Abstract
Objectives
This retrospective study was aimed to compare the clinical and radiographic outcomes of implants with the same body design but different collar surface (laser-microtextured vs. not laser-microtextured) after functional loading.
Materials and methods
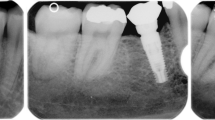
Forty-three patients (29 females, 14 males) with 139 implants (60 laser-microtextured and 79 without laser microtexturing) were included in this study. Patients were consecutively included, and the data were collected during their implant maintenance visit. Clinical and radiographic parameters including probing depth (PD), bleeding on probing (BoP), and marginal bone loss (MBL) were recorded. In addition, the implant success index (ISI) score was determined. Statistical analysis was performed using the Mann–Whitney U test, the Kruskal–Wallis rank test, or the Pearson χ2 test, along with binary logistic regression (p < 0.05 was considered to be statistically significant).
Results
The median post-loading follow-up was 24 months with 100% survival rate. There was no significant differences in terms of mean PD (3.01 mm vs. 2.63 mm), mean MBL (0.54 vs. 0.49 mm), BoP (56.7% vs. 53.2%), and ISI score between laser-microtextured collars and implants without laser microtexturing. Logistic regression revealed arch as a significant predictor of peri-implantitis (p = 0.02).
Conclusion
Within the limitations of this study, there was no statistically significant difference between the clinical and radiographic outcomes of implants with laser-microtextured and non-laser-microtextured collar designs.
Clinical relevance
Prospective studies with larger sample sizes and careful monitoring of implant placement protocols are needed for definite conclusions.


Similar content being viewed by others
References
Kotsakis GA (2000) Olmedo DG (2021) Peri-implantitis is not periodontitis: scientific discoveries shed light on microbiome-biomaterial interactions that may determine disease phenotype. Periodontol 86(1):231–240. https://doi.org/10.1111/prd.12372
Suarez-Lopez Del Amo F, Lin GH, Monje A, Galindo-Moreno P, Wang HL (2016) Influence of soft tissue thickness on peri-implant marginal bone loss: a systematic review and meta-analysis. J Periodontol 87(6):690–699. https://doi.org/10.1902/jop.2016.150571
de Brandao ML, Vettore MV, Vidigal Junior GM (2013) Peri-implant bone loss in cement- and screw-retained prostheses: systematic review and meta-analysis. J Clin Periodontol 40(3):287–295. https://doi.org/10.1111/jcpe.12041
Koutouzis T (2000) (2019) Implant-abutment connection as contributing factor to peri-implant diseases. Periodontol 81(1):152–166. https://doi.org/10.1111/prd
Bonfante EA, Jimbo R, Witek L, Tovar N, Neiva R, Torroni A et al (2000) (2019) Biomaterial and biomechanical considerations to prevent risks in implant therapy. Periodontol 81(1):139–151. https://doi.org/10.1111/prd.12288
Monje A, Galindo-Moreno P, Tozum TF, Suarez-Lopez del Amo F, Wang HL (2016) Into the paradigm of local factors as contributors for peri-implant disease: short communication. Int J Oral Maxillofac Implants 31(2):288–292. https://doi.org/10.11607/jomi.4265
Schwarz F, Hegewald A, Becker J (2014) Impact of implant-abutment connection and positioning of the machined collar/microgap on crestal bone level changes: a systematic review. Clin Oral Implants Res 25(4):417–425. https://doi.org/10.1111/clr.12215
Sykaras N, Iacopino AM, Marker VA, Triplett RG, Woody RD (2000) Implant materials, designs, and surface topographies: their effect on osseointegration. A literature review. Int J Oral Maxillofac Implants 15(5):675–690
Zhao G, Schwartz Z, Wieland M, Rupp F, Geis-Gerstorfer J, Cochran DL, Boyan BD (2005) High surface energy enhances cell response to titanium substrate microstructure. J Biomed Mater Res A 74(1):49–58. https://doi.org/10.1002/jbm.a.30320
Guerra F, Wagner W, Wiltfang J, Rocha S, Moergel M, Behrens E, Nicolau P (2014) Platform switch versus platform match in the posterior mandible-1-year results of a multicentre randomized clinical trial. J Clin Periodontol 41(5):521–529. https://doi.org/10.1111/jcpe.12244
Nevins M, Camelo M, Nevins ML, Schupbach P, Kim DM (2012) Connective tissue attachment to laser-microgrooved abutments: a human histologic case report. Int J Periodontics Restorative Dent 32(4):385–392
Alomrani AN, Hermann JS, Jones AA, Buser D, Schoolfield J, Cochran DL (2005) The effect of a machined collar on coronal hard tissue around titanium implants: a radiographic study in the canine mandible. Int J Oral Maxillofac Implants 20(5):677–686
Stein AE, McGlmphy EA, Johnston WM, Larsen PE (2009) Effects of implant design and surface roughness on crestal bone and soft tissue levels in the esthetic zone. Int J Oral Maxillofac Implants 24(5):910–919
Valderrama P, Jones AA, Wilson TG Jr, Higginbottom F, Schoolfield JD, Jung RE, Noujeim M, Cochran DL (2010) Bone changes around early loaded chemically modified sandblasted and acid-etched surfaced implants with and without a machined collar: a radiographic and resonance frequency analysis in the canine mandible. Int J Oral Maxillofac Implants 25(3):548–557
Schwarz F, Messias A, Sanz-Sanchez I, Carrillo de Albornoz A, Nicolau P, Taylor T, Beuer F (2019) Influence of implant neck and abutment characteristics on peri-implant tissue health and stability. Oral reconstruction foundation consensus report. Clin Oral Impl Res 30(6):588–593. https://doi.org/10.1111/clr.13439
Carrigy J, Sharma A, Perrotti V, Quaranta A (2021) Clinical outcomes of laser microtextured implants or abutments: a systematic review. Int J Oral Implantol (Berl) 14(2):141–154
Messias A, Nicolau P, Guerra F (2019) Titanium dental implants with different collar design and surface modifications: a systematic review on survival rates and marginal bone levels. Clin Oral Implants Res 30(1):20–48. https://doi.org/10.1111/clr.13389
Nevins M, Nevins ML, Camelo M, Boyesen JL, Kim DM (2008) Human histologic evidence of a connective tissue attachment to a dental implant. Int J Periodontics Restorative Dent 28(2):111–121
Shapoff CA, Lahey B, Wasserlauf PA, Kim DM (2010) Radiographic analysis of crestal bone levels around Laser-Lok collar dental implants. Int J Periodontics Restorative Dent 30(2):129–137
Small PN, Tarnow DP (2000) Gingival recession around implants: a 1-year longitudinal prospective study. Int J Oral Maxillofac Implants 15(4):527–532
Chen ST, Beagle J, Jensen SS, Chiapasco M, Darby I (2009) Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants 24(Suppl):272–278
Kadkhodazadeh M, Amid R (2012) Evaluation of peri-implant tissue health using a scoring system. JIACD 4:51–57
Furhauser R, Florescu D, Benesch T, Haas R, Mailath G, Watzek G (2005) Evaluation of soft tissue around single-tooth implant crowns: the pink esthetic score. Clin Oral Implants Res 16(6):639–644. https://doi.org/10.1111/j.1600-0501.2005.01193.x
Belser UC, Grutter L, Vailati F, Bornstein M, Weber H, Buser D (2009) Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol 80(1):140–151. https://doi.org/10.1902/jop.2009.080435
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM et al (2018) Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89(Suppl 1):S313-s318. https://doi.org/10.1002/jper.17-0739
Renvert S, Persson GR, Pirih FQ, Camargo PM (2018) Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol 89(Suppl 1):S304–S312. https://doi.org/10.1002/JPER.17-0588
Guarnieri R, Grande M, Zuffetti F, Testori T (2018) Incidence of peri-implant diseases on implants with and without laser-microgrooved collar: a 5-year retrospective study carried out in private practice patients. Int J Oral Maxillofac Implants 33(2):457–465
Randall EF, Abou-Arraj RV, Geurs N, Griffin R, Reddy M, Geisinger M (2019) The effect of dental implant collar design on crestal bone loss at 1 year after implant placement. Int J Periodontics Restorative Dent 39(2):165–173. https://doi.org/10.11607/prd.3516
Rath SK, Kosala M, Gupta A (2017) Comparative evaluation of laser-microtextured implant versus machined collar implant for soft and hard tissue attachment: a clinical and radiological study. Indian J Dent Res 28(3):298–303. https://doi.org/10.4103/ijdr.IJDR_578_15
Martins de Barros RR, Provinciatti MM, Muglia VA, Novaes AB Jr. (2021) The effect of Laser-Lok abutments on fiber orientation and buccal bone remodeling: a histomorphometric study. Int J Periodontics Restorative Dent 40(1):73–81
Mendonca JA, Senna PM, Francischone CE, Francischone Junior CE, de Souza Picorelli Assis NM, Sotto-Maior BS (2017) Retrospective evaluation of the influence of the collar surface topography on peri-implant bone preservation. Int J Oral Maxillofac Implants 32(4):858–863. https://doi.org/10.11607/jomi.4094
Vazquez Alvarez R, Perez Sayans M, Gayoso Diz P, Garcia Garcia A (2015) Factors affecting peri-implant bone loss: a post-five-year retrospective study. Clin Oral Implants Res 26(9):1006–1014. https://doi.org/10.1111/clr.12416
Linkevicius T, Apse P, Grybauskas S, Puisys A (2010) Influence of thin mucosal tissues on crestal bone stability around implants with platform switching: a 1-year pilot study. J Oral Maxillofac Surg 68(9):222272–222277. https://doi.org/10.1016/j.joms.2009.08.018
Pjetursson BE, Helbling C, Weber HP, Matuliene G, Salvi GE, Bragger U, Schmidlin K, Zwahlen M, Lang NP (2012) Peri-implantitis susceptibility as it relates to periodontal therapy and supportive care. Clin Oral Implants Res 23(7):888–894. https://doi.org/10.1111/j.1600-0501.2012.02474.x
Schwarz F, Derks J, Monje A, Wang HL (2018) Peri-implantitis. J Periodontol 89(Suppl 1):S267-s290. https://doi.org/10.1002/jper.16-0350
Serino G, Strom C (2009) Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res 20(2):169–174. https://doi.org/10.1111/j.1600-0501.2008.01627.x
Heitz-Mayfield LJA, Heitz F, Lang NP (2020) Implant Disease Risk Assessment IDRA-a tool for preventing peri-implant disease. Clin Oral Implants Res 31(4):397–403. https://doi.org/10.1111/clr.13585
Karlsson K, Derks J (2019) Interventions for peri-implantitis and their effects on further bone loss: a retrospective analysis of a registry-based cohort. J Clin Periodontol 46(8):872–879. https://doi.org/10.1111/jcpe.13129
Taylor D, Hazenberg JG, Lee TC (2007) Living with cracks: damage and repair in human bone. Nat Mater 6(4):263–268. https://doi.org/10.1038/nmat1866
Tonetti MS, Cortellini P, Graziani F, Cairo F, Lang NP, Abundo R et al (2017) Immediate versus delayed implant placement after anterior single tooth extraction: the timing randomized controlled clinical trial. J Clin Periodontol 44(2):215–224. https://doi.org/10.1111/jcpe.12666
Bassir SH, El Kholy K, Chen CY, Lee KH, Intini G (2019) Outcome of early dental implant placement versus other dental implant placement protocols: a systematic review and meta-analysis. J Periodontol 90(5):493–506. https://doi.org/10.1002/JPER.18-0338
Serino G, Turri A, Lang NP (2013) Probing at implants with peri-implantitis and its relation to clinical peri-implant bone loss. Clin Oral Implants Res 24(1):91–95. https://doi.org/10.1111/j.1600-0501.2012.02470.x
Mombelli A, Muhle T, Bragger U, Lang NP, Burgin WB (1997) Comparison of periodontal and peri-implant probing by depth-force pattern analysis. Clin Oral Implants Res 8(6):448–454. https://doi.org/10.1034/j.1600-0501.1997.080602.x
Grondahl K, Lekholm U (1997) The predictive value of radiographic diagnosis of implant instability. Int J Oral Maxillofac Implants 12(1):59–64
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed were in accordance with the 1964 Helsinki declaration following approval by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.DRC.REC.1399.122).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kadkhodazadeh, M., Amid, R. & Moscowchi, A. Impact of collar laser microtexturing on peri-implant health and disease: a retrospective clinical study. Clin Oral Invest 26, 1637–1645 (2022). https://doi.org/10.1007/s00784-021-04136-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04136-8