, LbL6 point, and gonion on the affected side were significantly positioned laterally and superiorly compared to the non-affected side. For CFM group, gonion on the affected side was significantly positioned anteriorly compared to the non-affected side.
For both groups, Sup-Con point on the affected side was significantly positioned inferiorly compared to the non-affected side (Table 5).
The repeated measures ANOVA with Bonferroni correction showed that, in relation to the midsagittal plane, there were significant differences between the transverse positional asymmetry of LbL3 point, LbL6 point, and gonion for both groups (CFM, 11.60 ± 9.00 mm vs. 7.28 ± 7.32 mm vs. 2.36 ± 5.08 mm, p < 0.01; Class II, 13.94 ± 8.22 mm vs. 10.30 ± 6.96 mm vs. 5.51 ± 5.52 mm, p < 0.01), implying more severe side shifting toward the anterior mandible (Fig. 3).
Compared to non-syndromic class II asymmetry (right) with similar extents of chin deviation, skeletal class II discrepancy, and mandibular retrusion, mild CFM (Left) showed: a more severe canting of occlusal and mandibular planes; b additional maxillary retrusion, and greater height asymmetry in mandibular body, ramus, and condyle; and c more severe deficit at the lateral border along the mandibular body (asymmetric shape of body arc), and a sagittally hypoplastic mandibular angle on the CFM-affected side
Regarding transverse positional asymmetry at L3Lb point, L6Lb point, gonion, and Sup-Con point, there was no significant difference between the two groups. Regarding the sagittal positional asymmetry, only gonion showed a significant difference between the two groups (CFM vs. Class II = 4.38 ± 6.05 mm vs. − 1.44 ± 3.36 mm, p < 0.001). Regarding the vertical positional asymmetry, all the points of LbL3, LbL6, Go, Sup-Con showed significant difference between the two groups (p < 0.05) (Table 4).
Discussion
Clinically, patients with mild CFM (type I and IIA) display similar facial features as non-syndromic class II asymmetry: notable mandibular retrusion and chin deviation. Considering all mandibular regions of interest are present, the CFM-related dysgnathia could be treated by OGS without the need of TMJ reconstruction [7, 9, 10]. Although the commonly known soft tissue deficits in addition to the skeletal hypoplasia in CFM further complicate the facial asymmetry, it has been suggested that soft tissue correction should be conducted after skeletal tissue reconstruction [3, 9, 10]. Even achieving skeletal symmetry is a challenge due to the aberrant shape besides the malposition of the mandible. To the authors’ knowledge, this was the first study to compare the 3D mandibular characteristics between class II asymmetry patients with and without CFM in order to enhance the contemporary OGS treatment strategy and to understand the treatment limitations specifically for mild CFM patients.
The results of the study have rejected the null hypothesis, indicating the presence of a more severe mandibular size asymmetry and vertical positional asymmetry in CFM group than in Class II group, despite a comparable chin deviation.
Compared to non-syndromic class II subjects with similar extent of chin deviation, CFM is characterized by 4 features.
-
1.
CFM subjects displayed significantly more severe occlusal plane cant and mandibular plane cant, and consequently the face was perceived as more asymmetric. Moreover, the canting of the mandibular plane was larger than that of the occlusal plane in CFM group, while the opposite was found in Class II group (Fig. 3a).
-
2.
The mandible of CFM had significantly greater size asymmetry between the affected and non-affected sides, in terms of mandibular, ramal, and condylar heights (Fig. 3b). A remarkable asymmetry in mandibular body height was present particularly in CFM. By contrast, subjects with non-CFM class II asymmetry had relatively symmetric body height, which is accordant with the study of Kim et al. [19]. The reduced ramal height on the chin deviation side is a consistent finding in the literature regardless of the presence of CFM, age, the type of sagittal skeletal discrepancy (class II or III) [8, 20,21,22,23,24], and unsurprisingly, the hypoplastic nature in CFM exaggerated the height discrepancy. The gonial width ratio, on the other hand, was not different between the two groups, indicating similar inward bending of the mandibular angle on the affected side. In CFM group, the asymmetry ratios of width at points of LbL3, LbL6, and gonion were 77.80%, 67.28%, and 74.37%, respectively; in Class II group, 86.60%, 82.34%, and 78.96%. The differences in width asymmetry ratios along the mandibular body implied that the curvature of the mandibular body on the affected side in CFM group resembled a half-V shape (a lateral deficit over the mandibular body), whereas in Class II group, it looked more like a half-U shape (Fig. 3c).
-
3.
CFM group exhibited significant differences in the volume of the mandibular body, ramus, and condyle between the affected and non-affected sides, whereas in Class II group, only the mandibular and condylar volumes were different between the two sides, which were of less severity as well.
-
4.
CFM subjects had significant more maxillary retrusion compared to non-CFM class II asymmetry subjects (Fig. 3b).
Both groups showed a similar transverse shift of the mandible to the affected side without a remarkable yaw rotation. Anteriorly positioned gonion on the affected side was only found among the CFM subjects. This might be the result of unilateral mandibular hypoplasia rather than a yaw rotation of the mandible as there was no significant sagittal discrepancy for bilateral LbL3 and LbL6 points. Also, the significant correlation between the sagittal positional discrepancy of gonion and the length discrepancy of mandibular body in CFM (r = 0.508, p = 0.019) supported the hypoplastic nature of the mandibular body particularly in CFM.
The four distinctive features between mild CFM and class II asymmetry were the primary findings of the present study. Furthermore, they would also be the fundament to justify different approaches in OGS planning for the two groups of patients.
-
1.
A larger roll correction of the maxilla and mandible is required in mild CFM patients. Moreover, looking into the different patterns of canting in CFM group in contrast to Class II group, the mandibular lower border of the affected side in CFM would remain asymmetric (positioned more cranially) after the occlusal plane cant is surgically leveled (Table 4, Fig. 3). Presurgical orthodontics to decrease the discrepancy between occlusal and mandibular plane cants, or additional hard tissue interventions (reduction, or augmentation with bone graft or PSI) at the mandibular lower border could be considered [11, 12, 25].
-
2.
A shift movement of the maxillomandibular complex toward the non-affected side to center the midline structures will displace the mandibular angle of the non-affected side laterally and that of the affected side medially, deteriorating the posterior mandibular asymmetry, especially in CFM group as the pretreatment transverse positional asymmetry in gonion was less than Class II group (Table 4). A yaw adjustment of the maxillomandibular complex; grinding of the medial side and/or decortication of the lateral side of the proximal segment, or a lingual osteotomy of the distal segment on the non-affected side [26]; or intentional flaring of the proximal segment on the affected side could be considered to reduce the subsequent posterior mandibular asymmetry. The asymmetric mandibular body curvature, or the notable volume deficiency in the mandibular body and ramus on the affected side in CFM would demand further hard or soft tissue interventions (augmentation, reduction, botuline toxine injection, etc.). As the soft tissue envelope on the affected side in CFM is often reduced and compromised, reduction management on the non-affected side with the modest augmentation on the affected side might lead to a more stable outcome than sole augmentation management [10].
-
3.
The retroposition of the maxilla in CFM group would also require a larger maxillary advancement than in Class II group to provide more soft tissue support of the midface and upper lip.
The key in correcting asymmetry of the maxillomandibular complex is the transverse movement of the maxilla and mandible to align the dental and skeletal midlines with the facial midline. As the chin deviation was the same in CFM and Class II groups, a similar transverse movement of the jaws would be required. Promising midline alignment in CFM could be achieved (around only 1 mm of residual chin deviation) as reported in the literature [9, 11], yet the significant bilateral differences in CFM mandibles found in the present study underline the difficulty and the demand for more effort to improve the bilateral asymmetry (cant and contour) in CFM than in cases of non-CFM class II asymmetry.
There are limitations to this current study. First, only hard tissue asymmetry is evaluated in CFM and Class II groups. Soft tissue asymmetry, which also influences the facial appearance, is additionally a core issue in CFM and needs to be inspected in future studies. Moreover, the postsurgical effects of the treatment options described above should be assessed on the soft tissue and hard tissue levels with an adequate follow-up in a clinical comparative study. Lastly, Class II group was significantly older than CFM group. This can be attributed to the very low prevalence of skeletal class II combined with facial asymmetry that is as severe as that of CFM patients. Chew [27] showed a low prevalence of 1.89% for class II asymmetry among 212 orthognathic patients; thus, the prevalence of severe asymmetry can be expected to be lower. Besides, patients with class II asymmetry usually did not have regular visits to our center since their childhood in contrast to CFM patients, and a timely surgical intervention could not be arranged. On the other hand, Pearson’s correlation coefficients showed no significant correlation between age and the extents of facial and mandibular asymmetry in each group, suggesting that the impact of age on skeletal asymmetry might be limited for subjects older than 16 years.
Conclusions
Mild CFM patients showed more severe size asymmetry in the mandibular body, ramus, and condyle, and displayed a larger roll in the mandibular body compared to patients with non-syndromic skeletal class II asymmetry. Clinicians should be aware of the significant size asymmetry found at the lower (asymmetric body height), posterior (asymmetric angle prominence), and lateral (asymmetric body arc shape) borders of the mandibular body in the treatment of CFM.
References
Cousley RR, Calvert ML (1997) Current concepts in the understanding and management of hemifacial microsomia. Br J Plast Surg 50(7):536–551. https://doi.org/10.1016/s0007-1226(97)91303-5
Caron C, Pluijmers BI, Wolvius EB, Looman CWN, Bulstrode N, Evans RD, Ayliffe P, Mulliken JB, Dunaway D, Padwa B, Koudstaal MJ (2017) Craniofacial and extracraniofacial anomalies in craniofacial microsomia: a multicenter study of 755 patients. J Craniomaxillofac Surg 45(8):1302–1310. https://doi.org/10.1016/j.jcms.2017.06.001
Resnick C, Kaban L, Padwa B (2017) Hemifacial microsomia: the disorder and its surgical management. In: Brennan PA, Schliephake H, Ghali GE, Cascarini L (eds) Maxillofacial Surgery, 3rd edn. Churchill Livingstone, pp 870–893. https://doi.org/10.1016/B978-0-7020-6056-4.00063-0
Kaban LB, Moses MH, Mulliken JB (1988) Surgical correction of hemifacial microsomia in the growing child. Plast Reconstr Surg 82(1):9–19
Posnick JC (2014) Hemifacial microsomia: evaluation and treatment. In: Posnick JC (ed) Orthognathic Surgery. W.B. Saunders, St. Louis, pp 1095–1158. https://doi.org/10.1016/B978-1-4557-2698-1.00028-9
Ascenco AS, Balbinot P, Junior IM, D’Oro U, Busato L, da Silva FR (2014) Mandibular distraction in hemifacial microsomia is not a permanent treatment: a long-term evaluation. J Craniofac Surg 25(2):352–354. https://doi.org/10.1097/01.scs.0000436741.90536.bf
Fattah AY, Caro C, Khechoyan DY, Tompson B, Forrest CR, Phillips JH (2014) Cephalometric outcomes of orthognathic surgery in hemifacial microsomia. J Craniofac Surg 25(5):1734–1739. https://doi.org/10.1097/scs.0000435808.91512.58
Ko EW, Chen PK, Lo LJ (2017) Comparison of the adult three-dimensional craniofacial features of patients with unilateral craniofacial microsomia with and without early mandible distraction. Int J Oral Maxillofac Surg 46(7):811–818. https://doi.org/10.1016/j.ijom.2017.03.002
Yamaguchi K, Lonic D, Ko EW, Lo LJ (2017) An integrated surgical protocol for adult patients with hemifacial microsomia: methods and outcome. PLoS ONE 12(8):e0177223. https://doi.org/10.1371/journal.pone.0177223
Suppapinyaroj C, Lin CH, Lo LJ, Ko EW (2021) Outcome of surgical-orthodontic treatment in hemifacial microsomia with and without early mandibular distraction osteogenesis. Int J Oral Maxillofac Surg 50(6):763–773. https://doi.org/10.1016/j.ijom.2020.10.007
Luo E, Yang S, Du W, Chen Q, Liao C, Fei W, Hu J (2016) Bimaxillary orthognathic approach to correct skeletal facial asymmetry of hemifacial microsomia in adults. Aesthetic Plast Surg 40(3):400–409. https://doi.org/10.1007/s00266-015-0590-9
Wang P, Wang Y, Zhang Z, Li X, Ye B, Li J (2018) Comprehensive consideration and design with the virtual surgical planning-assisted treatment for hemifacial microsomia in adult patients. J Craniomaxillofac Surg 46(8):1268–1274. https://doi.org/10.1016/j.jcms.2018.05.004
Chen YF, Liao YF, Chen YA, Chen YR (2019) Surgical-orthodontic treatment for class II asymmetry: outcome and influencing factors. Sci Rep 9(1):17956. https://doi.org/10.1038/s41598-019-54317-5
Chen YF, Liao YF, Chen YA, Chen YR (2019) Treatment outcome of bimaxillary surgery for asymmetric skeletal class II deformity. Clin Oral Investig 23(2):623–632. https://doi.org/10.1007/s00784-018-2462-6
Xi T, Schreurs R, Heerink WJ, Berge SJ, Maal TJ (2014) A novel region-growing based semi-automatic segmentation protocol for three-dimensional condylar reconstruction using cone beam computed tomography (CBCT). PLoS ONE 9(11):e111126. https://doi.org/10.1371/journal.pone.0111126
Swennen GR, Schutyser F, Barth EL, De Groeve P, De Mey A (2006) A new method of 3-D cephalometry Part I: the anatomic Cartesian 3-D reference system. J Craniofac Surg 17(2):314–325. https://doi.org/10.1097/00001665-200603000-00019
Chen YF, Vinayahalingam S, Bergé S, Liao YF, Maal T, Xi T (2021) Three-dimensional analysis of the condylar hypoplasia and facial asymmetry in craniofacial microsomia using cone-beam computed tomography. J Oral Maxillofac Surg:1750.e1751–1750.e1710. https://doi.org/10.1016/j.joms.2021.03.015
Chen YF, Baan F, Bruggink R, Bronkhorst E, Liao YF, Ongkosuwito E (2020) Three-dimensional characterization of mandibular asymmetry in craniofacial microsomia. Clin Oral Investig 24(12):4363–4372. https://doi.org/10.1007/s00784-020-03302-8
Kim EJ, Palomo JM, Kim SS, Lim HJ, Lee KM, Hwang HS (2011) Maxillofacial characteristics affecting chin deviation between mandibular retrusion and prognathism patients. Angle Orthod 81(6):988–993. https://doi.org/10.2319/112210-681.1
Baek SH, Cho IS, Chang YI, Kim MJ (2007) Skeletodental factors affecting chin point deviation in female patients with class III malocclusion and facial asymmetry: a three-dimensional analysis using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104(5):628–639. https://doi.org/10.1016/j.tripleo.2007.03.002
Hirschfelder U, Piechot E, Schulte M, Leher A (2004) Abnormalities of the TMJ and the musculature in the oculo-auriculo-vertebral spectrum (OAV). A CT study J Orofac Orthop 65(3):204–216. https://doi.org/10.1007/s00056-004-0331-1
Kwon TG, Park HS, Ryoo HM, Lee SH (2006) A comparison of craniofacial morphology in patients with and without facial asymmetry–a three-dimensional analysis with computed tomography. Int J Oral Maxillofac Surg 35(1):43–48. https://doi.org/10.1016/j.ijom.2005.04.006
Shibazaki-Yorozuya R, Yamada A, Nagata S, Ueda K, Miller AJ, Maki K (2014) Three-dimensional longitudinal changes in craniofacial growth in untreated hemifacial microsomia patients with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 145(5):579–594. https://doi.org/10.1016/j.ajodo.2013.09.015
Thiesen G, Gribel BF, Freitas MPM, Oliver DR, Kim KB (2017) Craniofacial features affecting mandibular asymmetries in skeletal Class II patients. J Orofac Orthop 78(5):437–445. https://doi.org/10.1007/s00056-017-0100-6
Igelbrink S, Zanettini LMS, Bohner L, Kleinheinz J, Jung S (2020) Three-dimensional planning of the mandibular margin in hemifacial microsomia using a printed patient-specific implant. J Craniofac Surg 31(8):2297–2301. https://doi.org/10.1097/scs.0000000000007039
Jo H, Ohe JY, Lee JW, Lee BS, Jung J (2021) Posterior bending osteotomy: an effective measure to secure facial symmetry in orthognathic surgery. J Craniomaxillofac Surg 49(7):538–544. https://doi.org/10.1016/j.jcms.2021.01.021
Chew MT (2006) Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod 76(5):806–809. https://doi.org/10.1043/0003-3219(2006)076[0806:Samodd]2.0.Co;2
Funding
The work was supported by the Chang Gung Memorial Hospital, Taiwan (CMRPG1K0171).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Board and Medical Ethics Committee at Chang Gung Memorial Hospital, Taoyuan, Taiwan (201901347B0).
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, YF., Vinayahalingam, S., Bergé, S. et al. Is the pattern of mandibular asymmetry in mild craniofacial microsomia comparable to non-syndromic class II asymmetry?. Clin Oral Invest 26, 4603–4613 (2022). https://doi.org/10.1007/s00784-022-04429-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04429-6