Abstract
Objectives
This follow-up study aimed to report the 24- and 30-month outcomes of a cohort previously enrolled in a randomized clinical trial on surgical reconstructive treatment of peri-implantitis.
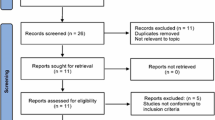
Methods
Twenty-four patients were diagnosed with peri-implantitis and treated with surgical reconstructive therapy with or without the adjunctive use of Er:YAG laser. Within-group and between-group comparisons were tested with mixed model with repeated measures.
Results
Regarding peri-implant pocket depth (PPD) reduction (control vs. laser test group) between 6 months (− 1.85 vs. − 2.65 mm) and 30 months (− 1.84 vs. − 3.04 mm), the laser group showed statistically significant changes but not the control group. In terms of radiographic marginal bone loss (RMBL) at 6 months (− 1.1 vs. − 1.46 mm) to 24 months (− 1.96 vs. − 2.82 mm), both groups showed statistical difference compared to baseline. The six explanted implants all were featured by severe peri-implantitis and mostly with no or limited keratinized tissue (< 2 mm) at baseline and membrane exposure after surgery. Among the 15 retained cases, eight cases achieved more than 50% peri-implant bone level gain.
Conclusions
Within the limitation and follow-up time frame of this trial, the outcome of the surgical reconstructive therapy sustained or improved in most of the cases. However, 25% of the implants with severe peri-implantitis failed 2 years after the surgical reconstructive therapy. The use of Er:YAG laser favors PPD reduction in the longer term up to 30 months.
Clinical relevance
Longer-term follow-up on reconstructive therapy of peri-implantitis revealed sustained or improved stability in certain cases, but the survival of implants with severe peri-implantitis has its limitation, especially when there is limited keratinized tissue (< 2 mm or no KT).
Trial registration
Clinical Trials Registration Number: NCT03127228 and HUM00160290.




Similar content being viewed by others
Data Availability
The demographic information of the extracted implants were included in the supplemental table and other data is available upon request, but the results up to 6 months follow-up was published previously and the data was stated available together with the transcriptomics information [18].
References
Derks J, Schaller D, Håkansson J, Wennström JL, Tomasi C, Berglundh T (2016) Effectiveness of implant therapy analyzed in a Swedish population: prevalence of peri-implantitis. J Dent Res 95:43–49. https://doi.org/10.1177/0022034515608832
Chan HL, Lin GH, Suarez F, MacEachern M, Wang HL (2014) Surgical management of peri-implantitis: a systematic review and meta-analysis of treatment outcomes. J Periodontol 85:1027–1041. https://doi.org/10.1902/jop.2013.130563
Di Gianfilippo R, Sirinirund B, Rodriguez MV, Chen Z, Wang H-L (2020) Long-term prognosis of peri-implantitis treatment: a systematic review of prospective trials with more than 3 years of follow-up. Appl Sci 10:9084
Wang CW, Renvert S, Wang HL (2019) Nonsurgical treatment of periimplantitis. Implant Dent 28:155–160. https://doi.org/10.1097/id.0000000000000846
Schwarz F, Jepsen S, Obreja K, Galarraga-Vinueza ME, Ramanauskaite A (2022) Surgical therapy of peri-implantitis. Periodontol 2000(88):145–181. https://doi.org/10.1111/prd.12417
Renvert S, Lindahl C, Persson GR (2018) Occurrence of cases with peri-implant mucositis or peri-implantitis in a 21–26 years follow-up study. J Clin Periodontol 45:233–240. https://doi.org/10.1111/jcpe.12822
Carcuac O, Derks J, Abrahamsson I, Wennström JL, Berglundh T (2020) Risk for recurrence of disease following surgical therapy of peri-implantitis—a prospective longitudinal study. Clin Oral Implants Res 31:1072–1077. https://doi.org/10.1111/clr.13653
Clem D, Gunsolley JC (2019) Peri-implantitis treatment using Er:YAG laser and bone grafting. A prospective consecutive case series evaluation: 1 year posttherapy. Int J Periodontics Restorative Dent 39:479–489. https://doi.org/10.11607/prd.4158
Yamamoto A, Kubota T, Komatsu Y, Nohno K, Yasuda T, Takahashi T, Torikata R, Tsumori N, Shibutani T, Umeda M, Yoshie H (2021) Efficacy of erbium:YAG laser for regenerative surgical treatment of peri-implantitis: clinical, microbiological, and biomarker analyses. Int J Periodontics Restorative Dent 41:187–192. https://doi.org/10.11607/prd.4071
Schwarz F, John G, Schmucker A, Sahm N, Becker J (2017) Combined surgical therapy of advanced peri-implantitis evaluating two methods of surface decontamination: a 7-year follow-up observation. J Clin Periodontol 44:337–342. https://doi.org/10.1111/jcpe.12648
Tomasi C, Regidor E, Ortiz-Vigón A, Derks J (2019) Efficacy of reconstructive surgical therapy at peri-implantitis-related bone defects. A systematic review and meta-analysis. J Clin Periodontol 46(Suppl 21):340–356. https://doi.org/10.1111/jcpe.13070
Roccuzzo M, Layton DM, Roccuzzo A, Heitz-Mayfield LJ (2018) Clinical outcomes of peri-implantitis treatment and supportive care: a systematic review. Clin Oral Implants Res 29(Suppl 16):331–350. https://doi.org/10.1111/clr.13287
Zipprich H, Weigl P, Di Gianfilippo R, Steigmann L, Henrich D, Wang HL, Schlee M, Ratka C (2022) Comparison of decontamination efficacy of two electrolyte cleaning methods to diode laser, plasma, and air-abrasive devices. Clin Oral Investig 26:4549–4558. https://doi.org/10.1007/s00784-022-04421-0
Nevins M, Nevins ML, Yamamoto A, Yoshino T, Ono Y, Wang CW, Kim DM (2014) Use of Er:YAG laser to decontaminate infected dental implant surface in preparation for reestablishment of bone-to-implant contact. Int J Periodontics Restorative Dent 34:461–466. https://doi.org/10.11607/prd.2192
Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, Romanos GE, Taniguchi Y, Sasaki KM, Zeredo JL, Koshy G, Coluzzi DJ, White JM, Abiko Y, Ishikawa I, Izumi Y (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000 68:217–69. https://doi.org/10.1111/prd.12080
Schwarz F, Sahm N, Iglhaut G, Becker J (2011) Impact of the method of surface debridement and decontamination on the clinical outcome following combined surgical therapy of peri-implantitis: a randomized controlled clinical study. J Clin Periodontol 38:276–284. https://doi.org/10.1111/j.1600-051X.2010.01690.x
Schwarz F, John G, Mainusch S, Sahm N, Becker J (2012) Combined surgical therapy of peri-implantitis evaluating two methods of surface debridement and decontamination. A two-year clinical follow up report. J Clin Periodontol 39:789–797. https://doi.org/10.1111/j.1600-051X.2012.01867.x
Wang CW, Ashnagar S, Gianfilippo RD, Arnett M, Kinney J, Wang HL (2021) Laser-assisted regenerative surgical therapy for peri-implantitis: a randomized controlled clinical trial. J Periodontol 92:378–388. https://doi.org/10.1002/jper.20-0040
Pfefferbaum B, North CS (2020) Mental health and the Covid-19 pandemic. N Engl J Med 383:510–512. https://doi.org/10.1056/NEJMp2008017
Ravidà A, Siqueira R, Di Gianfilippo R, Kaur G, Giannobile A, Galindo-Moreno P, Wang CW, Wang HL (2022) Prognostic factors associated with implant loss, disease progression or favorable outcomes after peri-implantitis surgical therapy. Clin Implant Dent Relat Res 24:222–232. https://doi.org/10.1111/cid.13074
Isehed C, Svenson B, Lundberg P, Holmlund A (2018) Surgical treatment of peri-implantitis using enamel matrix derivative, an RCT: 3- and 5-year follow-up. J Clin Periodontol 45:744–753. https://doi.org/10.1111/jcpe.12894
Brian Z, Weintraub JA (2020) Oral health and COVID-19: increasing the need for prevention and access. Prev Chronic Dis 17:E82. https://doi.org/10.5888/pcd17.200266
Hashim D, Cionca N, Combescure C, Mombelli A (2018) The diagnosis of peri-implantitis: a systematic review on the predictive value of bleeding on probing. Clin Oral Implants Res 29(Suppl 16):276–293. https://doi.org/10.1111/clr.13127
Dukka H, Saleh MHA, Ravidà A, Greenwell H, Wang HL (2021) Is bleeding on probing a reliable clinical indicator of peri-implant diseases? J Periodontol 92:1669–1674. https://doi.org/10.1002/jper.20-0890
Di Gianfilippo R, Askar H, Henderson J, Franceschi D, Wang HL, Wang CW (2021) Intra- and inter-examiner repeatability of diagnostic peri-implant clinical measurement: a pilot study. J Oral Implantol. https://doi.org/10.1563/aaid-joi-D-20-00160
Funding
This follow-up study was supported by research grant from J. Morita (Tokyo, Japan) through the University of Michigan as well as from the Department of Periodontics and Oral Medicine Clinical Research Fund. Manuscript preparation is supported by the Taipei Medical University Research Fund (TMU110-AE1-B27) and the National Science and Technology Council, Taiwan R.O.C. (grant number: NSTC111-2314-B-038–162 to C.W.W.).
Author information
Authors and Affiliations
Contributions
CWW contributed to study conception, design, performing surgeries, data analysis, drafting of the article. RD contributed to manage study visits, data analysis, drafting of the article. AO contributed to project administration and manage study visits. NK contributed to data analysis. SWF contributed to critical review of the manuscript. HLW contributed to study conception, performing surgeries, and critical review of the article.
Corresponding author
Ethics declarations
Conflict of interest
Dr. HL Wang has occasionally spoken on behalf of J. Morita and received honoraria for lectures. The other authors do not have any financial interests, either directly or indirectly, in the products or information listed in the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, CW., Di Gianfilippo, R., Kaciroti, N. et al. Stability of peri-implantitis surgical reconstructive therapy—a (> 2 years) follow-up of a randomized clinical trial. Clin Oral Invest 28, 30 (2024). https://doi.org/10.1007/s00784-023-05457-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00784-023-05457-6